Chapter 10 Endovenous Approach to Recurrent Varicose Veins
Historical Background
Recurrence rates of varicose veins of 20% are common, with rates as high as 70% at 10 years.1–3 Up to 25% of procedures for varicose veins are performed for recurrent disease,4 thus placing considerable demands on health care resources. It is important to note that recurrent varicose vein surgery carries a much greater morbidity risk to the patient than does primary surgery.3 This risk is reduced markedly with endovenous techniques.
Etiology and Natural History of Disease
Patients who have had previous high ligation and stripping typically present with recurrent varicose veins; anatomic distribution of these veins is variable. Neovascularization is commonly seen following traditional stripping procedures and is thought to be secondary to “frustrated” venous drainage from the abdominal wall and perineum.5 Regardless of the mechanism, the result is recurrent reflux in the thigh or lower leg veins.
Pearls and Pitfalls
Previous High Ligation and Stripping
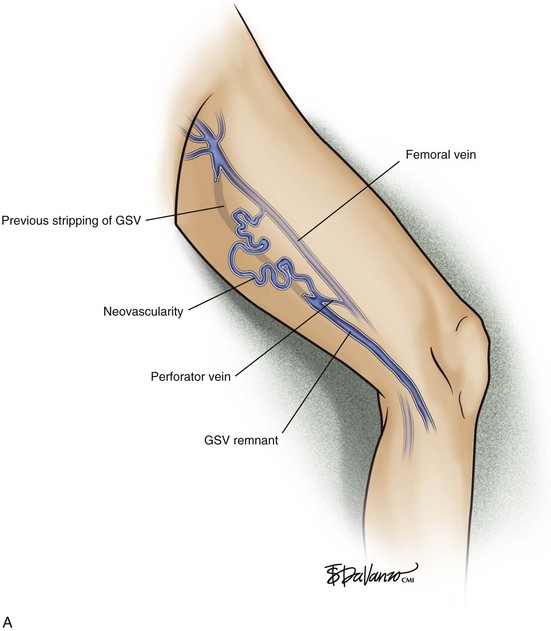
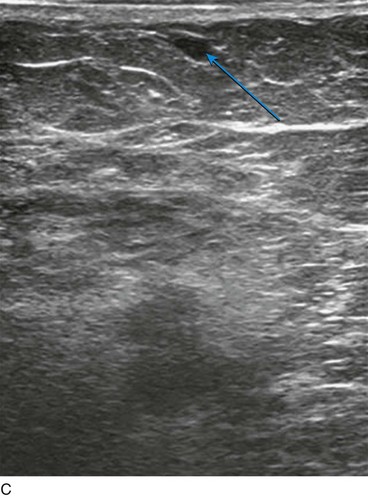
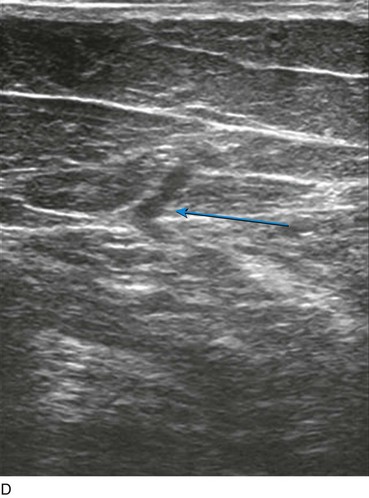
All patients with recurrent varicose veins should be evaluated with CFDI. Usually findings include neovascularity in the groin from which one or more tributary veins are found to descend the thigh. The tributary may attach to another tributary, a perforator, or a remnant of the great saphenous vein (GSV) in the thigh or calf (Fig. 10-1). The reflux extends into dilated tributaries of the skin; these vessels bulge and are palpable. In most cases, our approach is to enter any straight incompetent axial venous segments deep to the skin with a micropuncture access kit. These kits usually contain 4-Fr microsheaths, through which we place a 400- or 600-µm-diameter laser fiber. Perivenous tumescent anesthesia is placed, and the vein or veins are ablated in the usual manner. Because tortuous incompetent venous segments below the level of the skin do not allow the passage of guidewires, these are treated with ultrasound-guided foam sclerotherapy (Fig. 10-2).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree