Gary J. Balady, Anthony P. Morise
Exercise Testing
Exercise electrocardiographic testing is among the most fundamental and widely used tests for the evaluation of patients with cardiovascular disease (CVD). It is easy to administer, perform, and interpret; it is flexible and adaptable; and it is reliable, inexpensive, and readily available in hospital or practice settings. The exercise test has been used by clinicians for more than half a century, and its durability can be attributed to its evolution over time. Initially developed to detect the presence of myocardial ischemia secondary to coronary artery disease (CAD), the exercise electrocardiogram (ECG) is now recognized for its power in predicting prognosis. Exercise test variables beyond the ST segment yield important information, particularly when used in combination with clinical information, to predict outcomes and guide therapy in a broad range of individuals—from the healthy to those crippled by heart disease. Emerging applications of exercise electrocardiography have demonstrated its usefulness in the evaluation and management of patients with a wide variety of cardiovascular conditions, including valvular heart disease, congenital heart disease, genetic cardiovascular conditions, arrhythmias, and peripheral arterial disease (PAD). When used appropriately with adjunctive modalities to measure gas exchange and ventilation or with imaging techniques such as echocardiography or nuclear perfusion imaging (see Chapters 14 and 16), the power of the exercise ECG is greatly enhanced. The exercise ECG is the clinician’s beacon that can guide optimal care for a great majority of patients with known or suspected CVD. This chapter provides a detailed foundation of information on the exercise ECG. Other chapters in this text address adjunctive imaging techniques and further discuss the use of exercise testing in patients with specific cardiovascular conditions.
Physiology of Exercise Testing
Total-Body Oxygen Uptake
Exercising muscles require energy to contract and relax. Most of this energy is derived from oxidative metabolism to generate adenosine triphosphate; hence energy requirements at rest and for any given amount of physical activity (work rate) can be estimated from measurements of total-body oxygen uptake ( ). The Fick equation demonstrates that
). The Fick equation demonstrates that  is equal to the product of cardiac output and oxygen extraction at the periphery (i.e., arteriovenous oxygen difference).
is equal to the product of cardiac output and oxygen extraction at the periphery (i.e., arteriovenous oxygen difference).  is easily expressed in multiples of resting oxygen requirements (metabolic equivalents [METs]), with 1 MET being resting energy expenditure and defined as approximately 3.5 mL oxygen/kg body weight/min. This convenient system indexes the amount of energy used during any given physical activity against that used at rest. Accordingly, 5-MET activity requires five times the energy expenditure at rest.
is easily expressed in multiples of resting oxygen requirements (metabolic equivalents [METs]), with 1 MET being resting energy expenditure and defined as approximately 3.5 mL oxygen/kg body weight/min. This convenient system indexes the amount of energy used during any given physical activity against that used at rest. Accordingly, 5-MET activity requires five times the energy expenditure at rest.  is the peak oxygen uptake achieved during performance of the highest level of dynamic exercise involving large muscle groups and by definition cannot be exceeded despite increases in work rate. It is related to age, sex, heredity, exercise habits, and cardiovascular status. Cardiac output can increase as much as four to six times resting levels in the upright position. Maximum cardiac output is the result of a twofold to threefold increase in heart rate from resting levels and an increase in stroke volume. Stroke volume in healthy persons generally plateaus at 50% to 60% of
is the peak oxygen uptake achieved during performance of the highest level of dynamic exercise involving large muscle groups and by definition cannot be exceeded despite increases in work rate. It is related to age, sex, heredity, exercise habits, and cardiovascular status. Cardiac output can increase as much as four to six times resting levels in the upright position. Maximum cardiac output is the result of a twofold to threefold increase in heart rate from resting levels and an increase in stroke volume. Stroke volume in healthy persons generally plateaus at 50% to 60% of  . Oxygen extraction at the periphery can increase as much as threefold, and the maximum arteriovenous oxygen difference has a physiologic limit of 15 to 17 mL oxygen/100 mL blood. During clinical exercise testing, patients are prompted to exercise not until they attain
. Oxygen extraction at the periphery can increase as much as threefold, and the maximum arteriovenous oxygen difference has a physiologic limit of 15 to 17 mL oxygen/100 mL blood. During clinical exercise testing, patients are prompted to exercise not until they attain  but rather to the
but rather to the  that is attained during symptom-limited, maximum tolerated exercise—this level is termed the
that is attained during symptom-limited, maximum tolerated exercise—this level is termed the  peak.1
peak.1
Effects of Exercise on Myocardial Oxygen Demand and Supply Relationships
Myocardial ischemia occurs when the supply of oxygenated blood to myocardial cells is inadequate to meet demands. Many factors affect the delicate balance of supply and demand (Fig. 13-1). Exercise testing is performed to stress these relationships and observe the physiologic responses that ensue. This enables the clinician to not only assess for the development of myocardial ischemia but, importantly, to also evaluate at what level of myocardial oxygen demand and physical activity (work rate) it occurs.1
Technical Aspects of Exercise Testing
Subject Preparation
Patient Assessment
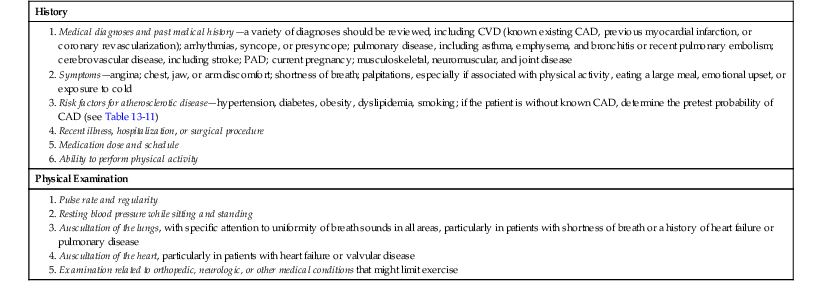
It is important to assess the patient before performing the exercise test to evaluate the indications for the test, the appropriateness of the specific test that has been ordered to answer the question posed, the ability of the patient to perform exercise, and whether the patient has any contraindications to exercise testing (Table 13-1). Information from the medical history as provided by the patient, chart review, and the ordering provider and/or the patient’s primary care physician or cardiologist can be most useful in this pretest evaluation. A brief physical examination that addresses the components outlined in Table 13-2 can also be helpful. A current standard resting 12-lead ECG is useful in assessing heart rate, rhythm, conduction abnormalities, and evidence of previous myocardial infarction and should be compared with the most recent previous ECG, if available.
TABLE 13-1
Contraindications to Exercise Testing
| Absolute Contraindications |
| Relative Contraindications |
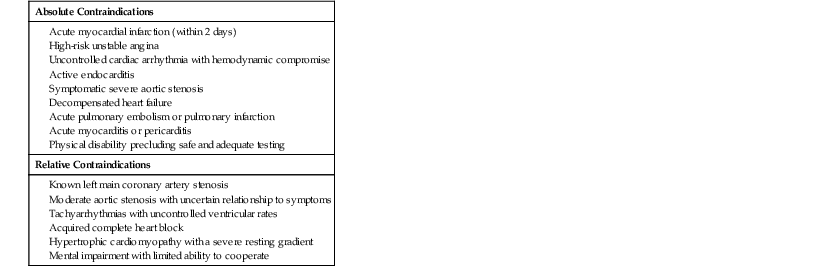
From Fletcher GF, Ades PA, Kligfield P, et al: Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation 128:873, 2013.
TABLE 13-2
Patient Assessment for Exercise Testing
| History |
| Physical Examination |
Although diagnostic exercise tests in patients without known CAD are best performed by withholding cardioactive medications on the day of the test to better assess for an ischemic response, functional testing in patients with known CAD might best be performed with patients having taken their usual medications to evaluate the effects of the medications on heart rate, blood pressure, symptoms, and ischemia during exercise. This issue is discussed again later in this chapter (see Medication Effects).
In patients with permanent cardiac pacemakers, it is important to obtain information from the patient’s cardiologist regarding the type of pacemaker (single or dual chamber), programmed mode, rate responsiveness, and pacing heart rate limits before the test. Similarly, in patients with implantable cardioverter-defibrillators (ICDs), information regarding ICD rhythm detection and treatment algorithms should be obtained so that the peak heart rate during the exercise test is maintained at least 10 beats/min below the programmed heart rate threshold for antitachycardia pacing and defibrillation.2 Additional details of patient assessment are provided elsewhere.1
Electrocardiographic Lead Systems
As the technology of exercise electrocardiographic testing has evolved, several different types of lead systems have been developed and used. Details regarding these lead systems, along with skin preparation techniques, are provided elsewhere.1,3 The importance of adequate skin preparation cannot be overstated, as this is essential to optimize the quality of the exercise ECG. To obtain a high-quality 12-lead ECG during testing, electrode placement on the torso is standard for routine testing. Torso electrodes are placed under the lateral aspect of the clavicles for the arm leads and on the lower end of the rib cage or high under the rib cage for the leg leads. A standard 12-lead ECG should be performed before placement of the torso limb leads because such lead placement may alter the inferior lead complexes and result in previous Q waves being either mimicked or hidden.
Exercise Test Modality and Protocols
The testing modality and protocol should be selected in accordance with the patient’s estimated functional capacity based on age, estimated physical fitness from the patient’s history, and underlying disease. Several exercise test protocols are available for both treadmill and stationary cycle ergometers. Patients who have low estimated fitness levels or are deemed to be at higher risk because of underlying disease (e.g., recent myocardial infarction, heart failure) should be tested with a less aggressive exercise protocol. Treadmill and cycle ergometers may use stepped or continuous ramp protocols. Work rate increments (stages) during stepped protocols can vary from 1 to 2.5 METs. Ramp protocols are designed with stages that are no longer than 1 minute and for the patient to attain peak effort within 8 to 12 minutes. Accordingly, ramp protocols must be individualized and selected to accommodate the patient’s estimated exercise capacity. Because there are no widely published or standard sets of ramp protocols, individual exercise testing laboratories usually develop their own customized protocols that accommodate a wide range of fitness levels. Examples of such protocols are shown in Table 13-3.4,5 A variety of treadmill and cycle ergometer testing protocols are provided in detail by the American College of Sports Medicine (ACSM).2
TABLE 13-3
Boston Medical Center Treadmill Ramp Protocols
| STAGE* | VERY LOW RAMP | LOW RAMP | MODERATE RAMP | HIGH RAMP | ATHLETE’S RAMP | ||||||||||
| mph | % Grade | METs | mph | % Grade | METs | mph | % Grade | METs | mph | % Grade | METs | mph | % Grade | METs | |
| 1 | 1.0 | 0.0 | 1.8 | 1.0 | 0.0 | 1.8 | 1.5 | 1.5 | 2.5 | 2.1 | 3.0 | 3.5 | 1.8 | 0.0 | 2.4 |
| 2 | 1.1 | 0.2 | 1.9 | 1.1 | 0.5 | 1.9 | 1.6 | 2.0 | 2.7 | 2.2 | 4.0 | 3.9 | 2.1 | 0.5 | 2.7 |
| 3 | 1.2 | 0.4 | 2.0 | 1.2 | 1.0 | 2.1 | 1.7 | 2.5 | 2.9 | 2.3 | 4.5 | 4.2 | 2.4 | 1.0 | 3.2 |
| 4 | 1.3 | 0.6 | 2.1 | 1.3 | 1.5 | 2.3 | 1.8 | 3.0 | 3.1 | 2.4 | 5.5 | 4.6 | 2.7 | 1.5 | 3.6 |
| 5 | 1.4 | 0.8 | 2.2 | 1.4 | 2.0 | 2.5 | 1.9 | 3.5 | 3.4 | 2.5 | 6.0 | 5.0 | 3.0 | 2.0 | 4.1 |
| 6 | 1.5 | 1.0 | 2.3 | 1.5 | 2.5 | 2.7 | 2.0 | 4.0 | 3.6 | 2.6 | 7.0 | 5.5 | 3.3 | 2.5 | 4.6 |
| 7 | 1.6 | 1.2 | 2.5 | 1.6 | 3.0 | 2.9 | 2.1 | 4.5 | 3.9 | 2.7 | 7.5 | 5.8 | 3.6 | 3.0 | 5.2 |
| 8 | 1.7 | 1.4 | 2.6 | 1.7 | 3.5 | 3.1 | 2.2 | 5.0 | 4.2 | 2.8 | 8.5 | 6.4 | 3.9 | 3.5 | 6.1 |
| 9 | 1.8 | 1.6 | 2.8 | 1.8 | 4.0 | 3.4 | 2.3 | 5.5 | 4.5 | 2.9 | 9.0 | 6.8 | 4.2 | 4.0 | 7.3 |
| 10 | 1.9 | 1.8 | 2.9 | 1.9 | 4.5 | 3.6 | 2.4 | 6.0 | 4.8 | 3.0 | 10.0 | 7.4 | 4.5 | 4.5 | 8.4 |
| 11 | 2.0 | 2.0 | 3.1 | 2.0 | 5.0 | 3.9 | 2.5 | 6.5 | 5.1 | 3.1 | 10.5 | 7.8 | 4.8 | 5.0 | 9.5 |
| 12 | 2.1 | 2.2 | 3.2 | 2.1 | 5.5 | 4.2 | 2.6 | 7.0 | 5.5 | 3.2 | 11.5 | 8.5 | 5.1 | 5.5 | 10.6 |
| 13 | 2.2 | 2.4 | 3.4 | 2.2 | 6.0 | 4.5 | 2.7 | 7.5 | 5.8 | 3.3 | 12.0 | 8.9 | 5.4 | 6.0 | 11.5 |
| 14 | 2.3 | 2.6 | 3.6 | 2.3 | 6.5 | 4.8 | 2.8 | 8.0 | 6.2 | 3.4 | 13.0 | 9.7 | 5.7 | 6.5 | 12.2 |
| 15 | 2.4 | 2.8 | 3.8 | 2.4 | 7.0 | 5.1 | 2.9 | 8.5 | 6.6 | 3.5 | 13.5 | 10.1 | 6.0 | 7.0 | 13.0 |
| 16 | 2.5 | 3.0 | 3.9 | 2.5 | 7.5 | 5.5 | 3.0 | 9.0 | 7.0 | 3.6 | 14.5 | 10.9 | 6.3 | 7.5 | 13.8 |
| 17 | 2.6 | 3.2 | 4.1 | 2.6 | 8.0 | 5.8 | 3.1 | 9.5 | 7.4 | 3.7 | 15.0 | 11.4 | 6.6 | 8.0 | 14.7 |
| 18 | 2.7 | 3.4 | 4.3 | 2.7 | 8.5 | 6.2 | 3.2 | 10.0 | 7.8 | 3.8 | 16.0 | 12.2 | 6.9 | 8.5 | 15.5 |
| 19 | 2.8 | 3.6 | 4.5 | 2.8 | 9.0 | 6.6 | 3.3 | 10.5 | 8.3 | 3.9 | 16.5 | 12.6 | 7.2 | 9.0 | 16.4 |
| 20 | 2.9 | 3.8 | 4.7 | 2.9 | 9.5 | 7.0 | 3.4 | 11.0 | 8.7 | 4.0 | 17.5 | 13.3 | 7.5 | 9.5 | 17.3 |
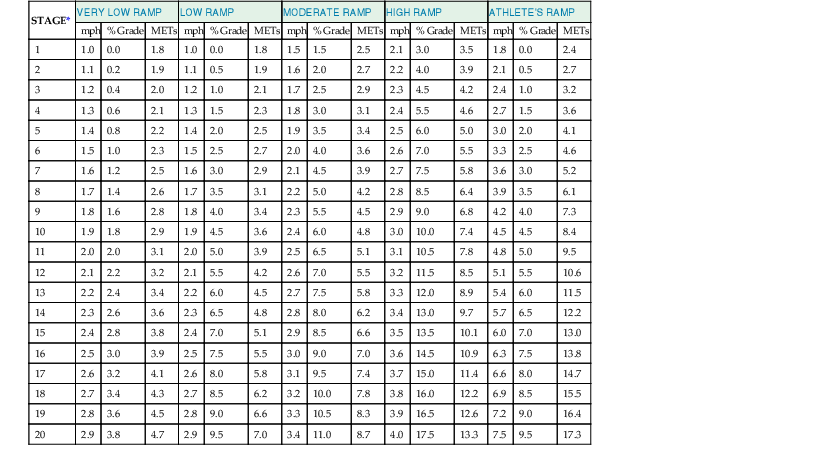
* Stages are each 30 seconds in duration
Exercise tests may be submaximal or maximal relative to the patient’s effort. In addition to common indications for stopping the exercise test (Table 13-4), submaximal exercise testing has a predetermined endpoint often defined as a peak heart rate (e.g., 120 beats/min or 70% of predicted maximum heart rate) or an arbitrary MET level (e.g., 5 METs). Submaximal tests are used in patients early after myocardial infarction before discharge from the hospital because they can provide prognostic information to guide management. They can also be useful in the evaluation of a patient’s ability to engage in daily activities after discharge and in addition serve as a baseline for cardiac rehabilitative exercise therapy (see the later section Physical Activity and Exercise Prescription). Symptom-limited tests are designed to continue until the patient demonstrates signs and/or symptoms necessitating termination of exercise (see Table 13-4). Whatever modality or protocol is used, standard patient monitoring and measurements are made during and early after exercise, as outlined in Table 13-5.
TABLE 13-4
Indications for Terminating an Exercise Test
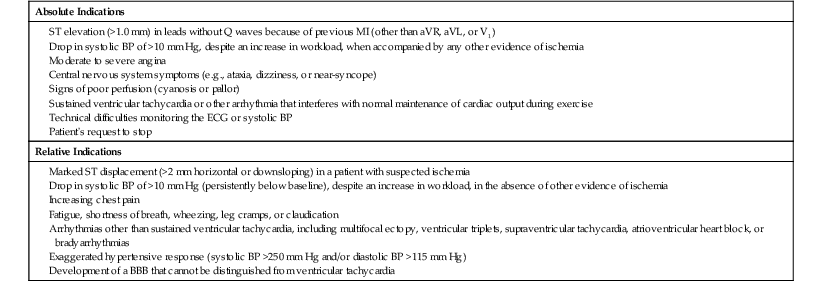
BBB = bundle branch block; BP = blood pressure; MI = myocardial infarction.
From Fletcher GF, Ades PA, Kligfield P, et al: Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation 128:873, 2013.
TABLE 13-5
Patient Monitoring During Exercise Testing
| During the Exercise Period |
| During the Recovery Period |
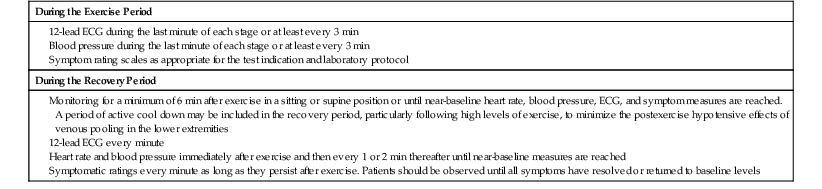
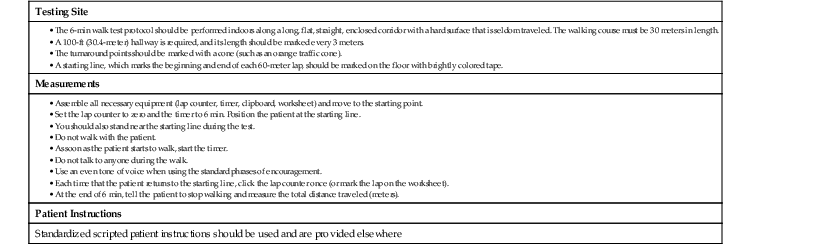
TABLE 13-8
Six-Minute Walk Test Protocol
| Testing Site |
| Measurements |
• Set the lap counter to zero and the timer to 6 min. Position the patient at the starting line. • You should also stand near the starting line during the test. • Do not walk with the patient. • As soon as the patient starts to walk, start the timer. • Do not talk to anyone during the walk. • Use an even tone of voice when using the standard phrases of encouragement. |
| Patient Instructions |
| Standardized scripted patient instructions should be used and are provided elsewhere |
Data from American Thoracic Society: ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med 166:111, 2002. Official journal of the American Thoracic Society.
Exercise Test Supervision
Over the past 30 years since the American Heart Association (AHA) published its first set of Standards for Adult Exercise Testing Laboratories, the role of the physician in ensuring that the exercise laboratory is properly equipped and appropriately staffed with qualified personnel who adhere to a written set of policies and procedures specific to that laboratory has not changed. In subsequent iterations of their respective guidelines, the AHA, the ACSM, the American College of Cardiology (ACC), and the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) have consistently addressed this issue. In the year 2000, the ACC/AHA/American College of Physicians/American College of Sports Medicine Competency Task Force focused its efforts on outlining the specific cognitive and training requirements for personnel involved in supervising and interpreting exercise ECGs and was the first to look beyond the specific professional type (e.g., physician, nurse, exercise physiologist) and focus on specific competencies of the individual staff member.8 This statement clearly defined different levels of supervision as follows: (1) “personal supervision” requires a physician’s presence in the room; (2) “direct supervision” requires a physician to be in the immediate vicinity, on the premises or the floor, and be available for emergencies; and (3) “general supervision” requires the physician to be available by phone or by page.8 Common to every guideline is the recommendation that patients be screened before exercise testing to assess their risk for an exercise-related adverse event so that the most appropriate personnel to supervise the test can be provided. Exercise testing may be supervised by nonphysician staff members who are deemed competent according to the criteria outlined in the ACC/AHA statement.8 In all such cases the physician should be immediately available to assist as needed (i.e., provide direct supervision); in high-risk patients the physician should personally supervise the test (i.e., provide personal supervision).
Risks of Exercise Testing
Exercise is associated with increased risk for an adverse cardiovascular event, and hence details regarding the safety of exercise testing and emergency preparedness in exercise laboratories are addressed in depth in guidelines from the AHA1,3 and the ACSM.2 Nonetheless, the safety of exercise testing is well documented and the overall risk for adverse events is quite low. In several large series of subjects with and without known CVD, the rate of major complications (including myocardial infarction and other events requiring hospitalization) was less than 1 to as high as 5 per 10,000 tests, and the rate of death was less than 0.5 per 10,000 tests. The incidence of adverse events depends on the study population.6 Patients with recent myocardial infarction, reduced left ventricular systolic function, exertion-induced myocardial ischemia, and serious ventricular arrhythmias are at highest risk.1 In more than 2000 subjects with New York Heart Association Functional class II to IV systolic heart failure who completed exercise testing in the HF-ACTION (Heart Failure: A Controlled Trial Investigating Outcomes of exercise traiNing) study, there were no deaths and the rate of nonfatal major cardiovascular events was lower than 0.5 per 1000 tests.9 A recent report of 5060 CPX studies performed in patients with severe functional impairment and a variety of high-risk cardiac diseases, including heart failure, hypertrophic cardiomyopathy (HCM), pulmonary hypertension, and aortic stenosis, further supports the safety of exercise testing. The adverse event rate was 0.16%, and the most common adverse event was sustained ventricular tachycardia. No fatal events were reported.10
Maintenance of appropriate emergency equipment, establishment of an emergency plan, and regular practice in carrying out the plan are fundamental to ensuring safety in an exercise testing laboratory.3
Exercise Testing in Patients with Coronary Artery Disease
Clinical Responses
Any chest pain produced during the exercise test needs to be factored into the exercise test conclusion and report.
First, are the symptoms reported during the test the same or similar to the reported historical symptoms that prompted the exercise test? If the answer is yes, the clinician can assess the objective test responses and discern whether they support the presence of CAD. If the answer is no, differences between the produced and historical symptoms need to be clarified. In addition, the symptoms produced need to be categorized according to whether they are consistent with angina. Distinguishing anginal from nonanginal chest pain is important at the time of occurrence of the chest pain. Angina is not well localized, pleuritic, or associated with palpable tenderness (see Chapter 11), and the only opportunity to define these qualities may be after the exercise test.
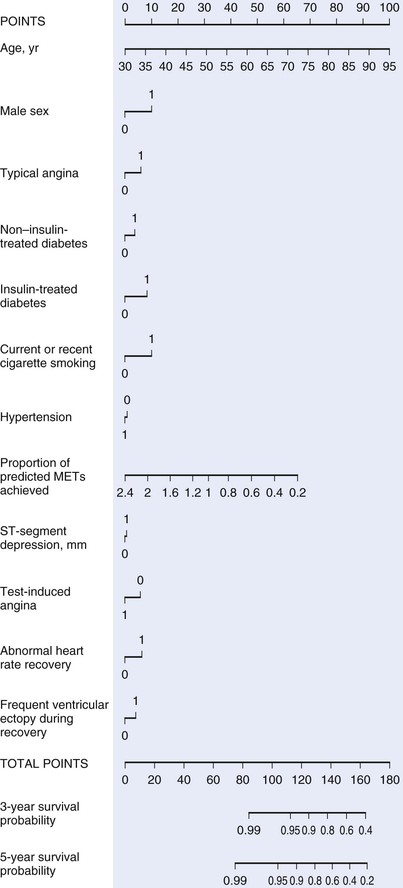
Second, exercise-induced angina is an important clinical predictor of the presence and severity of CAD, equal to or greater than ST-segment depression. Consideration of limiting versus nonlimiting chest pain, in addition to any induced angina, has been incorporated into the Duke treadmill score, as well as into other treadmill scores (see later). These factors will have an impact on prognostic and diagnostic assessment of the test results and ultimately the next step in the clinical evaluation.
Exercise Capacity
Exercise capacity is a strong predictor of mortality and nonfatal cardiovascular outcomes in both men and women with and without CAD.11,12 Even though exercise capacity is most accurately measured by CPX, a reasonable estimate can be obtained from treadmill testing alone.13 The best methods for estimating predicted METs are the following simple regression equations:
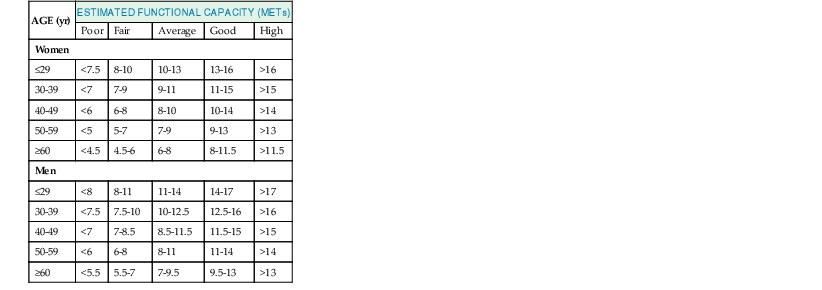
The reported exercise time can be translated into metabolic equivalents or METs based on the exercise test protocol. The reported METs can then be expressed as a percentage of the predicted METs. An alternative qualitative classification of functional capacity that adjusts for age and sex is provided in Table 13-9.
In addition to clinical factors, exercise capacity can be related to familiarity with the exercise equipment, level of training, and environmental conditions in the exercise laboratory. Patients who cannot perform an exercise test or who undergo a pharmacologic stress test have a worse prognosis than do those who can perform an exercise test.
Exercise capacity should always be incorporated into the results, conclusions, and/or recommendations of the exercise test report. Exercise capacity can be incorporated into available multivariable scores such as the Duke treadmill score or the method of Lauer (see later and Fig. 13-2) to classify the prognosis as low, intermediate, or high risk.
Hemodynamic Responses
Heart Rate
Maximum Heart Rate
The maximum heart rate with exercise is a fundamental physiologic parameter that provides the clinician relevant information concerning the intensity of exercise, the adequacy of the exercise test, the effect of medications that influence heart rate, the potential contribution to exercise intolerance, and the patient’s prognosis.14 The maximum achievable heart rate (HRmax) is unique for each patient but can be estimated by using regression equations that adjust for the patient’s age. The most familiar equation, which was developed principally in middle-aged men, is
Although easy to apply and calculate, there is considerable variability with this equation, especially in patients with CAD who are taking beta blockers. Newer equations14 have been proposed to replace the 220 − age rule to generate the age-predicted maximum heart rate:
Chronotropic Incompetence
Inability of the heart to increase its rate to meet the demand placed on it is termed chronotropic incompetence. It is considered an independent predictor of cardiac or all-cause mortality, as well as other adverse cardiovascular outcomes.14 This independence also includes the well-established Duke treadmill score.15
A submaximal study is assigned when the peak heart rate achieved is below the age-predicted maximum heart rate. An inadequate study is defined by failure to achieve a predefined goal, such as 85% of the age-predicted maximum heart rate. If a patient without known CAD has an inadequate study, the term nondiagnostic study is often applied. As with all things, this “nondiagnostic” status is relative. In the presence of any other diagnostic endpoints, such as 2-mm or greater ST-segment depression or exercise-induced hypotension, the heart rate adequacy question becomes irrelevant. One might even extend that argument to reproduction of the patient’s reported chest pain symptoms.
Chronotropic incompetence most commonly has been defined by the adjusted heart rate reserve, which incorporates both resting and peak heart rates, as well as the age-adjusted maximum heart rate. However, before the term chronotropic incompetence is applied, consideration should be given to the effort exerted in performing exercise, present medications, and the reason for termination of the exercise test. Effort applied to the exercise is often defined by the symptoms produced or by indices of perceived exertion such as the Borg scale.1 These work well in most settings but can also be defined quantitatively by using CPX parameters such as the respiratory exchange ratio. For the usual non-CPX application, the following formula14,14a defines the chronotropic index:
Failure to achieve a chronotropic index higher than 80% defines the presence of chronotropic incompetence. In patients taking nontrivial doses of beta blockers who are compliant with their medication, a value lower than 62% is considered chronotropic incompetence, but this criterion is not universally accepted.16 Criteria for assessing chronotropic incompetence in patients with atrial fibrillation have not been established.
Get Clinical Tree app for offline access

 ). Diminution of vagal tone and a rise in sympathetic tone lead to an increase in heart rate and left ventricular contractility. Stroke volume also rises because of increases in venous return of blood from exercising muscles, and blood flow is redistributed from the renal, splanchnic, and cutaneous circulation to the exercising muscles. Accumulation of metabolites in the actively contracting muscles causes vasodilation of muscle arterioles, which increases skeletal muscle blood flow up to four times that of resting levels and results in a reduction in aortic outflow impedance. This, in turn, allows more complete systolic ejection, thereby further increasing stroke volume. Systolic blood pressure increases mostly because of the rise in cardiac output, whereas diastolic blood pressure either remains constant or falls as a result of the reduction in vascular resistance. The size and location of the exercising muscle groups will have different effects on the hemodynamic response to exercise. Dynamic arm exercise elicits higher heart rate and blood pressure responses at any given work rate than does dynamic leg exercise. Arm work yields differences in sympathetic output, peripheral vasodilation, venous return, and metabolic requirements, which are influenced not only by the exercising muscle mass but also by the stabilizing muscles recruited during arm exercise.
). Diminution of vagal tone and a rise in sympathetic tone lead to an increase in heart rate and left ventricular contractility. Stroke volume also rises because of increases in venous return of blood from exercising muscles, and blood flow is redistributed from the renal, splanchnic, and cutaneous circulation to the exercising muscles. Accumulation of metabolites in the actively contracting muscles causes vasodilation of muscle arterioles, which increases skeletal muscle blood flow up to four times that of resting levels and results in a reduction in aortic outflow impedance. This, in turn, allows more complete systolic ejection, thereby further increasing stroke volume. Systolic blood pressure increases mostly because of the rise in cardiac output, whereas diastolic blood pressure either remains constant or falls as a result of the reduction in vascular resistance. The size and location of the exercising muscle groups will have different effects on the hemodynamic response to exercise. Dynamic arm exercise elicits higher heart rate and blood pressure responses at any given work rate than does dynamic leg exercise. Arm work yields differences in sympathetic output, peripheral vasodilation, venous return, and metabolic requirements, which are influenced not only by the exercising muscle mass but also by the stabilizing muscles recruited during arm exercise.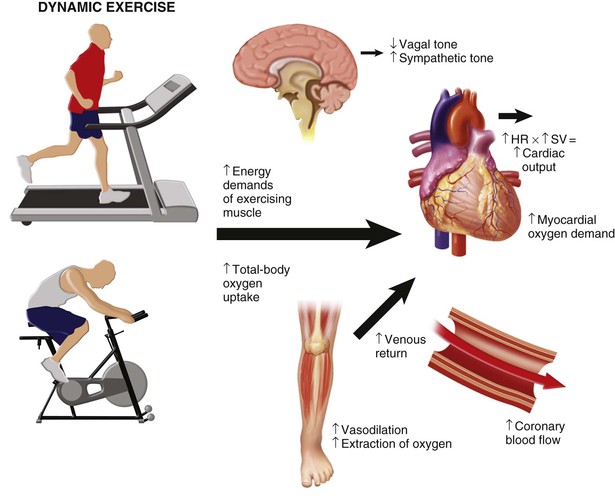
 ) and METs from work rate with the treadmill or cycle ergometer, many laboratories perform cardiopulmonary exercise testing (CPX), which uses ventilatory gas exchange analysis during exercise to provide a more reliable and reproducible measure of
) and METs from work rate with the treadmill or cycle ergometer, many laboratories perform cardiopulmonary exercise testing (CPX), which uses ventilatory gas exchange analysis during exercise to provide a more reliable and reproducible measure of  . Peak
. Peak  is the most accurate measure of exercise capacity and is a useful reflection of overall cardiopulmonary health. Measurement of expired gases is not necessary for all clinical exercise testing, but the additional information can provide important physiologic data that can be useful in both clinical and research applications. Measures of gas exchange primarily include
is the most accurate measure of exercise capacity and is a useful reflection of overall cardiopulmonary health. Measurement of expired gases is not necessary for all clinical exercise testing, but the additional information can provide important physiologic data that can be useful in both clinical and research applications. Measures of gas exchange primarily include  , carbon dioxide output (
, carbon dioxide output ( ), and minute ventilation. Use of these variables in graphic form provides further information on the ventilatory threshold and ventilatory efficiency. These latter concepts are explored in detail elsewhere.
), and minute ventilation. Use of these variables in graphic form provides further information on the ventilatory threshold and ventilatory efficiency. These latter concepts are explored in detail elsewhere.

 . From a mechanistic standpoint, abnormal HRR has been associated with a high prevalence of abnormal and high-risk myocardial perfusion imaging.
. From a mechanistic standpoint, abnormal HRR has been associated with a high prevalence of abnormal and high-risk myocardial perfusion imaging.

