The transradial approach for percutaneous coronary procedures may be effectively performed through the right radial approach (RRA) or left radial approach (LRA) after an appropriate “learning curve.” However, studies evaluating the “learning curve” for RRA and LRA are lacking. In the Transradial Approach (Left vs Right) and Procedural Times During Percutaneous Coronary Procedures (TALENT) study, which randomized 1,540 patients to the RRA or LRA, transradial procedures were performed by either seniors or fellows. Diagnostic procedures performed by fellows were divided into 3 stages: 0 to 100 procedures (stage 1), 101 to 200 procedures (stage 2), and >200 procedures (sage 3). The primary end point of the study was fluoroscopy time during the 3 stages. Six fellows performed 532 procedures, 260 through the RRA and 272 through the LRA. During the training period, fellows showed a progressive significant reduction in fluoroscopy time for the LRA over the 3 stages (stage 1: 258 seconds, interquartile range [IQR] 138 to 377; stage 2: 198 seconds, IQR 126.5 to 375; stage 3: 142 seconds, IQR 95 to 325; p = 0.003), whereas for the RRA, only a slight and nonsignificant reduction in fluoroscopy time was observed (stage 1: 271 seconds, IQR 186 to 364; stage 2: 240 seconds, IQR 156 to 395; stage 3: 218.5 seconds, IQR 145.5 to 300.5; p = 0.20). Cannulation time was progressively reduced over the time for the 2 radial approaches: during stage 1, <40% of procedures required ≤3 minutes for radial cannulation, whereas at stage 3, radial cannulation time was ≤3 minutes in >60% of procedures (p <0.0001). In conclusion, the LRA is associated with a shorter learning curve compared to the RRA.
The transradial approach for percutaneous coronary procedures has been shown to reduce access-site vascular complications compared to the transfemoral approach. Moreover, the transradial approach reduces patient procedural discomfort, mostly because of the prolonged vascular compression time and bed rest duration associated with transfemoral access. However, the transradial approach is more demanding for operators because of its longer learning curve and increased fluoroscopy time compared to the transfemoral approach. We have previously shown that the left radial approach (LRA) is associated with lower fluoroscopy time and radiation dose adsorbed by patients compared to the right radial approach (RRA), especially when the operator is in training. However, dedicated studies evaluating the learning curve for the right or the LRA are still lacking. The aim of our study was to evaluate the learning curve for the RRA or LRA in operators in training during diagnostic coronary procedures.
Methods
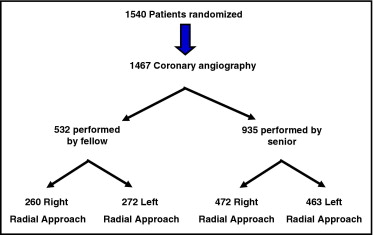
The Transradial Approach (Left vs Right) and Procedural Times During Percutaneous Coronary Procedures (TALENT) is a randomized study aiming to evaluate the safety and efficacy of the LRA compared to the RRA for percutaneous coronary procedures. From January 2009 to December 2009, of the 1,540 patients enrolled in the study, 1,467 underwent diagnostic coronary angiography and were randomized either to the RRA or to the LRA. All procedures were performed in 2 different hospitals by 10 expert operators (the senior group) and 6 operators in training (the fellow group). Allocation to 1 of the 2 approaches was made by means of a concealed computer-generated random sequence. The randomization list was managed by the nursing staff, who informed the interventional cardiologist of the assigned approach just before the procedure. There was no randomization between fellows and seniors.
The learning curve for fellows was divided into 3 stages : 0 to 100 procedures (stage 1), 101 to 200 procedures (stage 2), and >200 procedures (stage 3). Change in fluoroscopy time during the fellows’ learning curve for the RRA or LRA was considered the primary end point of the study.
Exclusion criteria were previous coronary artery bypass, hemodynamic instability, ST-segment elevation acute myocardial infarction, hemodialysis patients who also had an arteriovenous fistula.
The study was approved by the institutional ethical committee, and written informed consent was obtained to take part in the study. The study protocol is registered at ClinicalTrials.gov ( NCT 00821106 ).
The 2 hospitals perform routinely >90% of procedures through the transradial approach. A 5Fr or 6Fr artery sheath was used in all cases. The Allen test was performed before the procedure, and patients with ischemic results were excluded. The radial artery approach was performed using a hydrophilic guidewire and hydrophilic sheath (Radifocus and Introducer II; Terumo Corporation, Tokyo, Japan).
Selective catheterization of the right and left coronary arteries was carried out using Judkins curve catheters (Judkins left 3.5 and Judkins right 4). Different curve catheters were used in case of inability of the default catheters to engage coronary ostia.
Contrast injection was performed using an automatic power injection device that allows online control of contrast injection rate and volume.
For the 2 approaches, the catheterization laboratory was arranged as in the standard transfemoral approach. In case of the LRA, to reduce operator discomfort, the left arm was uplifted (using drapes and towels) to the same level as the patient’s abdomen and fixed with tape. All radial punctures were performed from the right side of the table. All procedures performed by fellows were overlooked by a senior operator located in the control room.
The radiation dose adsorbed by patients was evaluated measuring the dose-area product (DAP). The DAP was directly measured by the collimator of the angiographic system.
Radial cannulation time was considered as the time in minutes from local anesthesia to sheath insertion.
Continuous variables for the study groups are reported as mean ± SD for normally distributed variables and as medians and interquartile ranges for those not normally distributed and were compared using Student’s t test or the Mann-Whitney U test as appropriate. Categorical variables were compared using Pearson’s chi-square test or, if the expected number of patients was <5, Fisher’s exact test. Fluoroscopy time of the 3 stages of learning curve was compared using the Kruskal-Wallis test, and in case of global statistical significance, multiple comparisons were done by appropriate Mann-Whitney U test. A 2-tailed p value ≤0.05 was considered statistically significant. Statistica for Windows version 10.0 (StatSoft, Inc., Tulsa, Oklahoma) was used for all analysis.
Results
Of the 1,540 patients randomized in the study (770 RRA and 770 LRA), 1,467 patients underwent diagnostic coronary angiography (735 LRA and 732 RRA). In 532 patients, the diagnostic procedure was performed by a fellow (260 RRA and 272 LRA), and in 965 patients, the procedure was performed by a senior operator (472 RRA and 463 LRA) ( Figure 1 ). The baseline characteristics of patients are listed in Table 1 and were similar between groups.
| Characteristic | Fellows | Seniors | ||||
|---|---|---|---|---|---|---|
| RRA (n = 260) | LRA (n = 272) | p Value | RRA (n = 472) | LRA (n = 463) | p Value | |
| Age (years) | 66.6 ± 11 | 66.9 ± 10 | 0.74 | 65.3 ± 11 | 66.1 ± 11 | 0.29 |
| Men | 182 (70%) | 188 (69%) | 0.82 | 321 (68%) | 315 (68%) | 0.99 |
| Height (cm) | 168 ± 9 | 168 ± 8 | 0.87 | 168 ± 8 | 167 ± 9 | 0.82 |
| Weight (kg) | 76 ± 13 | 77 ± 14 | 0.32 | 78 ± 14 | 77 ± 14 | 0.56 |
| Body mass index (kg/m 2 ) | 26.9 ± 4 | 27.4 ± 5 | 0.31 | 27.7 ± 4 | 27.6 ± 4 | 0.66 |
| Diabetes mellitus | 71 (27%) | 84 (31%) | 0.36 | 146 (31%) | 144 (31%) | 0.96 |
| Hypertension | 190 (73%) | 190 (70%) | 0.41 | 321 (68%) | 296 (64%) | 0.19 |
| Creatinine (mg/dl) | 1 ± 0.3 | 1 ± 0.3 | 0.93 | 1 ± 0.7 | 1 ± 0.6 | 0.79 |
| Acute coronary syndromes | 70 (27%) | 82 (30%) | 0.93 | 269 (57%) | 245 (53%) | 0.21 |
| Glomerular filtration rate (ml/min) | 84 ± 31 | 85 ± 36 | 0.61 | 93 ± 38 | 91 ± 34 | 0.35 |
| Hemoglobin (g/dl) | 13.6 ± 1.6 | 13.3 ± 1.6 | 0.12 | 13.5 ± 1.7 | 13.4 ± 1.7 | 0.39 |
During the study, a progressive significant reduction in fluoroscopy time was observed in the 3 stages of the LRA learning curve ( Figure 2 , Table 2 ). In contrast, for the RRA, there was only a slight reduction in fluoroscopy time during the 3 stages of the learning curve, which did not reach a statistical significance ( Figure 3 , Table 2 ). For senior operators, no significant change over time in fluoroscopy time for the RRA or LRA was observed.
| Variable | RRA | LRA | ||||||
|---|---|---|---|---|---|---|---|---|
| Stage 1 (n = 100) | Stage 2 (n = 100) | Stage 3 (n = 60) | p Value | Stage 1 (n = 100) | Stage 2 (n = 100) | Stage 3 (n = 72) | p Value | |
| Fluoroscopy time (seconds) | 271 (186–364) | 240 (156–395) | 218.5 (145.5–300.5) | 0.20 | 258 (138–377) | 198 (126.5–375) | 142 (95–325) | 0.003 |
| DAP (Gy · cm 2 ) | 60 (43–85) | 61 (37–90) | 50 (30–91) | 0.32 | 75 (47–101) | 48 (32–76) | 36 (30–64) | <0.001 |
| ≤3-minute radial cannulation | 31 (31%) | 54 (54%) | 37 (62%) | <0.001 | 40 (40%) | 56 (56%) | 44 (61%) | 0.01 |
| Contrast dose (ml) | 89.2 ± 31 | 88.2 ± 50 | 90.8 ± 57 | 0.85 | 85.6 ± 48 | 74.5 ± 31 | 74.4 ± 32 | 0.077 |
| Subclavian tortuosity | 14 (14%) | 12 (12%) | 12 (20%) | 0.37 | 10 (10%) | 5 (5%) | 5 (7%) | 0.39 |
| Shift to femoral approach | 2 (2%) | 0 (0%) | 0 (0%) | 0.33 | 2 (2%) | 0 (0%) | 0 (0%) | 0.34 |
| Radial spasm | 2 (2%) | 2 (2%) | 1 (2%) | 1.00 | 2 (2%) | 1 (1%) | 0 (0%) | 0.78 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


