Patients with first acute myocardial infarction (AMI) constitute a demographic that is exposed to significant amounts of low-dose ionizing radiation (LDIR) over a short period. The aim of this study was to describe cardiac LDIR exposure trends among patients with first AMI over a recent approximately 10-year period. Administrative databases were used to identify a cohort of 106,803 patients who had first AMIs in Quebec, Canada, from 1996 to 2004. These patients were followed through 2007, and the use over time of cardiac imaging procedures associated with LDIR was documented using a cumulative exposure variable. Exposure was documented in 2 periods: the acute phase (<1 month after AMI) and the chronic phase (1 month to 3 years after AMI). The mean dose of cardiac LDIR incurred in the acute post-AMI phase increased twofold during the study period, from 6.8 to 11.8 mSv/patient. However, the mean dose of cardiac LDIR incurred in the chronic post-AMI phase decreased, from 8.3 to 7.3 mSv/patient. Overall, there was a 26.4% increase in cumulative cardiac LDIR exposure, to a mean of 19.1 mSv/patient in the 2 years after AMI, which was driven primarily by an increase in percutaneous coronary interventions. When patients were stratified by cumulative LDIR exposure, several predictors of heavier LDIR exposure were identified among the strata of exposed patients, including younger age and the absence of acute and co-morbid conditions, and the heaviest exposed group subsequently had the lowest overall mortality. In conclusion, among patients experiencing first AMI in Canada, exposure to cardiac LDIR increased over a recent approximately 10-year period. However, the observed trend is toward increasing use of therapeutic procedures with proven mortality benefit undertaken earlier in the disease course and away from diagnostic procedures in the subsequent years after AMI.
With the rapid growth of cardiac imaging and therapeutic procedures, concern has arisen that patients are being exposed to large amounts of low-dose ionizing radiation (LDIR). Studies from atomic bomb survivors and nuclear workers have established the link between LDIR exposure and malignancy. Recently, an association between medical LDIR exposure and incident malignancies has been suggested using data from a large population-based cohort. Survivors of acute myocardial infarction (AMI) represent a potentially high-risk group of patients, because they are exposed to large amounts of radiation over a short period. To our knowledge, there has been only one other attempt to quantify LDIR exposure among these patients, which suggested that most patients receive at least modest exposure. Our objectives were to document the magnitude of this potential risk among a population-based cohort of patients with AMI and to determine how this exposure changed over a approximately 10-year period.
Methods
A longitudinal cohort composed of all patients hospitalized with first AMI in Quebec, Canada, was created by linking the Quebec hospital discharge summary database (which includes information on all hospitalizations) to provincial physicians’ services and drug claims databases. Quebec has a system of universal access to government-provided health care, and hence all inhabitants are included in these databases. Vital status information was obtained from these databases linked to pension, car insurance, and death registry. Linkage was done anonymously using patients’ unique, encrypted health care insurance numbers. Patients with first AMIs from April 1, 1996, to March 31, 2004, were identified using International Classification of Diseases, Ninth Revision (410), and International Classification of Diseases, Tenth Revision (I21 and I22), codes. Patient demographic data were collected for all patients and recoded in categories on the basis of fiscal year of index AMI. Relative risks (RR) and 95% confidence intervals (CIs) were calculated to quantify the changing proportion of patients with medical co-morbidities.
LDIR exposure was measured by recording the number of cardiac imaging and therapeutic procedures undergone by each member of the cohort, who were subsequently categorized by fiscal year of AMI. Exposure to 4 tests of interest was noted, and their respective LDIR doses were estimated from validated estimates: myocardial perfusion imaging (MPI) (15.6 mSv), diagnostic cardiac catheterization without intervention (7 mSv), cardiac catheterization with percutaneous coronary intervention (PCI) (15 mSv), and cardiac rest ventriculography/multiple gated acquisition (MUGA) (7.8 mSv). Exposure was documented in 2 time periods: an acute phase (<1 month after AMI) and a chronic phase (1 month to 3 years after AMI). The proportion of patients exposed to a given test was defined as the percentage of patients receiving ≥1 test during the specified period. In addition, the absolute number of each procedure was multiplied by the estimated LDIR dose for that procedure to define a cumulative exposure variable.
We then identified demographic factors that predicted heavier LDIR exposure by creating exposure categories on the basis of our groups of exposure: 0, 0 to 10, 10 to 20, 20 to 30, and >30 mSv. To avoid the influence of temporal trends in practice patterns, and to provide the most current information, only demographic data from the latest year of the study, 2004, were considered for this purpose. Statistical significance was determined for the interaction between each clinical variable and subsequent exposure to LDIR only within the exposed patients (i.e., excluding the 0-mSv exposure group), because these patients were dramatically demographically different from the other strata and their short-term mortality was much higher, suggesting early in-hospital mortality, which precluded subsequent LDIR exposure. Analyses were performed using SAS (SAS Institute, Inc., Cary, North Carolina).
Results
A total of 106,803 patients who were hospitalized for first AMI from 1996 to 2004 were identified. Patient characteristics stratified by year are listed in Table 1 . During the study period, the median hospital length of stay decreased, and the prevalence of several co-morbidities at the time of presentation increased, including diabetes mellitus (from 20% to 25%; RR 1.25, 95% CI 1.19 to 1.31), chronic kidney disease (from 6% to 14%; RR 2.16, 95% CI 1.98 to 2.35), and arterial hypertension (from 25% to 41%; RR 1.62, 95% CI 1.56 to 1.68). The median age increased from 67.5 to 68.7 years. Thirty-day mortality decreased from 13.6% to 11.0% (RR 0.81, 95% CI 0.76 to 0.87), while 2-year mortality decreased from 26.4% to 22.7% (RR 0.86, 95% CI 0.82 to 0.90).
| Variable | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | Overall |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of patients | 12,437 | 12,116 | 11,678 | 11,507 | 12,081 | 11,756 | 11,596 | 12,205 | 11,427 | 106,803 |
| Median age (years) | 67.5 | 67.3 | 68.2 | 68.0 | 68.2 | 68.7 | 67.9 | 68.3 | 68.7 | 68.0 |
| Median index length of stay (days) | 8 | 8 | 8 | 7 | 7 | 7 | 6 | 6 | 5 | 7 |
| Men | 66.1% | 65.5% | 65.5% | 65.5% | 64.7% | 64.6% | 64.6% | 63.8% | 63.7% | 64.9% |
| Chronic co-morbidities at presentation | ||||||||||
| Chronic heart failure | 20.0% | 21.7% | 21.0% | 21.0% | 21.3% | 21.5% | 20.5% | 20.1% | 20.5% | 20.8% |
| Cerebrovascular disease | 6.1% | 6.0% | 7.2% | 6.9% | 6.9% | 6.1% | 5.3% | 5.4% | 5.2% | 6.1% |
| Diabetes mellitus | 20.0% | 21.1% | 21.9% | 22.5% | 24.3% | 24.6% | 24.9% | 23.7% | 24.9% | 23.1% |
| Chronic renal failure | 6.0% | 6.3% | 7.1% | 7.8% | 9.4% | 10.5% | 11.5% | 11.9% | 13.0% | 9.2% |
| Hypertension | 25.1% | 26.1% | 29.4% | 30.7% | 34.1% | 37.6% | 37.7% | 39.3% | 40.6% | 33.3% |
| Acute co-morbidities at presentation | ||||||||||
| Acute renal failure | 4.9% | 3.9% | 4.2% | 4.5% | 5.0% | 5.3% | 6.5% | 6.2% | 7.1% | 5.2% |
| Shock | 4.3% | 3.8% | 3.8% | 4.0% | 3.4% | 3.4% | 3.5% | 3.4% | 3.6% | 3.7% |
| Dysrhythmias | 15.4% | 16.0% | 18.8% | 18.4% | 21.9% | 23.0% | 20.0% | 17.7% | 17.8% | 18.8% |
| Mortality after AMI | ||||||||||
| At 30 days | 13.6% | 13.6% | 12.9% | 12.8% | 11.8% | 11.2% | 11.1% | 10.9% | 11.0% | 12.1% |
| At 365 days | 21.5% | 20.9% | 20.7% | 20.3% | 19.5% | 19.4% | 18.9% | 19.0% | 18.5% | 19.9% |
| At 730 days | 26.4% | 25.3% | 25.7% | 24.6% | 24.1% | 24.2% | 23.4% | 23.1% | 22.7% | 24.4% |
The yearly proportion of patients who underwent PCI in the acute phase after AMI increased by 380% (RR 3.81, 95% CI 3.62 to 4.00) over the study period ( Figure 1 ). The use of PCI in the chronic phase was largely unchanged, corresponding to an average yearly rate of 8.5%. Concurrently, the use of diagnostic cardiac catheterization decreased over time in the acute and chronic periods ( Figure 1 ). After a rapid 180% increase from 1996 to 2000 (RR 1.79, 95% CI 1.69 to 1.89) in its early use, the proportion of MPI decreased consistently in the acute and chronic phases ( Figure 1 ). The proportion of MUGA decreased precipitously ( Figure 1 ).
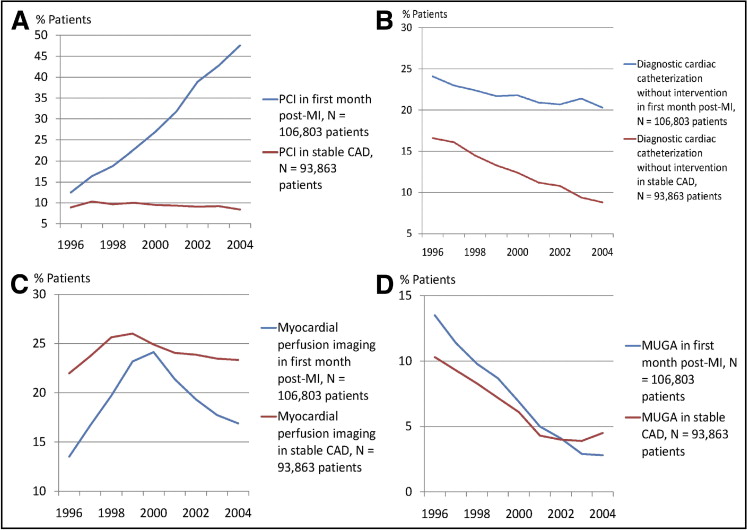
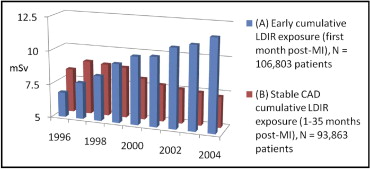
Cumulative exposure to LDIR from cardiac imaging in the acute phase increased by 172% over the study period ( Figure 2 , Table 2 ), to a mean of 11.8 mSv/patient. Among patients in the chronic phase, there was a sustained decrease in cumulative exposure to LDIR over the study period ( Figure 2 , Table 2 ). Overall, the total cumulative cardiac LDIR in the 2 years after first AMI increased by 26%, from 15.1 to 19.1 mSv/patient.
| Year | Cumulative LDIR Exposure (mSv) | ||
|---|---|---|---|
| Acute (<1 Month After AMI) | Chronic (1–36 Months After AMI) | Total (0–36 Months After AMI) | |
| 1996 | 6.84 | 8.26 | 15.1 |
| 1997 | 7.70 | 8.98 | 16.68 |
| 1998 | 8.35 | 8.87 | 17.22 |
| 1999 | 9.37 | 8.76 | 18.13 |
| 2000 | 10.03 | 8.05 | 18.08 |
| 2001 | 10.13 | 7.71 | 17.84 |
| 2002 | 10.89 | 7.54 | 18.43 |
| 2003 | 11.20 | 7.43 | 18.63 |
| 2004 | 11.82 | 7.27 | 19.09 |
Demographic data differed between the exposure strata in the first acute phase ( Table 3 ), as they did similarly in the chronic phase and overall during the 3 years after AMI (data not shown). When comparing the exposed patients, several significant predictors of heavier LDIR exposure were identified: younger age, treatment by a cardiologist, longer length of stay for index AMI admission, as well as the absence of chronic heart failure, cerebrovascular disease, and acute or chronic renal failure ( Table 3 ). Overall, all-cause mortality at 30 days, 1 year, and 2 years decreased across the exposure strata as exposure increased ( Table 3 ); that is, patients most heavily exposed were more likely to be alive at these follow-up intervals. This trend continued to be true within the exposed patients, reflecting a dose-related trend.
| Variable | Cumulative LDIR Exposure (mSv) | p Value ⁎ | |||||
|---|---|---|---|---|---|---|---|
| 0 | 0–10 | 10–20 | 20–30 | >30 | All | ||
| Number of patients | 3,094 | 1673 | 5,008 | 827 | 825 | 11,427 | — |
| Median ± SD age (years) | 77.7 ± 13.3 | 66.0 ± 12.5 | 63.1 ± 12.9 | 66.4 ± 12.0 | 64.4 ± 12.0 | 67.9 ± 14.2 | 0.368 |
| Median index length of stay (days) | 6 | 9 | 5 | 9 | 9 | 6 | 0.001 |
| Men | 51.0% | 65.5% | 69.8% | 67.7% | 66.1% | 63.7% | 0.004 |
| Chronic co-morbidities at presentation | |||||||
| Chronic heart failure | 34.7% | 20.1% | 12.5% | 20.7% | 16.6% | 20.5% | <0.001 |
| Cerebrovascular disease | 9.1% | 6.1% | 2.9% | 4.2% | 3.3% | 5.2% | <0.001 |
| Diabetes | 30.6% | 27.3% | 19.7% | 30.8% | 24.5% | 24.9% | <0.001 |
| Malignancy | 5.4% | 2.8% | 2.0% | 2.6% | 2.1% | 3.1% | 0.181 |
| Hypertension | 37.3% | 45.3% | 40.0% | 43.4% | 44.0% | 40.6% | <0.001 |
| Chronic renal failure | 25.6% | 10.2% | 7.3% | 10.3% | 8.5% | 13.0% | <0.001 |
| Acute co-morbidities at presentation | |||||||
| Acute renal failure | 15.0% | 4.5% | 3.8% | 6.5% | 3.8% | 7.1% | 0.004 |
| Shock | 7.0% | 3.1% | 2.1% | 2.5% | 2.6% | 3.6% | 0.181 |
| Dysrhythmias | 26.7% | 15.8% | 13.6% | 17.2% | 14.7% | 17.8% | 0.015 |
| Specialty of treating physician | |||||||
| Generalist practitioner/general internist | 54.0% | 40.9% | 33.5% | 31.7% | 33.1% | 40.0% | <0.001 |
| Cardiologist | 34.1% | 48.7% | 58.9% | 58.5% | 59.9% | 50.7% | <0.001 |
| Other subspecialty | 11.9% | 10.3% | 7.6% | 9.8% | 7.0% | 9.3% | 0.001 |
| Mortality after AMI | |||||||
| At 30 days | 30.0% | 7.0% | 3.4% | 4.2% | 1.6% | 11.0% | — |
| At 365 days | 45.6% | 13.8% | 6.9% | 9.7% | 5.9% | 18.5% | — |
| At 730 days | 53.4% | 17.5% | 9.6% | 12.5% | 8.5% | 22.7% | — |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


