Multidetector computed tomographic coronary angiography (CTA) image quality is inversely related to the heart rate (HR). As a result beta-blocking medication is routinely administered before investigation. In the present study, the use, contraindications, and efficacy of prescan beta blockade with regard to HR reduction and CTA image quality were assessed. In 537 patients referred for CTA, the baseline HR and blood pressure were measured on arrival, and contraindications for beta blockade were noted. Unless contraindicated, a single dose of metoprolol was administered orally 1 hour before data acquisition in patients with a HR of ≥65 beats/min according to a predefined medication protocol. After 1 hour, the HR was remeasured. A total of 283 patients (53%) had a HR of ≥65 beats/min. In this group, beta blockade was contraindicated in 46 patients (16%). Metoprolol was administered to the remaining 237 patients. However, 26 patients (11%) received suboptimal (lower dose than prescribed by protocol) beta blockade because of contraindications. Of the 211 patients receiving optimal beta blockade, 57 (27%) did not achieve the target HR. Of the patients with contraindications to beta blockade, 43 (60%) did not achieve the target HR. Compared to patients with optimal HR control, those receiving no or suboptimal beta blockade because of contraindications had significantly fewer examinations of good image quality (40% vs 74%, p <0.001), and significantly more examinations of poor image quality (20% vs 6%, p <0.001). In conclusion, most patients require HR reduction before CTA. Contraindications to beta blockade are present in a substantial proportion of patients. This results in suboptimal HR control and image quality, indicating the need for alternative approaches for HR reduction.
To achieve heart rate (HR) control, beta-blocking medication is routinely administered, either orally or intravenously, before multidetector computed tomographic coronary angiography (CTA) examination. Beta-blocking medication lengthens the diastolic interval, during which the heart is relatively motion free and, thereby, reduces cardiac motion artifacts. In addition, beta blockade reduces the HR variability. At present, however, limited data are available concerning the prevalence of contraindications for beta blockade, as well as its efficacy, in a general population referred for CTA. Therefore, the present study assessed the use and contraindications of oral beta blockade before CTA and evaluated the effect on image quality.
Methods
In consecutive patients clinically referred for CTA, information on HR before and during CTA, as well as beta-blocking medication use, were recorded. A total of 537 patients (298 men and 239 women, mean age 56 ± 18 years) were enrolled. The exclusion criteria for CTA investigation were (1) (supra)ventricular arrhythmias, (2) renal insufficiency (glomerular filtration rate <30 ml/min), (3) known allergy to iodine contrast material, (4) severe claustrophobia, and (5) pregnancy. The main clinical characteristics of the study population are listed in Table 1 .
| Characteristic | Value |
|---|---|
| Gender (n) | |
| Male | 298 |
| Female | 239 |
| Age (years) | 56 ± 18 |
| Current smoker | 84 (16%) |
| Positive family history for coronary artery disease ⁎ | 194 (36%) |
| Hypertension † | 323 (60%) |
| Hypercholesterolemia ‡ | 249 (46%) |
| Diabetes mellitus | 128 (24%) |
| Previous percutaneous coronary intervention | 49 (9%) |
| Previous myocardial infarction | 33 (6%) |
| Previous coronary artery bypass grafting | 32 (6%) |
| Use of chronic medication | |
| Beta blockade | 217 (40%) |
| Diuretic | 97 (18%) |
| Statin | 187 (35%) |
⁎ Defined as presence of coronary artery disease in first-degree family members at <55 years old in men and <65 years old in women.
† Defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or antihypertensive medication use.
‡ Serum total cholesterol ≥230 mg/dl and/or serum triglycerides ≥200 mg/dl or treatment with lipid-lowering drugs.
The baseline HR and blood pressure (BP) were evaluated manually in all subjects on arrival, 1 hour before the scheduled CTA examination. Contraindications for beta blockade were noted. The absolute contraindications were low BP (defined as a systolic BP <100 mm Hg), severe chronic obstructive pulmonary disease (defined as GOLD stage III or IV), severe aortic valve stenosis (defined as aortic valve area <1.0 mm 2 ), reduced left ventricular ejection fraction (defined as an ejection fraction <35%), second- or third-degree atrioventricular block and known allergy to metoprolol. In addition, for patients already receiving high-dose beta-blocking medication (defined as >100 mg metoprolol or an equivalent dose of another beta-blocking agent) as a part of their baseline medication at CTA, additional beta-blocking medication was contraindicated. Unless contraindicated, a single dose of metoprolol was administered orally 1 hour before data acquisition in patients with a HR of ≥65 beats/min. The administered dose before CTA was determined according to a predefined beta-blocking medication administration protocol. Patients with a HR of 65 to 75 beats/min received 50 mg metoprolol, and patients with a HR of ≥75 beats/min received 100 mg metoprolol. However, patients already using low-dose beta-blocking medication as a part of their baseline medication (defined as <100 mg metoprolol or an equivalent dose of another beta-blocking agent) and patients with mild to moderate chronic obstructive pulmonary disease (defined as GOLD stage I or II) were considered to have relative contraindications to beta blockade. In these subjects, additional beta-blocking medication before CTA was administered at a lower dose, classified as a suboptimal dose of beta-blocking medication. Finally, in the case of anxiety, 1 mg of lorazepam was administered orally. After 1 hour, the HR was re-evaluated. The target HR, which was also the threshold for beta-blocker administration, was defined as an average HR of <65 beats/min.
CTA was performed using 2 different systems: a 64-row scanner (Aquilion 64, Toshiba Medical Systems, Otawara, Japan) and a 320-row scanner (Aquilion ONE, Toshiba Medical Systems) with 64 and 320 simultaneous detector rows, respectively (each 0.5-mm wide). The total amount of nonionic contrast media (Iomeron 400, Bracco, Milan, Italy) injected into the antecubital vein was 60 to 100 ml (depending on body weight and scanner type) at a flow rate of 5.0 or 6.0 ml/s, followed by a saline flush of 25 to 50 ml. To synchronize the arrival of the contrast media, bolus arrival was detected using a real-time bolus tracking technique. All images were acquired during a single inspiratory breath-hold of 12 seconds maximum. During the scan, the electrocardiogram was registered simultaneously for retrospective (64-row CTA) or prospective (320-row CTA) gating of the data. For 64-row CTA, the additional scan parameters were a 400-ms gantry rotation time, 120-kV tube voltage, and 300 to 350 mA (depending on bodyweight and thoracic anatomy). For 320-row CTA, the scan parameters were a 350-ms gantry rotation time, 120 to 135-kV tube voltage, and 400 to 580 mA (depending on bodyweight and thoracic anatomy). The average investigation time for CTA was approximately 20 minutes. No complications occurred because of beta-blocker administration.
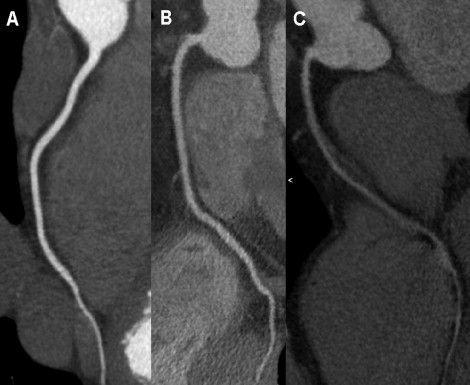
The computed tomographic coronary angiographic reconstructions were transferred to a remote workstation with dedicated analysis software (for 64-row CTA: Vitrea 2, Vital Images, Minnetonka, Minnesota; for 320-row CTA: Vitrea FX 1.0, Vital Images). The assessment of image quality of each CTA study was conducted on a per patient basis. When multiple reconstructions from different cardiac phases were available, the reconstruction with the best image quality was evaluated. The image quality was assessed using a 3-point grading scale ( Figure 1 ): (1) good image quality (no artifacts), (2) moderate image quality (moderate image degradation), (3) poor image quality (severe image degradation). Computed tomographic coronary angiographic analysis was performed by 2 experienced observers who unaware of the medication used and the patient’s HR.
Quantitative data are expressed as the mean ± SD and compared using the paired 2-tailed Student t test. Categorical variables are described as percentages. The comparison of image quality between groups and between systems was performed using chi-square analysis. p Values <0.05 were considered statistically significant.
Results
In the total population referred for CTA (n = 537), the mean baseline HR was 67 ± 13 beats/min. At arrival, 254 patients (47%) had a baseline HR that was less than the target HR and did not require HR reduction. In contrast, 283 patients (53%) had a baseline HR greater than the target HR and required HR reduction. In the latter group, 98 patients (35%) were already using beta blockade as a part of their baseline medication. Of the 283 patients requiring HR reduction, beta blockade was contraindicated in 46 (16%). The contraindications were low BP (n = 18), high-dose beta blockade as a part of their baseline medication (n = 17), severe chronic obstructive pulmonary disease (n = 5), severe aortic valve stenosis (n = 4), and reduced left ventricular ejection fraction (n = 2).
Metoprolol was administered to the remaining 237 patients (84%) requiring HR reduction. Of these 237 patients, 157 received 50 mg metoprolol and 80 received 100 mg metoprolol. However, of the 237 patients receiving beta blockade, 26 (11%) received suboptimal beta blockade because of relative contraindications. Specific relative contraindications included low-dose beta blockade as a part of their baseline medication (n = 23) and mild to moderate chronic obstructive pulmonary disease (n = 3). No adverse effects were seen from beta-blocking medication administration. In addition, 22 patients (4%) received 1 mg lorazepam.
Of the 254 patients with a baseline HR <65 beats/min, 37 (15%) did not remain at less than the target HR at the investigation. In 9 of these patients, the increased HR was caused by atrial fibrillation. Of the 211 patients receiving optimal beta blockade in the absence of contraindications, 57 (27%) did not achieve the target HR. In contrast, of the patients receiving no or suboptimal beta blockade because of contraindications, 43 (60%) did not achieve the target HR.
Immediately before data acquisition, 25 patients (5%) were excluded from CTA examination because of atrial fibrillation (n = 14), inadequate HR reduction (n = 9), or irregular HR because of frequent ventricular extrasystoles (n = 2). Accordingly, CTA was performed in 512 patients (95%; 64-row scanner, n = 311; 320-row scanner, n = 201). The mean HR at baseline and during CTA in patients with and without contraindications to beta blockade are shown in Figure 2 . Good or moderate image quality was achieved for 472 patients (92%) scanned and poor image quality was achieved for 40 patients (8%).
In the presence of contraindications to beta blockade, the overall computed tomographic angiographic image quality was decreased compared to patients without contraindications. In patients without contraindications to beta blockade, 334 scans (74%) were of good image quality, 88 (20%) were of moderate image quality, and 28 (6%) were of poor image quality. In contrast, in the presence of contraindications to beta blockade, 25 scans (40%) were of good image quality, 25 (40%) were of moderate image quality, and 12 (20%) were of poor image quality. Thus, optimal HR reduction using beta-blocking medication was associated with a significant improvement in image quality ( Figure 3 ). In a separate analysis, the results were compared between the data obtained with 64-row and 320-row CTA, indicating no significant differences in the distribution of image quality for patients with and without contraindications to beta blockade (chi-square = 1.786, p = 0.41).




