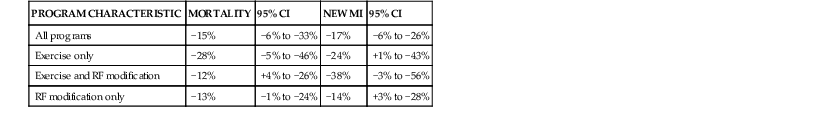
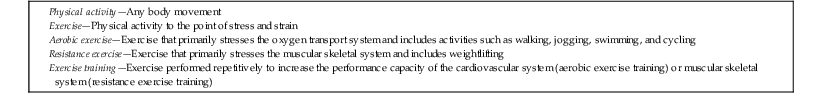
Paul D. Thompson Until the early 1950s, standard treatment of myocardial infarction (MI) was several weeks of hospitalization followed by months of restricted physical activity. Exercise-based cardiac rehabilitation was developed to reverse the physical deconditioning produced by this restriction of physical activity. Exercise training was central to this process and was one of the few interventions that reduced exertional angina pectoris in the era before beta-adrenergic blocking agents and coronary artery revascularization procedures.1 Shorter hospitalizations, along with effective medications and procedures to treat myocardial ischemia, have changed cardiac rehabilitation programs. Exercise training is still important, but education and counseling to improve psychological well-being, reduce cigarette smoking, and increase adherence to medications and diet are now key components of the rehabilitation effort.2 U.S. Centers for Medicare & Medicaid Services (CMS) guidelines reflect these changes and stipulate that “cardiac rehabilitation programs must be comprehensive and…include a medical evaluation, a program to modify cardiac risk factors…prescribed exercise, education, and counseling.” Consequently, cardiac rehabilitation programs are now often referred to as “cardiac rehabilitation/secondary prevention programs.”2 The American Heart Association (AHA) and American College of Cardiology Foundation (ACCF) recommend comprehensive cardiac rehabilitation programs (class I indication) for patients who have undergone percutaneous transluminal coronary angioplasty (PTCA) or coronary artery bypass grafting (CABG), who have suffered an acute cardiac syndrome, or who have stable angina pectoris or peripheral vascular disease.3 This recommendation received the highest level of evidence (level A) for all conditions except angina (level B).3 The CMS also considers comprehensive cardiac rehabilitation “reasonable and necessary” for patients after valve surgery and heart or heart and lung transplantation.4 They proposed using referral to cardiac rehabilitation as a core performance measure for the management of patients with coronary disease and after cardiac surgery starting in January 2014, with an impact on hospital reimbursement in 2015.5 Consequently, interest in cardiac rehabilitation will probably increase in the near future. Exercise training is central to most cardiac rehabilitation/risk reduction programs because it increases exercise capacity and reduces exercise-induced cardiac ischemia and angina, but even programs without an exercise component may reduce recurrent cardiac events. A meta-analysis of 63 randomized secondary prevention trials that included 21,295 patients with coronary artery disease (CAD) noted a 15% reduction in mortality, but the reductions in mortality and recurrent MI were similar for programs that involved exercise only, exercise and risk factor education and counseling, and risk factor education and counseling alone6 (Table 47-1). Because risk factor reduction is discussed elsewhere in detail (see also Chapters 42, 44, and 45), this chapter specifically addresses exercise training in the rehabilitation process. TABLE 47-2 Terms to Describe Exercise From Thompson PD: Exercise prescription and proscription for patients with coronary artery disease. Circulation 112:2354, 2005. Exercise performance may be normal for age and sex in individuals with cardiac disease. Alternatively, diseases that limit maximal SV, impair the HR response, or cause myocardial ischemia that produces limiting symptoms or a diminished increase in SV may impair exercise capacity. Medications that limit the HR response to exercise (such as beta-adrenergic blocking agents) or restrictions in physical activity that produce a detraining effect may also contribute to reduced exercise tolerance in cardiac patients. The primary effect of either aerobic or strength training is increased exercise capacity. With strength training, the primary adaptation is to increase muscular strength and endurance in the exercise-trained muscle. The principal effect of aerobic exercise training is increased The magnitude of the increase in exercise
Exercise-Based, Comprehensive Cardiac Rehabilitation
Historical Perspective
Effect of Cardiac Disease on Exercise Performance
Effect of Exercise Training on Exercise Performance
 . This increase in maximal exercise capacity means that any submaximal work rate requires a lower percentage of
. This increase in maximal exercise capacity means that any submaximal work rate requires a lower percentage of  , thereby reducing the HR and SBP response and Mo2 requirements. Endurance exercise training also increases the absolute VT and VT as a percentage of
, thereby reducing the HR and SBP response and Mo2 requirements. Endurance exercise training also increases the absolute VT and VT as a percentage of  . Multiple adaptations contribute to improvement in exercise tolerance after training, including increases in SV and widening of the A-V O2 Δ.
. Multiple adaptations contribute to improvement in exercise tolerance after training, including increases in SV and widening of the A-V O2 Δ.
 with endurance exercise training depends on multiple factors, including the age of the subject, the intensity and duration of the training regimen, genetic factors, underlying disease states, and whether testing and training use similar exercises. In general, young subjects trained intensively have greater improvement in exercise tolerance. Increases in
with endurance exercise training depends on multiple factors, including the age of the subject, the intensity and duration of the training regimen, genetic factors, underlying disease states, and whether testing and training use similar exercises. In general, young subjects trained intensively have greater improvement in exercise tolerance. Increases in  average 11% to 36% in cardiac rehabilitation patients,7 although the response varies with the severity of the underlying disease. Individuals with markedly reduced ventricular function, for example, may achieve much of their increase in exercise capacity by widening the A-V O2
average 11% to 36% in cardiac rehabilitation patients,7 although the response varies with the severity of the underlying disease. Individuals with markedly reduced ventricular function, for example, may achieve much of their increase in exercise capacity by widening the A-V O2![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Exercise-Based, Comprehensive Cardiac Rehabilitation
47

 ). Rearranging the Fick equation—cardiac output (Q) =
). Rearranging the Fick equation—cardiac output (Q) =  /arterial − venous O2 difference (A-V O2 Δ)—demonstrates that
/arterial − venous O2 difference (A-V O2 Δ)—demonstrates that  is the product of Q and A-V O2 Δ. Thus, the metabolic demands of exercise are met by increasing O2 delivery through increases in Q, which in turn is the product of heart rate (HR) and cardiac stroke volume (SV), as well as through increases in A-V O2 Δ. A-V O2 Δ increases during exercise by redistribution of blood flow from nonexercising tissue (such as the kidneys and splanchnic bed) to exercising muscle, by increased O2 extraction in the exercising muscle, and by hemoconcentration as a result of plasma fluid losses into the interstitial space of exercising muscle. The increase in Q during exercise is tightly coupled to the increase in
is the product of Q and A-V O2 Δ. Thus, the metabolic demands of exercise are met by increasing O2 delivery through increases in Q, which in turn is the product of heart rate (HR) and cardiac stroke volume (SV), as well as through increases in A-V O2 Δ. A-V O2 Δ increases during exercise by redistribution of blood flow from nonexercising tissue (such as the kidneys and splanchnic bed) to exercising muscle, by increased O2 extraction in the exercising muscle, and by hemoconcentration as a result of plasma fluid losses into the interstitial space of exercising muscle. The increase in Q during exercise is tightly coupled to the increase in  such that a 1-liter increase in
such that a 1-liter increase in  elicits approximately a 6-liter increase in Q. Maximal exercise capacity is measured as
elicits approximately a 6-liter increase in Q. Maximal exercise capacity is measured as  —the maximal amount of oxygen that an individual can transport during exercise before being limited by fatigue or dyspnea.
—the maximal amount of oxygen that an individual can transport during exercise before being limited by fatigue or dyspnea.  is a highly stable and reproducible measure of exercise capacity, expressed as either an absolute value in liters per minute or relative to body weight as milliliters per kilogram per minute. The maximal increase in A-V O2 Δ is fixed at approximately 15 to 17 vol-%. Because the exercise work rate determines
is a highly stable and reproducible measure of exercise capacity, expressed as either an absolute value in liters per minute or relative to body weight as milliliters per kilogram per minute. The maximal increase in A-V O2 Δ is fixed at approximately 15 to 17 vol-%. Because the exercise work rate determines  , which is the product of Q and A-V O2 Δ, and because the maximal A-V O2 Δ is relatively fixed,
, which is the product of Q and A-V O2 Δ, and because the maximal A-V O2 Δ is relatively fixed,  is an indirect measure of maximal cardiac pump capacity, or maximal Q and SV.
is an indirect measure of maximal cardiac pump capacity, or maximal Q and SV. and Q, increases in HR and SBP are determined by the exercise
and Q, increases in HR and SBP are determined by the exercise  requirement as a percentage of
requirement as a percentage of  . Consequently, for any absolute exercise level, an individual with a larger
. Consequently, for any absolute exercise level, an individual with a larger  uses less maximal capacity and has a lower HR and SBP response to exercise. The key point is that M
uses less maximal capacity and has a lower HR and SBP response to exercise. The key point is that M ) also increases as the exercise work rate increases. Increases in
) also increases as the exercise work rate increases. Increases in  and
and  are parallel early during exercise, but the rate of CO2 expiration increases more rapidly, and the coupling of
are parallel early during exercise, but the rate of CO2 expiration increases more rapidly, and the coupling of  and
and  diverge at what is termed the
diverge at what is termed the  in non–exercise-trained individuals but at higher levels of the percentage of
in non–exercise-trained individuals but at higher levels of the percentage of  in exercise-trained subjects. VT is an important measurement of exercise tolerance because it represents the maximal steady work rate that can be maintained during submaximal exercise.
in exercise-trained subjects. VT is an important measurement of exercise tolerance because it represents the maximal steady work rate that can be maintained during submaximal exercise.