Chapter 82
Erectile Dysfunction
Boback M. Berookhim, John P. Mulhall
Based on a chapter in the seventh edition by Ralph G. DePalma
Erectile dysfunction (ED) is the recurrent or consistent inability to obtain or to maintain a penile erection sufficient for satisfactory sexual performance.1 A common problem with significant negative effects on the quality of life of both the patient and his partner, it is associated with poor relationship satisfaction, negative general health perceptions, and role limitations due to physical and emotional problems.2
Epidemiology
Estimates on the prevalence of ED vary; however, it is estimated that at least 20 million men in the United States experience the condition.3 The Massachusetts Male Aging Study has reported a combined prevalence of ED in 52% of men older than 40 years, with an increase in the rate of moderate dysfunction from 17% to 34% and of complete ED from 5% to 15% between the ages of 40 and 70 years, respectively.4 Another study, looking at data from the National Health and Nutrition Examination Survey, reported a combined prevalence of ED in 18% of men older than 20 years, with an increase from 7% of the population between the ages of 20 and 29 years to 78% of those older than 75 years.5 The prevalence of ED appears to be similar among different ethnic groups; a different population-based study demonstrated a 22% rate of ED in white men older than 40 years, 24% rate among black men, and 20% rate among Hispanic men.6 Differences noted in the prevalence rates across these studies are partially due to nonstandardized definitions of the severity of ED, especially given the frequently subjective nature of this reported complaint.
Physiology of Penile Erection
The penis is a composite structure: the paired corpora cavernosa dorsally and the ventral corpus spongiosum, which contains the urethra. The corpora cavernosa are surrounded by the tunica albuginea, a bilayered structure that supports the cavernous tissue and provides the flexibility, rigidity, and strength of the penis. The spongiosum lacks the outer layer of the tunica, allowing a low-pressure urethra during erection. Blood flow to the penis typically originates from the internal pudendal artery, a branch of the internal iliac artery. Distally, it then becomes the common penile artery, where it subdivides into the dorsal, cavernosal, and bulbourethral arteries. Accessory pudendal arteries, arising from the external iliac, obturator, vesical, and femoral arteries, frequently contribute significantly to the arterial supply to the penis.7 The cavernosal arteries affect tumescence of the penis and end at the helicine arteries, which open into the endothelium-lined lacunar spaces. Venous drainage begins within the lacunar spaces, which drain into subtunical venules and emerge as emissary veins. The deep venous system continues with these emissary veins draining into the cavernosal, deep dorsal, or spongiosal veins until they join either the prostatic venous plexus or the internal pudendal veins. Superficial veins coalesce to form the superficial dorsal vein, which drains into the great saphenous veins (Fig. 82-1).
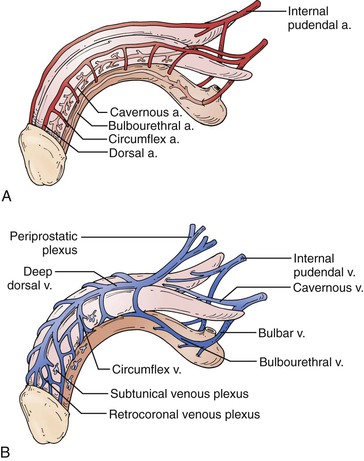
Figure 82-1 Penile vascular anatomy. A, Penile arterial supply. B, Penile venous drainage. (From Wein AJ: Campbell-Walsh urology, ed 10, Philadelphia, 2011, Saunders Elsevier, pp 691-692.)
Erection is the result of an integrative physiologic complex of psychologic, neuronal, hormonal, vascular, and cavernous smooth muscle systems that begins in the brain. Relevant innervation to the penis includes the somatic nerves, responsible for sensation and contraction of the bulbocavernosus and ischiocavernosus muscles, and the parasympathetic and sympathetic autonomic nerves located at levels S2-4 and T12-L2, respectively, which are instrumental in tumescence. These segments form the hypogastric and pelvic plexuses. Those fibers that innervate the penis compose the cavernous nerve, which travels along the posterolateral aspect of the prostate and then accompanies the membranous urethra through the urogenital diaphragm.8 The cavernous nerves then innervate the helicine arteries and trabecular smooth muscle.9
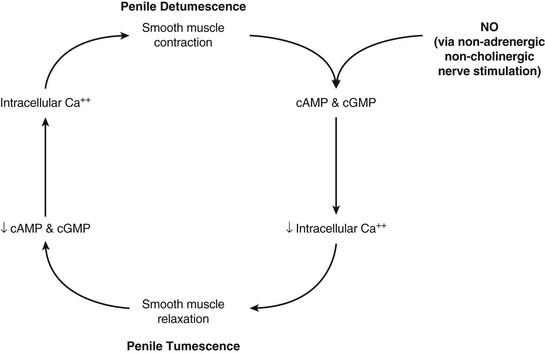
The cavernous smooth muscle plays a key role in erectile function and remains contracted in the flaccid state of the penis under α-adrenergic control. The erectile process begins with sexual stimulation, which increases parasympathetic activity and stimulates the release of neurotransmitters from cavernous nerve terminals or from the endothelium of the cavernosal arteries, resulting in relaxation of the penile smooth muscle.10,11 This is mediated by the nitric oxide (NO)/cyclic guanosine monophosphate (cGMP) pathway, ultimately resulting in increased blood flow through the penile arteries (Fig. 82-2).12,13 This blood flow then expands the sinusoids, compressing subtunical venules and peripheral sinusoids and ultimately reducing venous outflow (veno-occlusive mechanism). This leads to an increase in intracavernous pressure, resulting in an erection.
Pathophysiology of Erectile Dysfunction
Given the interaction of multiple different physiologic systems required for adequate erectile function, it is easy to appreciate that derangements in any one system can serve as a cause of ED. ED is classified according to its likely origin: psychogenic, neurogenic, endocrinologic, vasculogenic, and drug induced. It is often multifactorial in nature.
Psychogenic Erectile Dysfunction
Psychogenic (nonorganic) ED is generally assumed to be ED predominantly or exclusively related to psychologic or interpersonal factors.14 It is estimated to affect 10% to 15% of all men with ED. It has been further classified as situational psychogenic ED, which is noted to be partner related, performance related, or associated with psychologic distress, or generalized psychogenic ED, secondary to a lack of sexual arousability or a disorder of sexual intimacy.15 Psychogenic ED is an epinephrine-mediated phenomenon and is a diagnosis of exclusion, once physical (organic) factors have been ruled out. The clinical features include sudden-onset ED, with intermittency of function or a situational nature to the erectile problems, and good nocturnal erections.16
Neurogenic Erectile Dysfunction
Neurogenic ED, an uncommon entity, is secondary to events disrupting central neural networks or the peripheral nerves involved in sexual function. It is further subclassified into supraspinal, spinal, and peripheral neurogenic ED.17 Supraspinal ED is generally caused by tumor, stroke, Parkinson’s disease, dementia, and temporal lobe epilepsy.17 Spinal causes include multiple sclerosis, spinal cord injury, transverse myelitis, myelodysplasia, and lumbar disk disease or surgery.17–19 Peripheral causes include diseases associated with lower motor neuron lesions, trauma, pelvic disease, and radical pelvic surgery.17 Pelvic surgery, particularly radical prostatectomy, has a high risk of cavernous nerve injury and has been demonstrated to have a significant effect on erectile function.20
Endocrinologic Erectile Dysfunction
Androgens, specifically testosterone, have been linked to sexual desire, orgasmic function, and erectile function. However, low serum testosterone concentration has not been clearly linked to the presence or severity of ED.21,22 Animal models have shown that testosterone is important in the regulation of the expression of NO synthase and phosphodiesterase type 5 (PDE5) inside the penis.23 Hyperprolactinemia, leading to the inhibition of luteinizing hormone, is associated with low libido and possibly ED. Profound hypothyroidism (low luteinizing hormone levels) and profound hyperthyroidism (high estradiol levels) may be associated with sexual dysfunction.
Vasculogenic Erectile Dysfunction
ED and cardiovascular disease share common risk factors, including hypertension, diabetes mellitus, hypercholesterolemia, obesity, and smoking, leading to the concept that ED is another manifestation of vascular disease.24 A large patient survey of more than 7500 patients with hypertension and diabetes demonstrated ED in 67% of patients with hypertension alone, 71% of patients with diabetes alone, and 78% of patients with both conditions.25 A Spanish study of more than 2400 patients has demonstrated each of these to be independently associated with ED, with age-adjusted odds ratios of having ED of 4.0 in diabetics, 1.58 in patients with hypertension, 1.63 in patients with high cholesterol, 2.63 in patients with peripheral vascular disease, and 2.5 among smokers.26 ED patients have also been noted to have significantly higher plasma levels of low-density lipoprotein compared with normal counterparts.27
The Princeton III consensus guidelines recognize ED as a strong predictor of cardiovascular disease and specifically of coronary artery disease.28 Data from a meta-analysis of prospective cohort studies evaluating ED and the risk of cardiovascular disease demonstrated a combined relative risk for men with ED of 1.48 for overall cardiovascular disease, 1.46 for coronary artery disease, 1.35 for stroke, and 1.19 for all-cause mortality.29 In addition, ED has been described as an independent marker of cardiovascular events and all-cause mortality after adjustment for age, weight, hypertension, diabetes, hyperlipidemia, and cigarette smoking.30 ED is also an independent predictor for peripheral arterial disease (odds ratio, 1.97), with a significant stepwise increase in prevalence of peripheral arterial disease with increasing severity of ED (28% of men with mild ED, 33% with moderate ED, and 40% with severe ED).31
Looking specifically at patients with comorbid ED and cardiovascular disease, a number of theories have been proposed to explain the pathophysiologic association between these two disease states. Given that atherosclerosis is a systemic disease, with all vascular beds affected to the same extent, the artery size hypothesis proposes that symptoms are manifested at different time points according to the diameter of the arterial blood supply.32 Accordingly, a 50% stenosis of the coronary arteries would amount to a nearly complete occlusion of the penile arteries despite an equal amount of total atherosclerotic plaque in both vessels. In addition to the flow-limiting stenosis, ED due to arterial insufficiency is related to lower oxygen tension in intracavernous blood.33 This has been associated with possibly decreased prostaglandin E1 and E2 formation, leading to transforming growth factor-β1–induced collagenization of cavernous smooth muscle.17,34 Increases in the connective tissue have been correlated with failure of the veno-occlusive mechanism required for good erectile function.35
Endothelial dysfunction serves as an additional link between ED and cardiovascular disease. NO produced by the endothelium is necessary for the increased flow and vasodilatation of the penile arteries, which is necessary for erection. In both ED and cardiovascular disease, a deficiency of NO is brought about by impaired production or increased degradation, thereby decreasing vasodilatation and modulation of smooth muscle cells and inhibiting cellular adhesion.36,37 Among ED patients without evidence of cadiovascular disease, endothelial dysfunction has been noted within the penile vasculature but not in the small arteries of the forearm, indicating that penile endothelial dysfunction may occur earlier than in other vascular beds.38
ED has also been demonstrated to be a strong predictor of subsequent cardiovascular events. Data from the Prostate Cancer Prevention Trial demonstrated that incident ED was associated with a 25% increased likelihood of subsequent cardiovascular events during the 5-year study follow-up and that men with incident ED during the study period were at a 45% increased risk of cardiovascular events.39 This association was similar to the risk associated with current smoking or a family history of myocardial infarction. Another study addressing men referred with ED and vasculogenic ED documented on penile ultrasonography demonstrated a 20% rate of abnormalities on stress echocardiography in cardiac evaluation.40
In addition to arterial causes, as indicated before, vasculogenic ED is also often the result of inadequate venous occlusion.41 Corporal veno-occlusive dysfunction may be caused by the development of large venous channels draining the cavernous tissue or be a result of degenerative or functional changes in the tunica albuginea, as is seen in Peyronie’s disease.42,43
Drug-Induced Erectile Dysfunction
Antihypertensives, psychotropics, and antiandrogens are the primary drug classes associated with ED. Among the antihypertensives, multiple studies have demonstrated significant increases in ED among patients receiving thiazides compared with placebo.44,45 Studies of β-adrenergic antagonists demonstrate mixed results with respect to their potentially causing ED; nonselective drugs, such as propranolol, show clear associations with ED, and agents with higher selectivity for the β1-adrenoreceptor, such as acebutolol, show a reduction in ED compared with placebo.46 Angiotensin receptor blockers have been consistently shown to have pro-erectile effects.47 Antidepressants, specifically selective serotonin reuptake inhibitors, can negatively affect all steps of the sexual response cycle, most notably ejaculatory latency. Differences are noted in the incidence of ED among different medications, with higher rates noted in patients taking paroxetine.48 Antiandrogens cause partial or complete blockade of circulating androgens either through inhibition of production or by antagonism at the level of the androgen receptor and are frequently used in the treatment of prostate cancer. Use of these medications is generally associated with decreased sexual desire, although medical castration with luteinizing hormone–releasing hormone agonists or antagonists and nonsteroidal antiandrogens such as flutamide and bicalutamide can also contribute to veno-occlusive dysfunction.49 Other classes of drugs associated with ED include 5α-reductase inhibitors (finasteride, dutasteride) and digoxin.50,51
Assessment of Erectile Dysfunction
History and Physical Examination
ED is often multifactorial in origin, and the initial evaluation of ED must include a complete medical, psychosocial, and sexual history.52 Care should be taken to assess for signs and symptoms of possible underlying conditions, with a detailed review of current medications, to identify possibly reversible and underlying treatable disorders causing ED. One study of more than 270,000 ED patients demonstrated a 68% prevalence of a significant underlying condition at the time of ED presentation.53
Given the often sensitive subject matter, clinicians should give consideration to use of validated questionnaires to ease into the conversation, including the International Index of Erectile Function (IIEF) and the abridged, five-item version of the IIEF, the Sexual Health Inventory for Men. These have been demonstrated to accurately diagnose and quantify the severity of the ED complaint.54,55 Descriptive measures should be used for rigidity and sustainability of erections during sexual arousal, intermittency or any situational aspect of erections, and presence of nocturnal erections to further define underlying causes of ED. Patients complaining of sudden-onset ED with loss of sustaining capability and strong nocturnal erections are more likely to have nonorganic ED secondary to psychogenic causes. Frequently, physical examination will not reveal a specific cause of ED. A general examination, with evaluation of blood pressure, heart rate, abdominal pulsations, peripheral pulses, and male secondary sex characteristics, including the presence of gynecomastia, and a focused genital examination should be performed.52,56 Attention should be paid to the absence of femoral pulses, possibly indicative of aortoiliac arterial occlusive disease. This can be a marker of decreased penile arterial flow through the hypogastric (internal iliac) arteries. Genital examination should include examination of the penis, specifically the size and position of the urethral meatus; determination of the presence of tunical plaques; evaluation of testicular size and consistency; and a digital rectal examination in the appropriately aged man.56
Laboratory Evaluation and Adjunctive Testing
According to the International Consultation on Sexual Medicine committee, recommended laboratory tests to confirm the presence of underlying diseases include fasting blood glucose concentration, lipid profile, and serum testosterone level, with optional examinations such as thyroid function testing based on the clinical scenario.52,56 The Princeton III consensus statement recommends that all men with organic ED older than 30 years be considered at increased cardiovascular disease risk until recommended checks suggest otherwise and further recommends resting electrocardiography and serum creatinine level in addition to the previously described testing in men without known cardiovascular disease.28 It also recommends, in consultation with a cardiologist or primary care physician, performance of a thorough noninvasive and, when indicated, invasive evaluation of cardiovascular disease status, including measurement of biomarkers, physiologic stress testing for ischemia, and anatomic clarification by coronary computed tomographic angiography.28
Nocturnal penile tumescence monitoring, to study nocturnal erectile quality, may be used both in a sleep laboratory setting and with a portable, home-use device such as the RigiScan (Timm Medical Technologies, Minneapolis, Minn).57 It allows the monitoring of rigidity, tumescence, and number and duration of erectile events.58 Testing, however, does not indicate the cause and severity of ED and does not evaluate wakeful, sexually relevant erections. In contemporary practice, its routine use for diagnostic purposes is significantly limited.
Vascular Evaluation
Vascular studies in the patient with ED are designed to define the presence of arteriogenic ED or veno-occlusive dysfunction.
Penile-Brachial Pressure Index
The penile-brachial pressure index (PBI) refers to the ratio of penile systolic pressure to brachial systolic pressure and has been used to evaluate for the presence of significant hemodynamic occlusions proximal to the penile arteries contributing to ED (e.g., in the aorta or iliac arteries). Penile systolic blood pressure is measured by applying a small pediatric blood pressure cuff to the base of the flaccid penis and measuring the systolic blood pressure with a Doppler probe. The validity of this technique in the evaluation of ED has been called into question, given significant interobserver variability, failure to measure pressure in the erect state, and concerns with false-positive diagnosis of arterial insufficiency. In a study of 88 patients referred for evaluation of claudication, the sensitivity of PBI to determine clinically meaningful arterial stenosis or occlusion in the hypogastric circulation was determined with use of angiography as the “gold standard.”59 By use of a receiver operating characteristic curve, the only area significantly different from random choice was the detection of bilateral occlusion with PBI. On the basis of analysis of the positive and negative predictive values, the authors reported an inability to discriminate normal from abnormal angiographic results using a PBI threshold of 0.6. Thus, its use in the evaluation of ED is primarily of historical significance.59,60
Office Injection Testing
Intracavernosal injection testing is performed by injection of a vasodilatory drug (or cocktail of drugs), combined with genital or audiovisual stimulation, in a clinical setting. The erectile response is then evaluated by a clinician to rate both rigidity and duration of response. Patients are monitored for detumescence while in the office after the test is performed, and those who do not spontaneously detumesce within 1 hour of injection are given intracavernous injections of a diluted phenylephrine solution. Vasodilatory medications used include prostaglandin E1 (PGE1) alone and a combination of medications including PGE1, papaverine, and phentolamine. Whereas intracavernosal injection testing has been used in an attempt to differentiate organic from psychogenic ED, it is now accepted that its only value is to define a functional veno-occlusive mechanism in men who develop a rigid and sustained erection.61
Failure to obtain a rigid erection may indicate vascular disease but may also be the result of an excessive sympathetic response associated with anxiety during intracavernosal injection testing.62 Currently, the intracavernosal injection test is seldom performed and generally considered obsolete.
Duplex Ultrasonography of the Penis
Doppler duplex ultrasound (DUS) of the penis is a reliable and noninvasive diagnostic method for evaluating ED that allows objective quantification of the blood flow to the penis. It provides a physiologic diagnosis to guide therapy in patients with a poor response to oral ED therapy, differentiates psychogenic from organic ED, aids in the evaluation of the young man with primary ED or a history of pelvic trauma, and suggests the need for cardiovascular evaluation in the man with vasculogenic ED without overt cardiovascular disease risk factors.63
Given the significant influence of psychologic and environmental factors on erectile function, Doppler DUS should be performed in a quiet and comfortable room, isolated from intrusion and other distractions. An erection is then pharmacologically induced by intracavernosal injection with vasoactive medications. If a good erection is not achieved, the dose should be repeated to ensure maximal smooth muscle relaxation for accurate interpretation of the results. Rigidity and sustainability of the erection are noted by the examiner. Doppler DUS is performed with a high-resolution linear array ultrasound transducer, with a frequency between 7.5 and 12 MHz. With the patient in the supine position, the penis is scanned and the location of the left and right cavernosal arteries is identified. Peak systolic velocity (PSV), end-diastolic velocity (EDV), and resistive index (RI) are measured. The penis is then evaluated with use of B-mode images to observe for the presence of tunical plaque (Peyronie’s disease), fibrosis, and calcification either in the vasculature or in the plaque itself.
Various criteria have been suggested for normal PSV values, but it is generally accepted that the patients with PSV below 25 cm/s have evidence of arteriogenic ED.64 This level has been noted to have a sensitivity of 100% and a specificity of 86% among patients with abnormalities on pudendal angiography.65 Use of values of 35 cm/s decreases the sensitivity to 76% but increases specificity to 92%.66 Significant asymmetry of PSV, with a difference of more than 10 cm/s between the right and left sides, suggests a significant atherosclerotic lesion or iatrogenic or surgical cause of a decrease in arterial flows.66 Veno-occlusive dysfunction is evaluated by EDV, in the presence of normal arterial inflow. In general, an EDV of greater than 5 cm/s is accepted as the measurement at which corporal veno-occlusive dysfunction is present (Fig. 82-3).63,66 Given concerns for the specificity of EDV alone for the diagnosis of corporal veno-occlusive dysfunction in patients with arterial insufficiency, RI has been used with a cut point of less than 0.75 as abnormal.63,67 However, RI, calculated as the difference between PSV and EDV divided by the PSV, is ultimately dependent on PSV. Patients with good arterial inflow and significantly elevated EDV may still have RI values within the normal range, and as such, RI alone should not be used for diagnostic purposes.
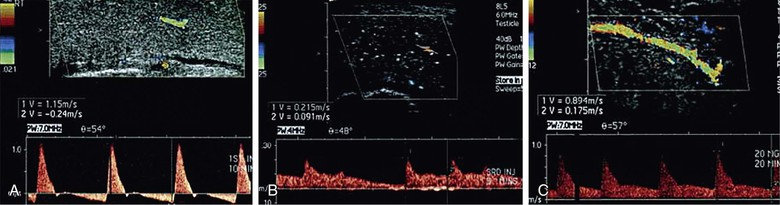
Figure 82-3 Color Doppler duplex ultrasound of the penis. A, Normal erectile hemodynamics: Doppler waveform analysis demonstrating cavernosal artery peak systolic velocity of 115 cm/s and end-diastolic velocity of −24 cm/s, representing normal erectile hemodynamics. B, Mixed vasculogenic erectile dysfunction: Doppler waveform analysis demonstrating cavernosal artery peak systolic velocity of 21.5 cm/s and end-diastolic velocity of 9.1 cm/s, indicating arterial insufficiency and corporal veno-occlusive dysfunction. C, Corporal veno-occlusive dysfunction: Doppler waveform analysis demonstrating cavernosal artery peak systolic velocity of 89.4 cm/s and end-diastolic velocity of 17.5 cm/s. End-diastolic velocity greater than 6 cm/s is an indication of corporal veno-occlusive dysfunction. (From Wilkins CJ, et al: Colour Doppler ultrasound of the penis. Clin Radiol 58:514-523, 2003.)
As described before, accurate assessment of penile hemodynamics requires maximal smooth muscle relaxation, ensuring that the sympathetic response (anxiety, stress) experienced with intracavernosal injection is minimized. As such, the patient’s erectile quality should be assessed throughout the examination and compared with the “bedroom quality erection,” which corresponds to the best erection hardness obtained at home without the use of a medication.68 Assessment of PSV and EDV in this situation is most likely to provide accurate results. Also, as noted, asymmetry between right and left PSV and EDV values must take erectile rigidity into account, as it is not uncommon to have a patient experience detumescence in the process of completing the study.
Dynamic Infusion Cavernosometry and Cavernosography
Dynamic infusion cavernosometry and cavernosography is the most accurate assessment of erectile hemodynamics. Given the widespread availability of Doppler DUS and the specialized equipment and training needed to perform dynamic infusion cavernosometry and cavernosography, its clinical use is limited. It is now generally used in young, healthy men with a history of perineal or pelvic trauma being considered candidates for penile revascularization; in young men with ED failing to respond to erectogenic pharmacotherapy, presumed to be secondary to corporal veno-occlusive dysfunction, and faced with penile implant surgery as their only option; in young men with primary ED (never had a rigid erection) to rule out corporal veno-occlusive dysfunction; in medicolegal cases in which a definitive diagnosis is needed; and in patients with Peyronie’s disease and comorbid ED, in whom the presence of corporal veno-occlusive dysfunction will ultimately change surgical management.69
Dynamic infusion cavernosometry involves placement of a butterfly needle in each corporal body, one connected to a pressure transducer and the other to a server-controlled pump for heparinized saline infusion.69,70 After the injection of vasoactive drugs (in doses significantly higher than those used for Doppler DUS), erection ensues, and a number of parameters are recorded: equilibrium pressure within the corpus cavernosum, which is an assessment of intracavernosal pressure development within the corpus cavernosum 10 to 15 minutes after vasoactive agent injection; cavernosal artery inflow gradient, which is the difference between the brachial artery systolic pressure and the cavernosal artery occlusion pressure, measured on both sides; flow to maintain, defined as the flow of saline required to maintain a given intracavernosal pressure; and pressure decay, the pressure drop occurring during a 30-second period after the intracavernosal pressure is raised to 150 mm Hg. The dose of the vasoactive agent is repeated as needed if flow to maintain or pressure decay values are abnormal.71 If the cavernosometry demonstrates corporal veno-occlusive dysfunction, cavernosography may be performed, in which nonionic radiopaque dye is injected intracavernosally and a radiograph is obtained to demonstrate the site of venous drainage.
Standardized data for results of dynamic infusion cavernosometry and cavernosography are not available. However, normal values are as follows: cavernosal artery occlusion pressure of less than 30 mm Hg, flow to maintain of less than 5 mL/min, and pressure decay of less than 45 mm Hg during 30 seconds.70 Whereas abnormal values aid in the diagnosis of corporal veno-occlusive dysfunction after dynamic infusion cavernosometry and cavernosography, additional data are available through the relationships between these parameters. Plotting the flow to maintain against the intracavernosal pressure graphically generates one of two patterns, a curvilinear pattern and a parabolic pattern. Patients with a linear pattern are generally accepted to have genuine evidence of corporal veno-occlusive dysfunction, whereas those with a parabolic pattern generally have abnormal veno-occlusive parameters secondary to excess sympathetic tone.69
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree