The prevalence of left ventricular noncompacted myocardium (LVNC) is not clearly defined yet. The goal of this study was to prospectively assess the prevalence of LVNC in a population of patients assessed for cardiovascular disease and to analyze the coincidence between observers using the echocardiographic criteria for diagnosis of LVNC. We included patients prospectively during a 1-year period. To analyze the concordance between different observers, we performed a blind analysis of 50 patients between 7 operators to calculate Kappa index for each criteria. The analysis of concordance for final diagnosis of LVNC was free-marginal kappa: 0.94. A total of 10,857 patients underwent echocardiography; 2,931 (27%) were normal. LVNC was found in 26 patients (prevalence = 0.24%), 16 patients were women, mean age of 52.6 years. Patients were divided into 2 groups; group A: ejection fraction (EF) <50% (n = 20) and group B: normal systolic function (n = 6). Among abnormal studies, 294 (2.7%) were dilated cardiomyopathies (DCs) Patients with LVNC and EF <50% comprised 6.8% of DC (20 of 294) and 24% (20 of 75) of patients with idiopathic DC (p <0.0001). Group A patients were older and with less presence of women (both p <0.05). In conclusion, the prevalence of LVNC in a population assessed for cardiovascular diseases is low. In contrast, it is very high in the subgroup of patients with idiopathic DC. The group of patients with LVNC and normal LVEF is younger and with a higher presence of women than those with LVNC and depressed LVEF. Coincidence between operators is very good for the identification of echocardiographic criteria.
Ventricular noncompaction (NC) is a primary muscle disease which affects the left ventricle and results from arrest of maturation of the fetal myocardium. This is deemed a distinct form of cardiomyopathy whose pathophysiology can mimic either a hypertrophic or a dilated cardiomyopathy. Its origin is unknown and however is associated with many ill-defined genetic abnormalities, besides familial clustering and isolated cases are reported in otherwise healthy children and young adults. Left ventricular noncompacted myocardium (LVNC) is a phenotypic diagnosis based on a set of criteria by the transthoracic echocardiography. Despite these inherent limitations, echocardiographic diagnosis of LVNC is still considered the gold standard for diagnosis. There are no population-based studies in adults to determine the prevalence of LVNC, and hence, this may potentially lead to underestimation of its prevalence in adults. Short of population screening, prospective detection of LVNC during echocardiography obtained for other reasons is a reasonable way to estimate its prevalence including coexistence with other cardiac diseases. The purpose of this study was to prospectively identify LVNC in adults through transthoracic echocardiography primarily obtained for various other cardiac reasons.
Methods
Prospective case-control study that includes all subjects who underwent a transthoracic echocardiogram at the Instituto Cardiovascular de Buenos Aires, from March 1, 2009, to March 1, 2010. We included only the first echocardiogram in subjects who had more than one study performed during this period. Staff physicians were trained in the use of the diagnostic criteria for LVNC before the initiation and launch of this project (before March 1, 2009). The criteria were printed and displayed in every echocardiographic examination room to prospectively detect LVNC and save appropriate video clips from each study. In ICBA’s echocardiography laboratories, the scans are performed by cardiologists with technicians assisting in capturing the video clips, still frames, and measurements. Echocardiographic examinations were performed using different ultrasound machines (IE 33, Sonos 7500, HD 15; Philips, Andover, Massachussets), and all of which were equipped with second harmonics, wide band transducers of various frequencies, color Doppler, and digital archiving systems with capabilities to transfer images to an image management and archiving system (PACS Estensa Ebit Esaote Italy) for later review.
All echocardiographic examinations were carried out with transducers appropriate for the patient’s age and body habitus that allowed better spatial resolution. Needed care was taken to obtain views from standard precordial windows. In addition to performing a complete study, we obtained the following measurements: LV dimensions in M-mode (left ventricular end diastolic diameter, left ventricular end systolic diameter), LV ejection fraction (EF) by Simpson’s single-plane formula, left atrial (LA) area at end systole in apical 4-chamber view. Diastolic LV function was assessed with transmitral pulsed Doppler flow to measure E and A waves and the tissue Doppler in the lateral portion of the mitral annulus to measure e′ and a′ waves to calculate the E/e′ ratio for estimation of LV end-diastolic pressure.
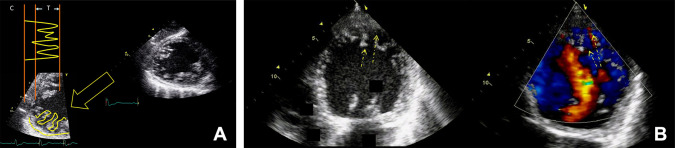
We used the following diagnostic criteria among the many proposed in the studies. First, the measurements of the trabeculated (T) inner layer of the ventricular wall and outer compact myocardium (C), the ratio (T/C) ≥2.3:1 in end diastole, as proposed by Jenni et al and Petersen et al, and second, the presence of color flow between the trabeculae especially during diastole, and we considered a positive diagnosis of LVNC when these 2 criteria were present in 4 or more LV wall segments which represented 25% of total number of LV segments according to the ASE segmentation ( Figure 1 ). All echocardiographic images were saved under predetermined diagnostic codes, including all the possible diagnoses in the clinical cardiology practice. In this report, we used the principal diagnosis according to the operator criteria. To analyze the concordance between different observers for the diagnosis of noncompaction myocardium and for each diagnostic criterion, we performed a random and blind analysis of the DICOM data in 50 patients (including 8 patients with LVNC) between 7 operators, to calculate Kappa index for each criteria and for final diagnosis of LVNC.
All patients with diagnosis of LVNC were followed up during 4 years through periodic telephone calls to obtain information related to adverse outcomes including death, systemic embolic events, arrhythmias, cardiac transplantation, ICD implantation for secondary prevention or hospitalizations for the previously mentioned or other cardiac causes.
Median and percentiles were calculated for all continuous variables and compared using the Student t test, and after a kurtosis analysis, parameters with normal distribution were calculated for median and SD. Prevalence was calculated as a percentage of cases with LVNC among the different populations considered. Concordance between different observers was measured using Fleiss’ Kappa index as free-marginal Kappa and median of different paired comparisons.
The concordance for the different diagnostic criteria were as follows: mean kappa 0.94 between 7 observers; Kappa: 0.84 for each of the 2 diagnostic criteria; ratio of the T/C layers ≥2.3:1 at end diastole: kappa: 0.67, mean kappa: 0.39; color flow between the trabeculae: kappa: 0.84, mean Kappa: 0.43; the number of LV segments involved kappa: 0.88, mean Kappa: 0.54.
Results
There were 10,857 echocardiograms performed that constituted the study group, of which 7,926 (73%) were abnormal and 2,931 (27%) were normal studies. The distribution of different diseases diagnosed by echocardiography is depicted in Table 1 . Twenty-six cases of LVNC were detected using the aforementioned diagnostic criteria giving an estimated prevalence of 0.24% for our cohort. Sixteen were women and 10 men; their median age was 52.6 years; range 13 to 86 years. Twenty-four of 26 cases showed isolated LVNC, whereas the remaining 2 showed an atrial septal defect of ostium secundum type. The distribution of segments with LVNC criteria was as follows: LV apex in 24 of 26 cases (92%), lateral wall in 21 of 26 (81%), and the inferior and/or posterior walls in 19 of 26 (73%); the anterior basal, midbasal, and anterior septal walls were not affected.
| Diagnosis | Number of Cases | Percentage of Total |
|---|---|---|
| Normal | 2925 | (27 %) |
| Isolated Diastolic Dysfunction and LA Enlargement | 2343 | (21.6 %) |
| Hypertensive Cardiopathy | 1731 | (15.9 %) |
| Coronary Artery Disease | 1077 | (9.9 %) |
| Heart Valve Disease | 747 | (6.9 %) |
| Dilated Cardiomyopathy | 274 | (2.7 %) |
| Hypertrophic Cardiomyopathy | 135 | (1.2 %) |
| Congenital Heart Disease | 87 | (0.8 %) |
| Other Diagnosis | 1478 | (13.5 %) |
| Bad Quality Echos | 34 | (0.31 %) |
| Left Ventricular Non Compaction | 26 | (0.24 %) |
| Total Abnormal Echos | 7926 | (73 %) |
| Total Population | 10857 | (100 %) |
To further study their clinical and demographic characteristics, we divided the cohort of LVNC into 2 distinct subgroups based on their baseline LV systolic function; EF ≤50% versus >50%. Of the 26 cases of LVNC, 20 showed an LV ejection fraction (LVEF) ≤50% (mean LVEF 32 ± 7.8%) and constituted group A, the remaining 6 showed an LVEF >50% (59 ± 6.2%) and constituted group B. Their mean age was different: group A 58 ± 12.4 versus 37.5 ± 20.8 years for group B (p <0.04); the gender distribution was different with an even distribution of M:F ratio for group A versus all women in group B (p <0.05). The comparison of echocardiographic parameters obtained by M-mode and 2-dimensional echocardiography for these subgroups is presented in Table 2 . The number of segments affected and fulfilling the diagnostic criteria was similar among the 2 subgroups, as well as the distribution of segments fulfilling the diagnostic criteria, 4.94 ± 1.53 for group A versus 4.33 ± 0.52 for group B (p = NS). The E/e′ ratio was 12.3 ± 6.8 in group A and 7.5 ± 1.29 in group B (p <0.05), the LA area was 22.52 ± 4.85 cm 2 in group A and 12.5 ± 6.19 cm 2 in group B (p <0.05).
| Patient | Age (years) | Sex | T/C (ratio) | LVEF (%) | LVEDD (mm) | LVESD (mm) | TR (0-4+) | LA (cm2) | E/e′ (ratio) | MR (0-4+) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 45 | M | 4 | 20 | 78 | 68 | 1 | 26 | 15 | 1 |
| 2 | 62 | M | 3 | 22 | 87 | 73 | 1 | 30 | 11 | 1 |
| 3 | 53 | M | 2.6 | 24 | 76 | 59 | 1 – 2 | 24 | 7 | 2 |
| 4 | 32 | M | 2.5 | 25 | 68 | 54 | 1 | 23 | 9 | 1 |
| 5 | 56 | M | 2.3 | 25 | 58 | 43 | 0 | 21 | 7 | 1 |
| 6 | 55 | M | >3 | 30 | 60 | 38 | 1 | 23 | 10 | 1 – 2 |
| 7 | 71 | M | 2.3 | 30 | 67 | 39 | 0 | 22 | 11 | 1 |
| 8 | 72 | F | 2.4 | 30 | 66 | 52 | 1 | 32 | 8 | 2 |
| 9 | 62 | F | 2.3 | 31 | 60 | 39 | 1 | 15 | 16 | 1 |
| 10 | 59 | M | 2.4 | 34 | 60 | 35 | 0 | 21 | 10 | 2 |
| 11 | 55 | F | 2.3 | 35 | 65 | 60 | 2 | 26 | 30 | 4 |
| 12 | 60 | F | 2.5 | 35 | 61 | 36 | 1 | 24 | 19 | 2 – 3 |
| 13 | 66 | F | 2.4 | 35 | 54 | 43 | 0 | 23 | 17 | 1 |
| 14 | 86 | M | 2.3 | 36 | 64 | 40 | 2 – 3 | 21 | 12 | 2 |
| 15 | 56 | F | 2.3 | 38 | 60 | 52 | 1 | 23 | 9 | 1 |
| 16 | 40 | M | 2.3 | 47 | 56 | 27 | 0 | 16 | 10 | 1 |
| 17 | 56 | F | 3.5 | 48 | 49 | 36 | 1 | 14 | 7 | 1 |
| 18 | 48 | F | 2.5 | 50 | 50 | 38 | 0 | 11 | 8 | 0 |
| 19 | 33 | F | 3.1 | 58 | 43 | 27 | 0 | 14 | 7 | 0 |
| 20 | 72 | F | 3.5 | 58 | 40 | 21 | 1 | 17 | 9 | 1 |
| 21 | 37 | F | 2.5 | 59 | 50 | 27 | 0 | 9 | 6 | 0 |
| 22 | 13 | F | 2.6 | 62 | 40 | 29 | 0 | 15 | 5 | 0 |
| 23 | 22 | F | 2.4 | 69 | 44 | 27 | 1 | 9 | 7 | 0 |
| 24 | 23 | F | 2.4 | 50 | 34 | 50 | 0 | 16 | 7 | 0 |
| 25 | 32 | M | 2.3 | 48 | 30 | 50 | 0 | 15 | 8,4 | 0 |
| 26 | 59 | M | 2.5 | 29 | 58 | 50 | 1 | 38 | 15 | 1 |
| Median St Dev | 52.6 Range (13-86) | 3.5±0.7 | 39.5±13.3 | 56.8±13.5 | 43±13 | 19.05±7.1 | 15±5.3 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


