EVAR Removal for Endoleak
NICHOLAS OSBORNE and GILBERT R. UPCHURCH Jr
Presentation
A 77-year-old gentleman, who underwent an endovascular abdominal aortic aneurysm repair with a bifurcated device (Cook Zenith) 3 years ago for a 7.7-cm infrarenal aneurysm on serial CT scan, was found to have an enlarging aneurysm sac. He was thought to have a type II endoleak originating from the left hypogastric branches, and this was embolized. He continued to have aneurysm growth and subsequently underwent embolization of his main left hypogastric artery and extension into the left external iliac artery. Following this, his aneurysm had enlarged to 8.8 cm, and he was referred for a second opinion. When he was seen in the clinic, he was asymptomatic. He had a nonpulsatile abdominal mass in his epigastrium and intact femoral pulses bilaterally. His laboratory studies included a normal white blood cell count of 6.3 and a creatinine of 1.0, and his C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were not elevated. An outside hospital CT scan demonstrated a large infrarenal aneurysm with a patent Cook Zenith bifurcated endograft. The left hypogastric artery was occluded with coils in place and the left limb extended into the external iliac artery. He had no evidence of a type I, type II, or type III endoleak on review of previous CT scans. He did not have any stranding around the aorta or in the retroperitoneum.
Differential Diagnosis
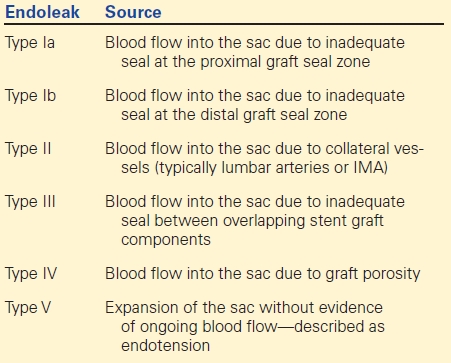
An enlarging sac following endovascular abdominal aortic aneurysm repair (EVAR) requires immediate attention to identify the source of the expansion. In general, aneurysm sac expansion can be thought to be due to endoleak (Table 1) or infection. A review of 100 consecutive explants performed at the Cleveland Clinic between 1999 and 2007 reported a temporal relationship to the indication for explant. Early explants (within 1 year of implantation) may be related to endoleak from inadequate seal (38%), less commonly type II (3%) and infection (28%). After the first year, explants are more commonly performed for type I endoleak (35%), type II endoleak (20%), and type III endoleak (24%). After 1 year, infection appears to be a less common indication for explant (7%). After 5 years, type I endoleaks remain the primary indication in over one third of explants (35%). Type III endoleaks are increasingly common (32%) as well as occlusions (9%). In approaching this patient with an endoleak diagnosed after 3 years from this primary EVAR, it is important to rule out not only endoleak but also infection.
TABLE 1. Types of Endoleaks
Workup
All EVAR patients are followed postoperatively with surveillance imaging to detect sac enlargement and endoleak. Although protocols for surveillance vary from institution to institution, initial CT angiography is the modality of choice to evaluate for an endoleak or sac enlargement in the postoperative period. This patient initially had a stable aneurysm sac following an EVAR with a type II endoleak. Over the course of 2 years, the aneurysm sac appeared to enlarge and he underwent an embolization and extension of endograft limb. When the sac continued to grow, the suspicion for infection was raised. In the absence of an endoleak, an enlarging sac may be due to endotension or infection. The patient underwent CT angiography, which failed to show any stigmata of infection, including any loss of the plane between the aorta and small bowel, stranding in the retroperitoneum or gas in the aneurysm sac (Fig. 1). He was afebrile, and he had a normal WBC count. His inflammatory markers, CRP and ESR, were both normal.
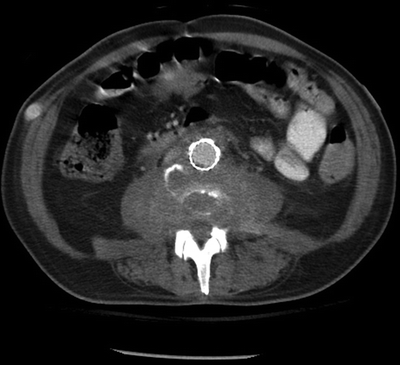
FIGURE 1 CT angiogram demonstrating a previous aortic endograft and enlarging sac.
Diagnosis and Treatment
Patients diagnosed with an expanding sac should undergo imaging to identify a cause. In the absence of an identifiable endoleak, the suspicion for infection should increase. Duplex ultrasonography can be employed to follow sac size and to detect evidence of a type I, II, or III endoleak. Although less specific and sensitive, duplex may help to identify gas within the sac or a fluid collection that could be concerning for graft infection. When there is evidence of either sac enlargement of endoleak, a CT angiogram should be performed to further evaluate the repair. CT angiography is the initial diagnostic study of choice due to the high sensitivity and specificity for graft infection and endoleak (Fig. 1). Although the sensitivity for grossly infected grafts may be as high as 95%, CT may be less useful for low-grade indolent infections (sensitivity 50%). In these cases, further imaging with either nuclear medicine tagged white blood cell scan (leukocyte scintigraphy) or FDG-PET scanning may offer higher sensitivities. FDG-PET can be fused with CT imaging and together yields a sensitivity of up to 91% for infections. Leukocyte scintigraphy, long considered the gold standard, offers similar sensitivity, but less exact localization, higher interobserver variability, and more time-intensive preparation (Fig. 2). In addition to imaging, patients with suspicion of a graft infection, either by imaging or an expanding sac without evidence of endoleak, should have routine blood cultures drawn and a CRP and an ESR as well. Although the rate of positive blood cultures is low, the ESR and CRP may be elevated with infection.
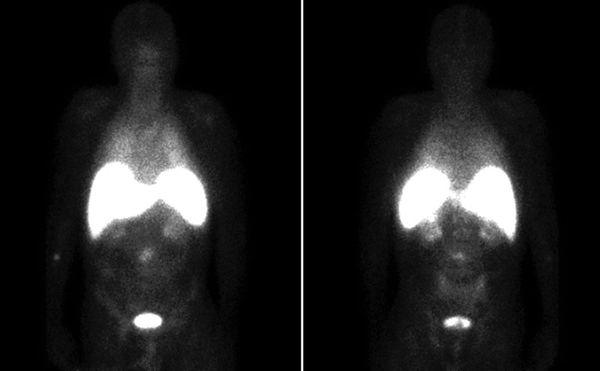
FIGURE 2 Leukocyte scintigraphy from a different patient demonstrating increased uptake in the region of the aortic graft.



