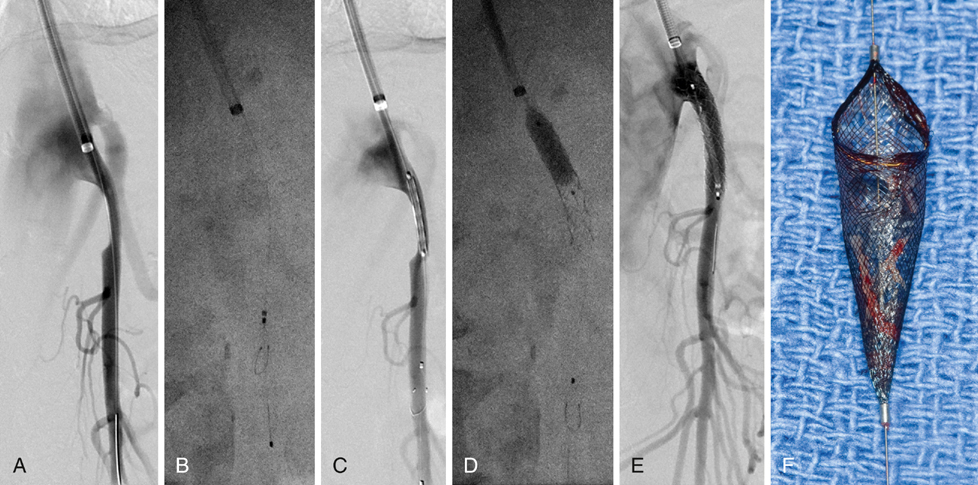
The target SMA lesion is initially crossed using a 0.035-inch soft Glidewire, which is exchanged for the interventional wire of choice after confirmation of true lumen access (Figure 1). The author’s preference is to use a small-profile (0.014- or 0.018-inch) stiff guidewire for most interventions. It is important to visualize the tip of the guidewire, which should be positioned within the main trunk of the SMA rather than within smaller side branches to avoid an inadvertent perforation or dissection. The author’s preference is to use embolic protection (e.g., 320-cm Spider RX filter wire) in patients with occlusions, long lesions (>30 mm), severe calcification, thrombus, and acute or subacute symptoms. If a longer 0.035-inch stent is used, the 0.014-inch filter wire is combined with a 0.018-inch buddy wire, and the stent is introduced via both wires for better support and to facilitate subsequent retrieval of the embolic protection device.
Endovascular Therapy for Chronic Mesenteric Ischemia
Treatment
Selection
Techniques
Diagnostic Angiography
Angioplasty and Stenting
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Endovascular Therapy for Chronic Mesenteric Ischemia
