Chapter 29 Endovascular Therapy for Infrapopliteal Arterial Occlusive Disease
Endovascular therapy (EVT) has increasingly become the initial clinical option for treating both claudication and critical limb ischemia (CLI).1 Similar to the evolution of open bypass surgery, EVT began above the knee and has been progressively extended to the infrapopliteal segment, now even including the pedal and arch vessels. Enthusiasm for infrapopliteal EVT was tempered by poor initial results,2 but advances in technique, equipment, and patient selection have led to improved outcomes and more widespread EVT application. This chapter discusses standard techniques for infrapopliteal EVT and reviews the contemporary results of tibial angioplasty, stenting, and atherectomy.
Patient Selection
The revised TransAtlantic Inter-Society Consensus (TASC II) guidelines provide the current consensus recommendations for EVT.3 TASC II guidelines do not delineate specific anatomic criteria for infrapopliteal disease and do not formally recommend infrapopliteal EVT, whereas previous TASC guidelines included anatomic criteria for infrapopliteal lesions (Table 29-1).4 TASC II guidelines mention growing evidence to support EVT for infrapopliteal occlusions in patients with comorbidities in whom in-line flow to the foot can be reestablished. In addition, the guidelines also point out that failed angioplasty does not usually preclude subsequent bypass. Graziani and colleagues5 also proposed a classification system for patients with CLI secondary to multilevel infrainguinal disease (Figure 29-1).5 Arterial lesions were graded class 1 to class 7, indicating progressive disease severity with decreasing transcutaneous oxygen tension (TcPO2).
TABLE 29-1 TASC I Classification of Infrapopliteal Lesions
| Classification | Lesions Characteristics |
|---|---|
| TASC A | |
| TASC B | |
| TASC C | |
| TASC D |
PTA, Percutaneous transluminal angioplasty.
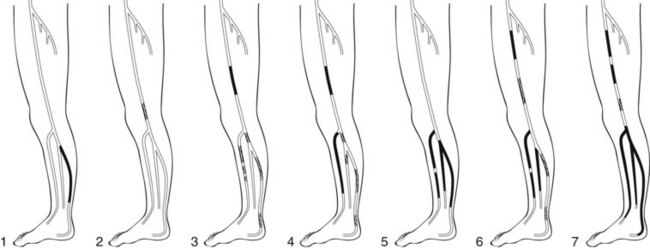
FIGURE 29-1 Graziani classification scheme for multilevel infrainguinal disease.
(From Graziani L, Silvestro A, Bertone V, et al: Vascular involvement in diabetic subjects with ischemic foot ulcer: a new morphologic categorization of disease severity. Eur J Vasc Endovasc Surg 33:453–460, 2007.)
Technique
Once the ipsilateral CFA has been accessed, a guidewire is manipulated anteromedially to cannulate the SFA. If this is not possible, the wire can be advanced down the profunda femoris artery, and a short, angled-tip catheter is advanced over the wire. Lateral anterior oblique positioning of the image intensifier helps to open the femoral bifurcation. The catheter is withdrawn slowly while puffing contrast until the femoral bifurcation is clearly demonstrated. The catheter tip is steered medially and anteriorly toward the SFA, and the guidewire is advanced into the SFA (see Figure 28-3). The access sheath diameter is typically 5 French, although tibial angioplasty with 0.014- and 0.018-inch platforms can be performed through a 4-French sheath. If an up-and-over approach is used, a long sheath with its tip in the popliteal artery facilitates tibial interventions.
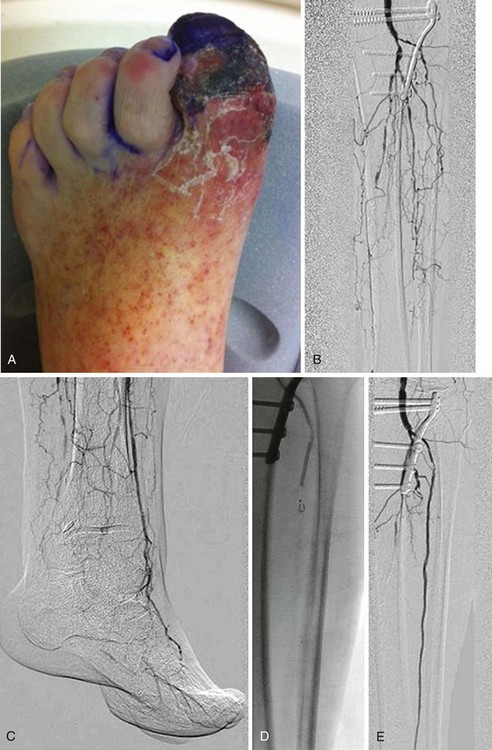
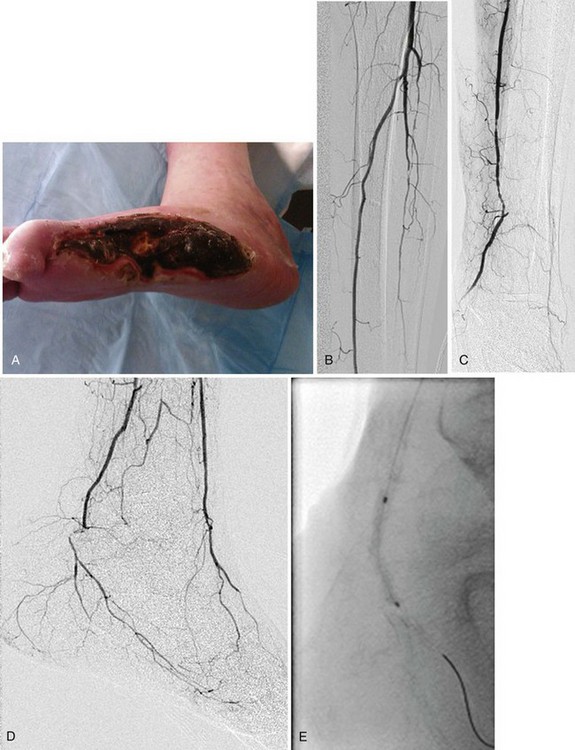
Subintimal angioplasty is a useful technique first described by Bolia and coworkers6 in 1989 for the treatment of long-segment femoropopliteal occlusions.6 This technique may also be successfully applied to infrapopliteal lesions as well (Figure 29-2, see color insert). A wire is used to intentionally create a subintimal dissection plane just proximal to an occlusion. The wire is typically formed into a short J shape and is advanced in the subintimal plane until the occlusion has been passed. If reentry into the true lumen is difficult, it may be facilitated by a special reentry device, such as the Outback LTD catheter (Cordis) or Pioneer catheter (Medtronic, Minneapolis, Minn.).
Once a stenosis or occlusion has been crossed successfully, balloon angioplasty is possible (Figure 29-3, see color insert). Balloon angioplasty stretches the arterial wall causing plaque fracture and sometimes local dissection, which is usually not flow limiting. Treating long-segment tibial lesions with longer balloons is a useful technique, but some short, focal lesions require a shorter balloon with more directed dilation force. A cutting balloon (Boston Scientific), which features three to four microsurgical blades fixed longitudinally along the outer surface of a noncompliant balloon, is particularly useful for the intimal hyperplasia near graft anastomoses. Creating controlled cuts in the intima theoretically allows less vessel wall disruption, less neutrophil activation, and more controlled balloon dilation.7 Drug-coated balloons are another emerging technology.8
Stenting in the infrapopliteal segment has traditionally been reserved for obviating emergency surgery because of poor angioplasty results, such as a flow-limiting dissection. More recently, drug-eluting stents have been used for the treatment of infrapopliteal disease, with encouraging results.9 Other infrapopliteal maneuvers, such as atherectomy and cryotherapy, may add more cost than real benefit compared to angioplasty alone.10
Results
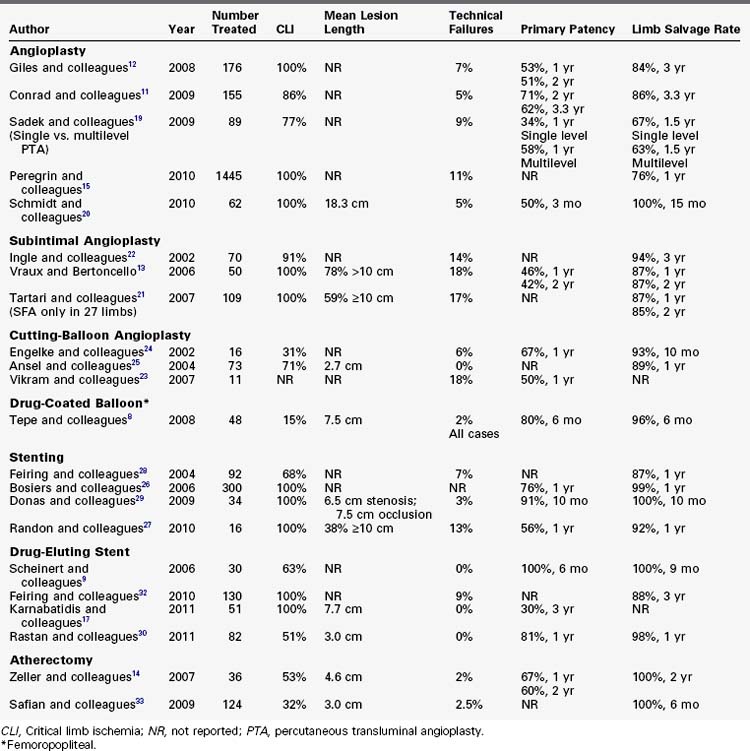
The outcome of infrapopliteal EVT depends on many factors, including indication for the procedure, lesion characteristics, runoff status, comorbidities, and technical factors, such as dissection or persistent stenosis (Table 29-2). Poorer outcomes appear to be predicted by the following factors: CLI versus claudication,11 longer lesion length,12–14 poor runoff status,11,12,15 comorbidities of diabetes16,17 and renal failure,11,18 smoking,17 and untreated intraprocedure flow-limiting dissection and persistent stenosis greater than 30%.
Angioplasty
Giles and associates12 retrospectively reviewed 163 consecutive patients (176 limbs) who underwent infrapopliteal EVT for CLI; 102 patients (58%) also had concomitant femoropopliteal angioplasty or stenting, or both12; and 97 lesions (55%) were TASC C or D. Subintimal angioplasty was performed only for complete occlusions that could not be crossed transluminally. The technical success rate was 93%, and 1- and 2-year primary patency rates were 53% and 51%, respectively. The 3-year limb salvage was 84%. On multivariate analysis, predictors of restenosis were TASC D lesions and lack of a bypass target, whereas multilevel intervention was protective. Sadek and colleagues19 retrospectively reviewed 85 patients (89 limbs) who underwent either single-level tibial (29 limbs) or multilevel (60 limbs) interventions. Overall, 77% of patients had CLI. The technical success rate was 91%, and 12- and 18-month primary patency rates were 34% and 27%, respectively, in the single-level interventions and 58% and 48%, respectively, in the multilevel interventions. The 12- and 18-month limb salvage rates were 75% and 67%, respectively, in the single-level interventions and 84% and 63%, respectively, in the multilevel interventions. The difference of primary patency and limb salvage between the two groups did not reach statistical significance. Peregrin and associates15 retrospectively reviewed 1268 patients (1445 limbs) who underwent infrapopliteal angioplasty for CLI. Almost all lesions were classified as TASC D. The technical success rate was 89%, and the primary and secondary limb salvage rates at 1 year were 76% and 84%, respectively. Interestingly, the number of patent infrapopliteal arteries at the end of angioplasty significantly correlated with 1-year limb salvage rates. As the number of patent crural arteries increased from 0 to 3, the 1-year limb salvage rate increased from 56% to 83%. Conrad and colleagues11 retrospectively reviewed 144 patients (155 limbs) who underwent infrapopliteal angioplasty; 133 limbs (86%) were treated for CLI, and 116 limbs (75%) had TASC C or D lesions. The technical success rate was 95%, and the 24- and 40-month primary patency rates were 71% and 62%, respectively. Multivariate analysis showed poor runoff, CLI, and dialysis as negative predictors of patency. The 40-month limb salvage rate was 86%; negative predictors of limb salvage included dialysis and failure to improve runoff.
Data are also available regarding angioplasty for long-segment infrapopliteal disease. Schmidt and coworkers20 studied 58 patients (62 limbs) with CLI who underwent infrapopliteal angioplasty for lesions 8 cm or greater in length.20 The technical success rate, defined by restoration of flow in at least one infrapopliteal vessel, was 95%. At short-term follow-up of 3 months, angiography demonstrated restenosis less than 50% in 31% of treated arteries, restenosis greater than 50% in 31%, and occlusion in 38%. Clinical improvement (wound healing or improvement of rest pain) was present in 76% of treated limbs. All arteries with restenosis greater than 50% or occlusion were retreated. At 15 months, 77% of limbs showed further clinical improvement, and the limb salvage rate was 100% without bypass.
Subintimal Angioplasty
Groups have also published specifically regarding subintimal angioplasty. Tartari and colleagues21 reported on 117 subintimal angioplasty procedures for complete occlusions, 82 (15 TASC C and 67 TASC D) of which were infrapopliteal. Technical success, defined as recanalization of at least one tibial vessel with adequate flow to the foot, was possible in 83% of cases. At a mean follow-up of 13.5 months, 12.5% of this cohort underwent major amputation and 11.3% underwent surgical bypass. Vraux and coworkers13 reviewed 46 patients (50 limbs) with CLI and tibial occlusions. Technical success was possible in 82% of cases. Primary patency was 46% at 12 months and 42% at 24 months. Limb salvage was 87% at 12 and 24 months. Longer lesion length and the need to extend treatment to the popliteal artery were associated with lower clinical patency rates. Ingle and colleagues22 retrospectively reviewed 67 consecutive patients (70 limbs) who underwent infrapopliteal angioplasty for occlusive lesions; 61 patients (91%) had CLI. The technical success rate was 86% and the limb salvage rate at 3 years by Kaplan-Meier life-table analysis was 94%.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree