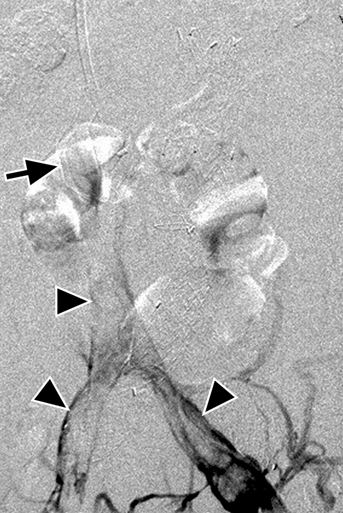
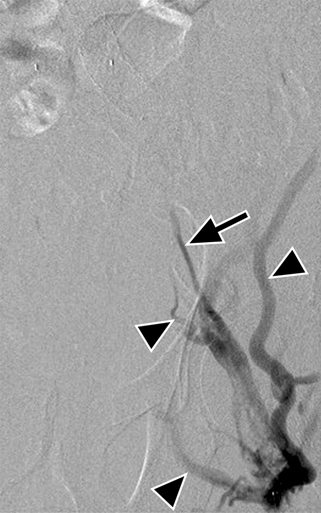
Contrast venography is performed after access has been obtained. This usually demonstrates multiple collaterals, which might or might not localize the thrombosed target vessel, depending on the site of injection, length of thrombosis, and point of recanalization. For this reason, it is usually best to start with an injection near the point of occlusion, with care not to advance the catheter into collaterals bypassing the obstruction. For example, in the cases of iliocaval occlusion, contrast injection at the saphenofemoral confluence will fill even the chronically thrombosed common femoral vein, as well as superficial body wall collaterals (Figure 1). The thrombosed target vein often appear as a threadlike channel, called a string sign, in the expected course of the iliac vein or IVC (see Figure 1). At this point, a catheter and guidewire are directed into the vein of choice. Uncomplicated recanalization proceeds by intermittent wire advancement, catheter passage, contrast injection to confirm intravenous location, and sheath advancement, all performed patiently and with a readiness to abandon pathways that do not look right or that repeatedly lead the catheter and wire into collateral pathways (Figure 2). In case of perforation of the thrombosed vessel wall and extravascular false passage of the catheter and wire, the catheter can be withdrawn until contrast injections reflux into venous structures, whereupon the catheter may be redirected and advanced by an alternative route. Occasionally, the thrombosed segment is so small or tight and the false passage is so prominent that attempts to redirect the catheter are fruitless. In these cases, it is best to retract the catheter into a confirmed intravascular location and attempt to complete recanalization from an alternate route.
Endovascular Treatment of Vena Cava Occlusion
Technique of Venous Recanalization
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine