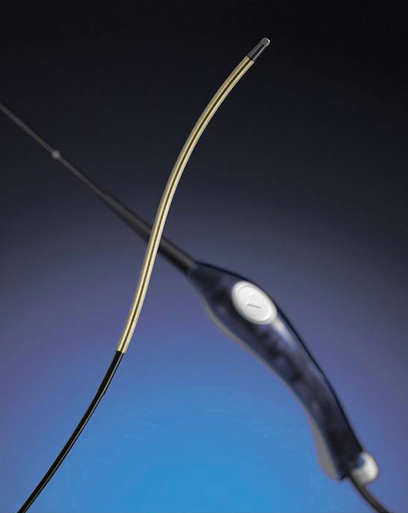
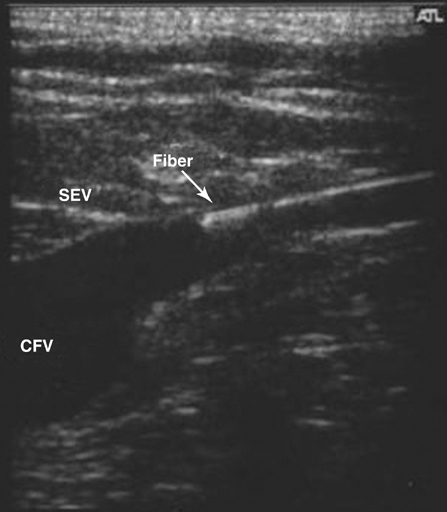
Endovenous radiofrequency (RF) ablation is an effective therapy of varicose veins affecting the greater saphenous vein (GSV), the small saphenous vein (SSV), the anterior accessory greater saphenous vein (AAGSV), the posterior accessory greater saphenous vein (PAGSV), and straight venous segments. The most current therapy is RF-controlled segmental thermal ablation (ClosureFast, Covidien, Mansfield, MA). This catheter fits through a 7-Fr introducer sheath (Figure 1). Venous treatment is segmental, rather than using a continuous catheter pullback rate, resulting in a more standardized delivery of energy. The older RF catheter (Figure 2) used a continuous pullback. The more variables one can eliminate with any technique, the better for physician and patient. A temperature of 120°C is attained at the 7-cm heating segment at the catheter tip. This equates to approximately 70 joules per centimeter of vein treated, which is in the same range delivered with laser ablation. The generator (Figure 3) monitors and delivers this energy automatically by modulating electrical power and impedance. As with all thermal endovenous ablation techniques, the RF catheter is positioned 2 cm from the saphenofemoral junction (SFJ) (Figure 4) or at the fascial curve near the saphenopopliteal junction (SPJ) (Figure 5). In the great majority of cases (>95%) the catheter can be positioned without any adjunctive steps such as guidewire placement, second access site, or ultrasound assistance. In cases of saphenous tortuosity, an attempt can be made to straighten this segment by changing leg position or by using the ultrasound probe with gentle compression to straighten the segment. When doing this, a significant amount of pressure or manipulation should not be applied because it can lead to spasm. Once again, gentle, slow, deliberate movements are best.
Endovascular Radiofrequency Treatment of Varicose Veins
Procedure
Access
Positioning
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Endovascular Radiofrequency Treatment of Varicose Veins