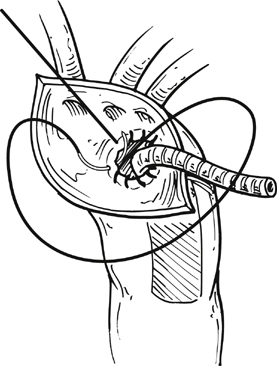
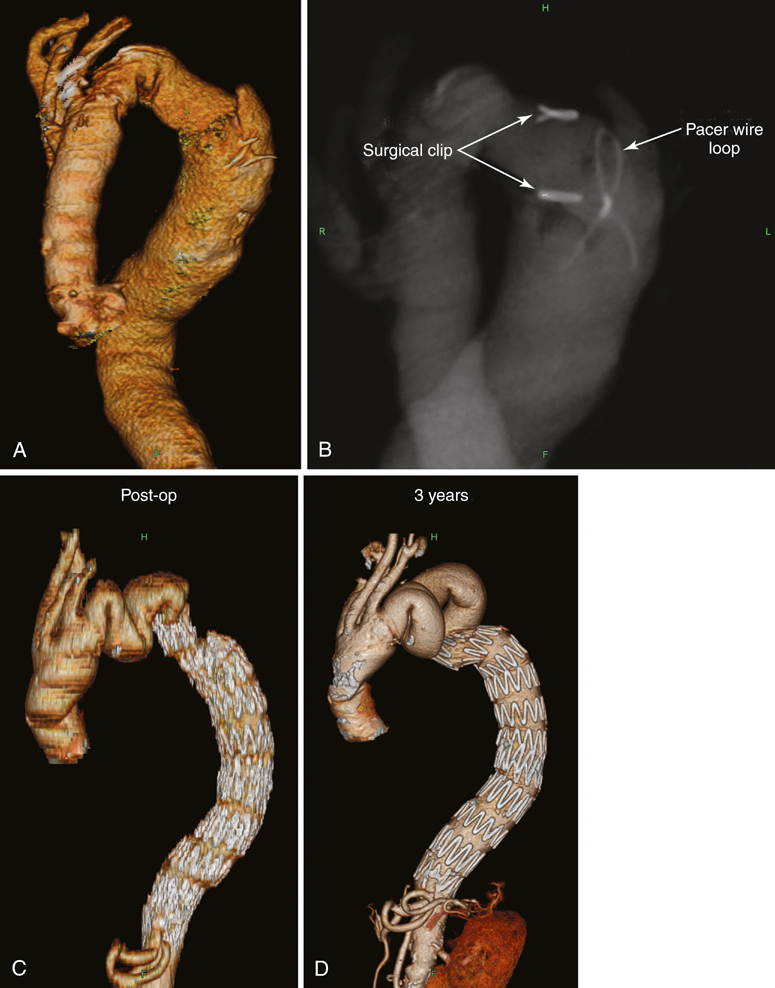
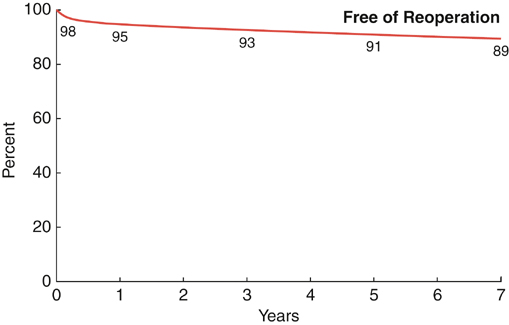
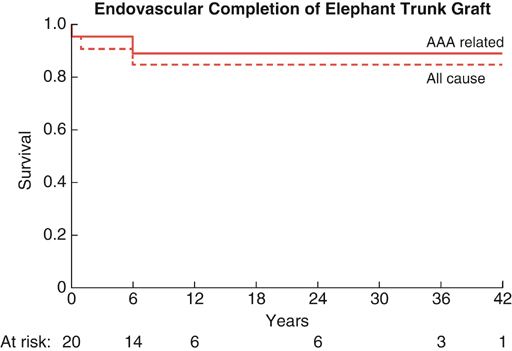
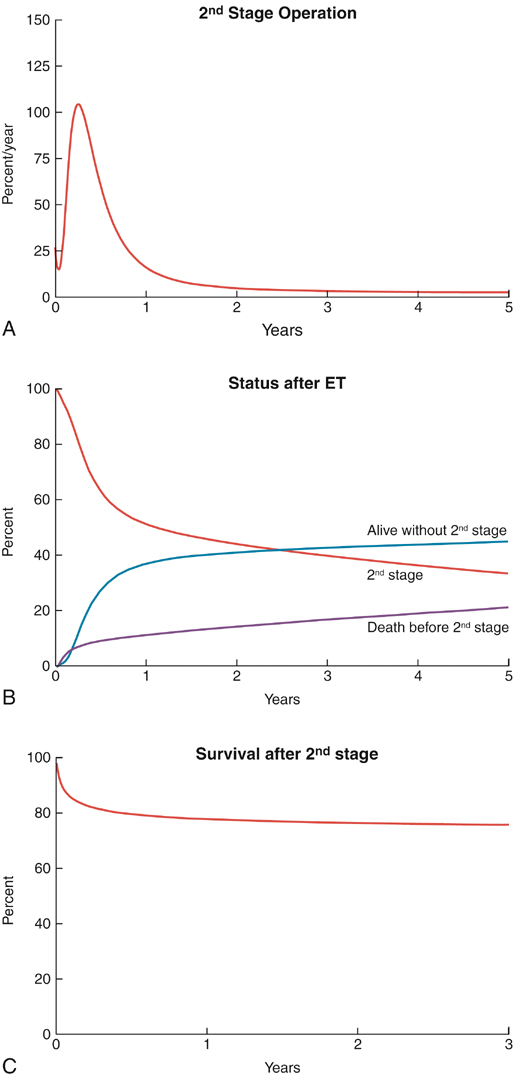
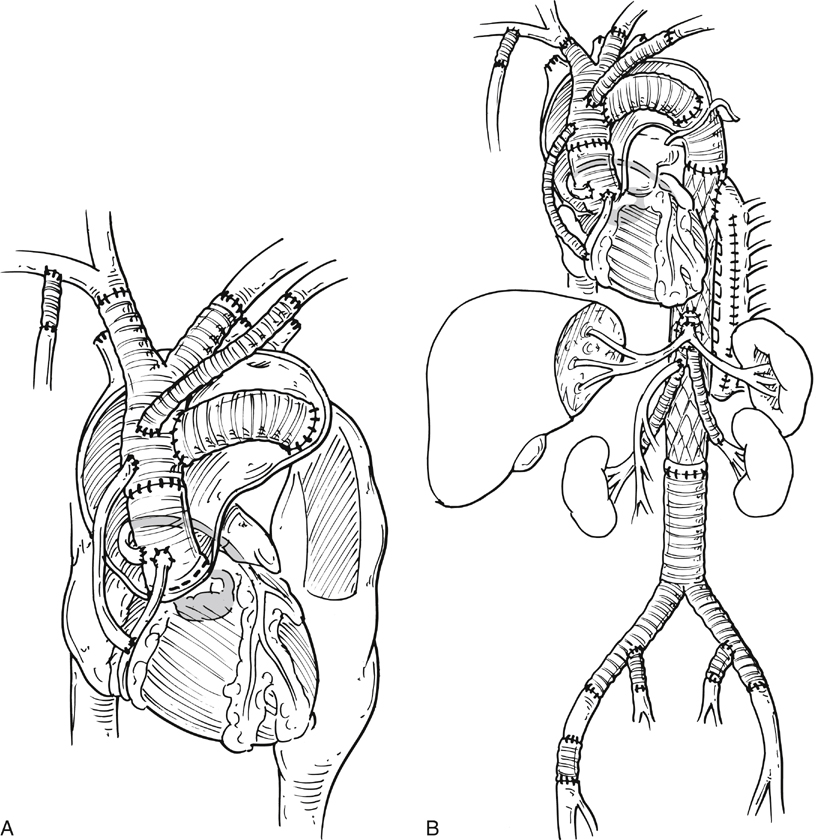
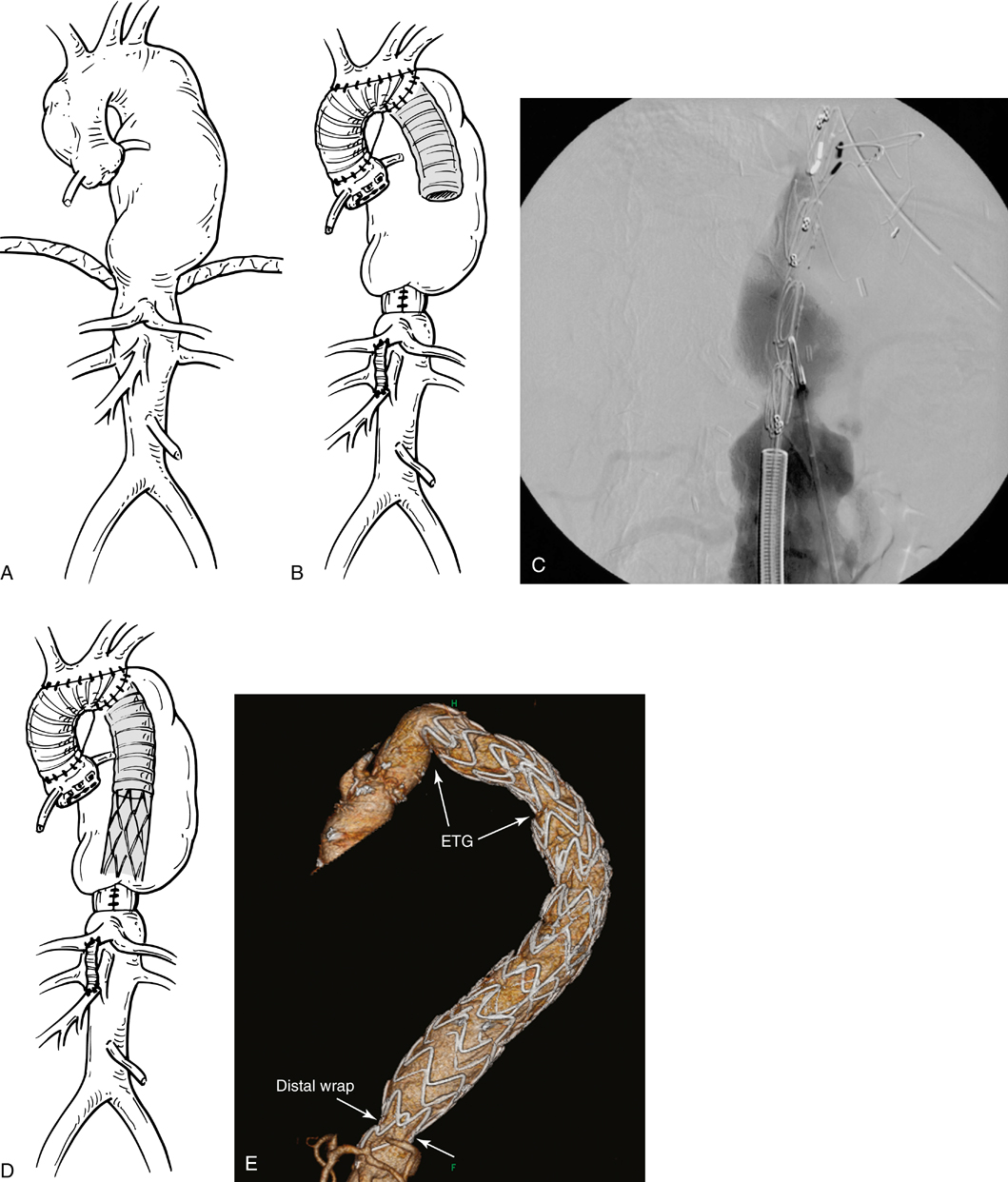
Because of this rupture risk, the technique was modified so that the tube graft was inverted on itself and then placed in the descending aorta (Figure 1). The anastomosis was then performed in the distal arch to the folded over and invaginated graft. This allowed a quicker and safer anastomosis to be performed and also resulted in a marked decline in the perioperative risk of distal arch rupture. Further modifications have included resewing the distal anastomosis with pledgetted horizontal mattress sutures because occasionally a periprosthetic leak could occur there; no longer sewing a side graft to the aortic arch because the right subclavian artery was used for arterial blood flow from the pump thus reducing the risk of stroke; and placing a pacing wire and clips on the end of the elephant trunk to facilitate finding an opening of the elephant trunk for endovascular grafting as well as allowing a wire to be passed through the looped pacing wire in case the elephant trunk needed to be stretched to remove any kinks and to reduce any risk of accordioning of the elephant trunk (Figure 2). Deep hypothermia and circulatory arrest is used for the initial procedure; the circulatory-arrest period should be kept to less than 30 minutes to reduce the risk of stroke after the procedure. Indeed, in one of our previous reports the 30-day survival rate was 98% and the stroke rate was 4% after the first-stage procedure. It is important to complete the second procedure as soon as possible to reduce the ongoing risk of rupture (Figure 3). After completing the second-stage procedure the late survival rate was 80% (Figure 4). A subsequent study by us also showed that completing the second stage with an endovascular device also resulted in a similar survival rate (Figure 5). It is important to not make the distal graft too small or too short (Figure 6). Most patients whose visceral arteries need to be reconstructed require individual bypasses with a short infrarenal elephant trunk. It is best to do individual bypasses to the visceral vessels with branch grafts and leave a separate infrarenal tube graft for later aorta and iliac artery stenting (Figure 7). In some patients there may be potential problems doing thoracoabdominal aneurysm stenting, particularly because the wait time is approximately 3 months to get a custom-made device. In such cases we have done a superceliac aortic wrap to reduce the aorta to a size suitable for stent grafting (Figure 8). This allows the second-stage endovascular stenting procedure to be done earlier into the wrap. Another alternative is to enter the posterior pericardial sac and open the aorta and resect the aortic dissection septum, which then facilitates placing a stent graft from the elephant trunk to the septum resected site, with distal perfusion of both the true and the false lumens. For most patients undergoing second-stage elephant trunk procedures who have a chronic dissection, particularly because these patients are typically young and have connective tissue disorders, we do an open second-stage procedure. However, some data suggest that the long-term survival may be as good with endovascular procedures for chronic dissection, and this requires further study. There are several options for performing the second-stage endovascular elephant trunk procedure:
Endovascular Graft Completion of Elephant Trunk Thoracic Aneurysm Repair
Second-Stage Endovascular Procedure
 Only the descending aorta is stented, which is typically the case in patients with degenerative aneurysms ending above the celiac artery with a distal landing site of less than 3.5 cm and without clot within the aortic lumen.
Only the descending aorta is stented, which is typically the case in patients with degenerative aneurysms ending above the celiac artery with a distal landing site of less than 3.5 cm and without clot within the aortic lumen.
 A stent graft is placed from the elephant trunk to the celiac artery.
A stent graft is placed from the elephant trunk to the celiac artery.
 Typically for type I thoracoabdominal aneurysms, most of a second-stage elephant trunk stent is placed down to below the celiac artery, with separate either covered or noncovered side stents into the visceral vessels through openings in the aortic stent.
Typically for type I thoracoabdominal aneurysms, most of a second-stage elephant trunk stent is placed down to below the celiac artery, with separate either covered or noncovered side stents into the visceral vessels through openings in the aortic stent.
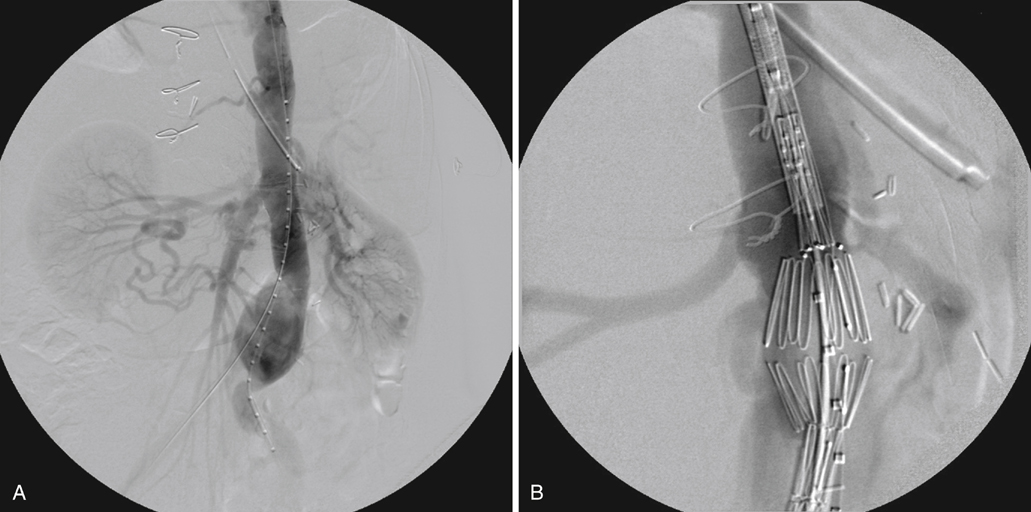
 A premanufactured stent graft with spiral endovascular branched tube grafts is placed into the visceral vessels, completing the repair (Figure 9).
A premanufactured stent graft with spiral endovascular branched tube grafts is placed into the visceral vessels, completing the repair (Figure 9).
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Endovascular Graft Completion of Elephant Trunk Thoracic Aneurysm Repair