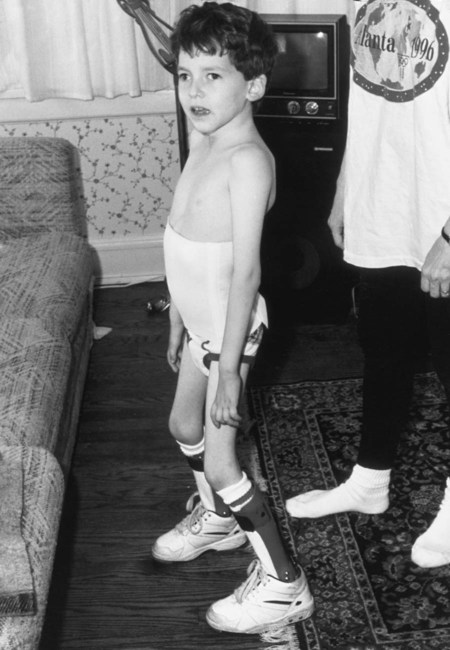
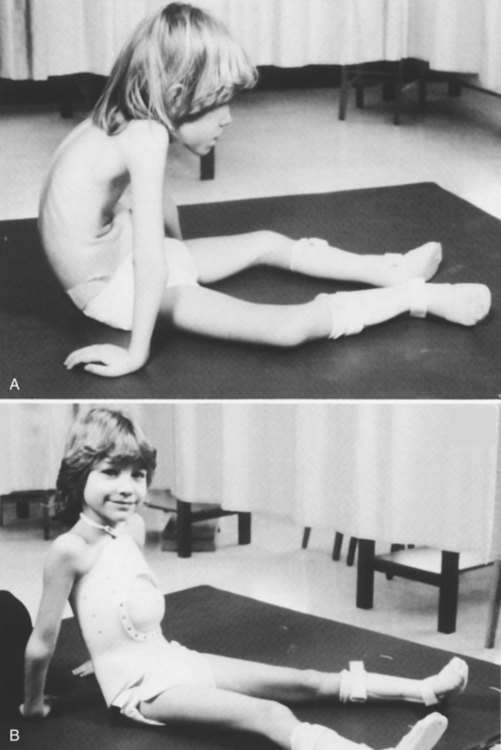
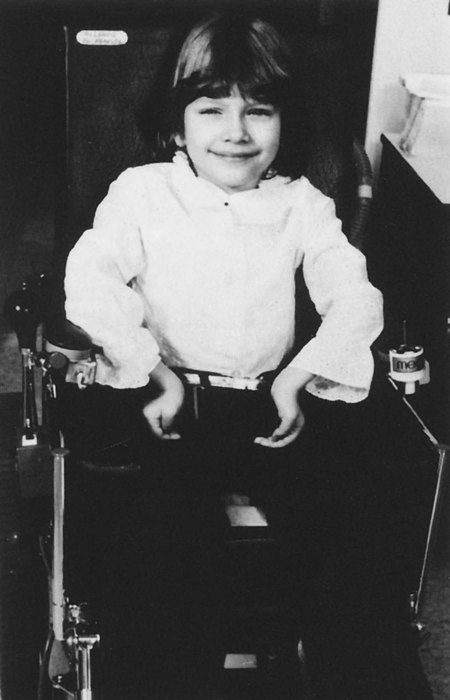
Individuals with breathing impairments (whether primary or secondary in origin) require a variety of interventions to optimize ventilation and oxygen delivery, as well as improving functional outcomes. Some interventions are passive in nature, such as the positioning of the patient or the application of an abdominal binder for better diaphragmatic positioning. Other interventions require very active participation on the part of the therapist, patient, or both, such as in assisted-cough techniques, in glossopharyngeal breathing instruction, or in learning a more efficient breathing pattern. Ideally techniques are incorporated into the patient’s total physical rehabilitation program, such as the use of ventilation strategies pairing breathing with movement. All of these diverse aspects of treatment play an important role in the development of a successful rehabilitation program to meet the needs of patients with pulmonary impairments. No single intervention or approach is appropriate in all cases. Sound clinical judgment and experience must be exercised when applying these ideas in each person. The interventions identified in this chapter are not inclusive. They are meant to provide examples and guidelines and to stimulate the clinician’s creative talents in order to incorporate the interventions into a comprehensive treatment program determined by individual needs that improve the outcomes for each patient (Box 23-1). All patients spend some portion of the day in a horizontal position for rest or sleep. Some who are acutely ill or medically compromised spent extended time in bed, and major emphasis must be placed on the mobilization of patients early and often to prevent immobility from exerting its negative effects on all body systems (see Chapter 18). Studies have shown that patients who are medicated and spend extended time on ventilators in the ICU have developed critical illness neuromuscular syndrome or ICU-acquired weakness. Interventions shown to help prevent this problem are physical therapy/activity and daily interruptions of sedative medication.1,2,3 These studies validate the need for intervention to prevent untoward effects of immobility and sedation. Despite these problems, the time spent in a horizontal position can be used as an opportunity to assist patients in passive drainage and preventing the retention of lung secretions. It can be a natural beginning in the development of a patient’s long-term respiratory program (e.g., the prevention of respiratory complications in a patient with tetraplegia). Specific postural drainage positions are covered under airway clearance interventions (see Chapter 21). Using a combination of these positions and the patient’s position in bed, in the hospital or at home, can help to achieve multiple goals. First, various horizontal positions can assist patients in passively clearing secretions that they may have difficulty clearing actively. Pneumonia is still the leading cause of death in patients with spinal cord injury (SCI) who are tetraplegic.4 Second, these position changes provide for skin relief and better circulation. Finally, they assist in retarding the development of joint contractures or other musculoskeletal abnormalities. A four-position rotation (i.e., supine, prone, and side-to-side) or a modified six-position rotation (supine, three-quarter supine, side-lying, three-quarter prone on each side) is usually an effective and reasonable means of incorporating these goals into a long-term prophylactic program. Simple adaptations may make ventilation easier in each of these postures. For example, when the patient is in the supine position, placing the patient’s arms up over his or her head facilitates greater anterior upper chest expansion.5 Likewise, positioning the pelvis in a slight posterior tilt facilitates more diaphragmatic excursion. (Detailed explanations of positioning are discussed in Chapter 42.) Observation of all precautions and contraindications to passive positioning is still warranted, and positions should be modified based on the individual need of each patient. Just as passive positioning of the patient in bed helps to maintain airway clearance and improve ventilation potential, optimal passive positioning of the patient’s skeletal frame in an upright posture (sitting, standing) helps to maximize the mechanical advantages that facilitate breathing and improve cardiovascular fluid shifts. For example, patients with SCIs resulting in tetraplegia will be unable to support their intestinal contents properly under the diaphragm to allow for maximal expansion of the chest in all three planes of ventilation (see Chapter 39). The use of an abdominal support from the iliac crest to the base of the xiphoid process provides positive-pressure support to restore intestinal positioning to an upright position (Figure 23-1). Research has documented well the significant improvements in vital capacity (VC), inspiratory capacity, and tidal volume (TV) in sitting with the use of a strong abdominal support.6 These binders have also been used in nursing care to provide for better circulation and the prevention of hypotension. A rigid type of abdominal support can be used when the vertebral column and the abdominal viscera need support. These are called body jackets or total contact thoracic lumbar sacral orthoses (TLSOs) (Figure 23-2). A TLSO is a rigid trunk support molded individually to the shape of the patient’s entire trunk from the axilla down to the pubis. It is composed of two separate pieces, a front and a back, ideally with an anterior cutout in the abdomen to allow for normal diaphragmatic displacement of the viscera. In addition to these jackets, an elastic binder is applied around the abdomen to allow for diaphragmatic motion but minimize excessive displacement of the abdominal contents. This is particularly appropriate for a growing child who needs more spinal stability and for the completely flaccid patient with tetraplegia, who may also require the same support. Because head and neck positioning are so dependent on trunk positioning, a body jacket may make the difference for these patients between being dependent or independent in an upright posture. It may result in significantly better head control and eye contact and improved phonation. However, because the TLSO limits trunk movement, its usefulness for each patient must be assessed carefully. The next consideration in passive respiratory techniques is proper wheelchair positioning. Optimal performance in ventilatory functioning, as well as many other areas of rehabilitation, depends on good alignment of the body against the force of gravity. Symmetry must be strived for through the use of a body jacket, lateral trunk supports in the wheelchair, abdominal binders, or some other means (Figure 23-3). This is especially important for patients with hemiplegia in whom habitual asymmetrical posturing leads to musculoskeletal problems later. Symmetrical breathing patterns and uniform aeration of all lung segments are augmented by careful upright positioning. Therefore everything from the type of neck and trunk support to the height and width of the arm rests to the length and type of the foot supports must be carefully analyzed for each patient. The patient is first positioned for successful ventilation. Then motor activities should be introduced. Interventions chosen will improve the patient’s ventilatory support, or the therapist should capitalize on the patient’s good ventilatory support to improve the motor activity. Using ventilatory strategies to improve motor performance or movement strategies to improve ventilation performance enables patients to achieve their functional goals sooner and have better health, including fewer respiratory complications. Generally, these simple concepts take no more than 1 to 2 additional minutes of therapy time, with no additional equipment costs other than a few extra pillows or towels. Therefore time and money are not mitigating factors. However, these ideas do require the practitioner to look carefully at the patient before beginning any treatment intervention and to ask, “Have I positioned my patient for ventilatory success?”; “Am I simply treating the patient in whatever position I found her or him in?”; and “Have I carefully chosen my verbal cues to include a ventilatory response and a functional response?” The practitioner must actively include ventilation in every activity to help the patient understand that breathing transcends all activities. Breathing is the bridge to function. A summary of the most important ventilation-movement strategies is listed in Box 23-2. After the patient has been carefully positioned for respiratory success, as described previously, begin the patient’s therapy or daily-living activities. In a study looking at rhythmic pronation and supination wrist movements, inspiration and exhalation adapted and became coordinated with the arm movement (Table 23-1).7,8 Accordingly, then, the simple task of passive range of movement (ROM) can easily include the active goal of increasing ventilation by asking the patient to breathe in and look up when his or her arm is raised up into shoulder flexion. This encourages the patient to breathe in when the chest wall muscles are being stretched and the ribs are naturally opening up, causing both activities to be more successful. It also begins to teach the patient to use ventilatory strategies to optimize potential functional movement, such as in reaching up to a kitchen cabinet. Patients need to focus on avoiding breath holding and incorporating breathing during each activity. Table 23-1 Anatomy of Inspiration and Expiration Thus the therapist may ask the patient to slowly count out loud to 10 while the arm is being returned eccentrically to his or her side. The patient learns to correlate exhalation with shoulder extension while simultaneously learning a much more complex idea—that of controlling his or her rate and volume of expiration by including deliberate speech during exhalation maneuvers. Research is being done in the area of respiratory plasticity to evaluate changes with exercise and conditioning.9,10 Clinical observation demonstrates that patients will incorporate new ventilation strategies and that these strategies become less cognitive and more based in habit as they are repeated. In a recent study of strategies for respiratory exercise patterns with upper extremity movements in patients with chronic obstructive pulmonary disease (COPD), 15 patients were instructed in the reverse pattern. For example, with shoulder flexion they performed the activity with exhalation versus inhalation. The researchers concluded that there was less chest asynchrony and that it may be an important strategy for people with COPD to use the opposite pattern.11 This study had only 15 patients with COPD; however, it may be noted that with ventilatory strategies, patients may try different ways of incorporating breathing. As long as patients are not breath holding, therapists should feel safe encouraging them to try techniques and see what works best for them. Upper extremity dressing and upper extremity exercise can incorporate the same ideas. All movements should be coordinated with appropriate chest wall movements to maximize upper extremity tasks. Thus every time the arm is moving up above 90 degrees of shoulder flexion, the patient should be asked to breathe in, allowing for the normal shoulder/rib-cage rhythm to occur. Full shoulder flexion requires the opening of the intercostal spacing and the separation of the individual ribs.12 Many patients with neurological impairments have lost the intrinsic mobility of the chest wall and thus may have lost some functional shoulder ROM as well. Not pairing inspiration with shoulder flexion is likely to limit the patient’s shoulder ROM to approximately 140 to 150 degrees. It may also encourage Valsalva maneuvers during the activity and may cause more shoulder pain. Many patients with lung cancer also have COPD, which increases their postoperative complications because of impaired pulmonary function before surgery. In a study of patients with COPD who needed to undergo surgical resection for cancer, it was found that a preoperative pulmonary rehabilitation program of 10 visits over a 4-week period consisting of exercise prescription, inspiratory muscle training, and slow breathing technique improved patients’ postoperative progress. The group in this program required a shorter period of time in the ICU and fewer days using a chest tube. Although this study was done with only nine patients, it has implications for improvement of postoperative success. However, in many cases, it may not be feasible to have 4 weeks of pulmonary rehabilitation before lung surgery. Some surgeons are hesitant to delay the needed surgery for pulmonary rehabilitation. A larger study would need to be conducted to demonstrate cost effectiveness, as well as the benefits and risks.13 Vital capacity is also affected in cases of tetraplegia, in which patients’ vital capacity may be reduced to 1000 to 1500 mL from their normal 3000-mL vital capacity (50%). If the normal TV (normal volume of breathing) is 500 mL, this means that with each breath the patient would use 33% to 50% of his or her vital capacity (maximal inspiration followed by maximal exhalation). This would greatly increase the work of breathing and oxygen consumption just for normal quiet breathing. The patient would have little pulmonary reserve. This can lead to respiratory muscle fatigue. During exercise or stress, the patient would have an increased subjective feeling of shortness of breath and feel an increase in the work of breathing. In addition, patients with spinal cord injury who are smokers experience excessive vital capacity losses.14 Commonly used terms to describe breathing patterns are listed in Box 23-3. A listing of indications for teaching controlled-breathing techniques is provided in Box 23-4. It should be appreciated that breathing comfortably and in a controlled manner is associated with wellness and a sense of ease. Even normal individuals who are under stress and have increased work levels are more cognizant of the increase in their work of breathing. For a patient who struggles with every breath and wonders how it will be possible to get through the day, ventilatory strategies and breathing-control techniques can be the key to maximizing potential. A list of goals for teaching controlled-breathing techniques is found in Box 23-5. Breathing control has long been used in yoga to focus and to promote meditation. This is a key to maximizing rehabilitation. Patients who cannot breathe cannot function! It is of primary importance to assess patients’ breathing at rest and during exercise. People often hold their breath with exertion, especially during new activities, so it is vital to assess the cardiopulmonary and neuromuscular response to each new activity. In many rehabilitation centers and health clubs, Pilates exercise regimens have been used to help patients achieve core strength and back stabilization. Pilates is a method of physical and mental conditioning combined with body, mind, and spirit integration; it has been also used by dancers and choreographers to improve postural control, increase ease of movement, and improve their performance. The first phase of Pilates incorporates diaphragmatic breathing before continuing with the steps to activate the muscles of the core (multifidus, diaphragm, pelvic floor, and transverse abdominis). The belief is that when the individual has a strong core, the posture will improve and the performance of other functional activities will be improved. This is similar to our concept of teaching diaphragmatic breathing control before functional activities in people with respiratory impairments. Joseph Pilates actually used the term contrology to define his concepts. That is what we are striving to teach our patients—breath control, then function.15 Patients with primary lung disease, such as COPD, asthma, bronchitis, or cystic fibrosis, present a picture very different from that of patients with secondary pulmonary deficits, SCI, Parkinson disease, myasthenia gravis, or Guillain-Barré syndrome. In general, patients with primary lung disease tend to overuse their accessory muscles and greatly increase the work of breathing secondary to shortness of breath or coughing. They often complain that they have difficulty “getting the air out,” which demonstrates the decreased expiratory flow rates noted on pulmonary function tests. This can lead to dynamic hyperinflation, in which patients continue to gasp and increase the respiratory rate so more air is coming in, but there is not time for the air to be exhaled. Large volumes of air can get trapped in the lungs, which causes increased feelings of shortness of breath and panic. The goal with these patients is to teach them to relax the neck and chest accessory muscles and use more diaphragmatic breathing (abdominal and lateral costal breathing) to reduce the work of breathing in combination with relaxed pursed-lips breathing and prolonged exhalation. Their treatment programs focus on energy conservation, relaxation, and pacing activity with breath control. In pulmonary rehabilitation programs, exercise is a key component. Patients learn to coordinate their breathing with their activities and find that they have less dyspnea with exertion.16,17 There has been controversy in the literature about the effectiveness of diaphragmatic breathing. No standardized “norms” of how to perform diaphragmatic breathing exist. However, many skilled cardiovascular and pulmonary physical therapists would consider teaching the patient with COPD how to relax the accessory muscles and use the diaphragm as an important part of the patient’s pulmonary rehabilitation. Dechman reported that in a search of the literature, pursed-lips breathing was considered most effective by people with COPD and that the literature does not strongly support the use of diaphragmatic breathing in people with COPD.18 Cahalin found there are both positive and potentially detrimental effects to diaphragmatic breathing training.19 Each individual patient needs to be evaluated to consider whether diaphragmatic breathing may be beneficial. For example, patients with severe hyperinflation and flattened diaphragms secondarily will most likely not benefit from diaphragmatic breathing because the muscle length tension relationship is abnormal and will not result in an appropriate movement of the diaphragm. With patients who have mild to moderate COPD and are overusing the accessory muscles, diaphragmatic breathing may be very helpful; it may require less oxygen consumption, decrease the respiratory rate, and increase the tidal volume. Patients with secondary pulmonary dysfunction, such as SCI, have a more restrictive component to inspiration. In these cases, accessory muscles may be intact, but they are not being used to facilitate deep breathing or coughing. Patients may have strong diaphragmatic breaths, but the upper chest collapses on inspiration (paradoxical breathing; see Chapter 39). The goal is to teach these patients to use the accessory muscles to balance the upper and lower chest. This facilitates an increase in vital capacity that prevents atelectasis and pneumonia by increasing the volume of ventilation and improving the cough mechanism. Pursed-lips breathing is a strategy that is often spontaneously used by people with COPD during episodes of dyspnea. Many patients feel this breathing pattern helps to decrease their breathlessness. The effect of PLB is an increase in the time of exhalation, which results in a decrease in the end-expiratory volume and an increase in the total time of the respiratory cycle. This results in a decreased respiratory rate and increased TV. According to studies, a decrease in the Borg scale of perceived exertion also occurs when PLB is used.20 This technique has been acknowledged by many patients with respiratory impairments as being very easy to learn and yet very effective, quick to use, and readily incorporated into their activities to reduce dyspnea.21 The respiratory action of the diaphragm and other respiratory muscles is normally coordinated with the need to provide postural control of the trunk during movement of the extremities.8 The diaphragm acts both as a muscle of respiration and as a muscle that works in providing core stability to the trunk. However, when respiratory demand increases, the diaphragm may not be able to continue to provide both of these functions.22–27 Because the diaphragm is the primary muscle of respiration, postural control may be impaired. A complete discussion of this concept is provided in Chapter 39. In the initial phases of breathing retraining, patients are taught to use the easiest intervention that facilitates diaphragmatic breathing; if it is not successful, a progression of specific facilitation and inhibition techniques will be tried. A summary of methods of facilitating diaphragmatic ventilation patterns is given in Box 23-6.
Facilitating Ventilation Patterns and Breathing Strategies
Positioning Concerns
Ventilatory and Movement Strategies for Improving Functional Outcomes
Incorporating Simple Therapy Tasks
Inspiration
Inspiration
Expiration
Trunk
Trunk extension
Trunk flexion
Shoulders
Shoulder flexion, abduction, and external rotation movements
Shoulder extension, adduction, and internal rotation movements
Gaze
Upward eye gaze
Downward eye gaze
Exhalation
Dynamic Activities
Dressing
Facilitating a Controlled Diaphragmatic Breathing Pattern
Considerations in Teaching Breathing Control to Patients with Primary Versus Secondary Pulmonary Dysfunction
 Does the patient have more difficulty during inspiration or exhalation?
Does the patient have more difficulty during inspiration or exhalation?
 Is there a normal sequence to inspiration (i.e., abdominal wall rise, then lateral costal expansion, then upper chest expansion, with a full inspiration)? Or does the chest sink and the abdomen rise on inspiration?
Is there a normal sequence to inspiration (i.e., abdominal wall rise, then lateral costal expansion, then upper chest expansion, with a full inspiration)? Or does the chest sink and the abdomen rise on inspiration?
 Does the patient appear to be working hard to breathe? Is the patient using the accessory muscles to an extreme?
Does the patient appear to be working hard to breathe? Is the patient using the accessory muscles to an extreme?
 Does the patient frequently clear the throat, have trouble coughing, or have difficulty speaking at a normal volume and for the normal length of sentences?
Does the patient frequently clear the throat, have trouble coughing, or have difficulty speaking at a normal volume and for the normal length of sentences?
 Is ventilation the limiting factor in accomplishing an activity (e.g., transfer, gait, or bed mobility)?
Is ventilation the limiting factor in accomplishing an activity (e.g., transfer, gait, or bed mobility)?
Pursed-Lips Breathing
Relationship of the Diaphragm and Posture
Facilitating Diaphragmatic Breathing
Facilitating Ventilation Patterns and Breathing Strategies