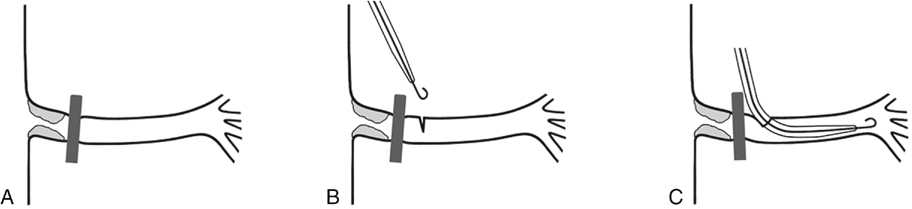
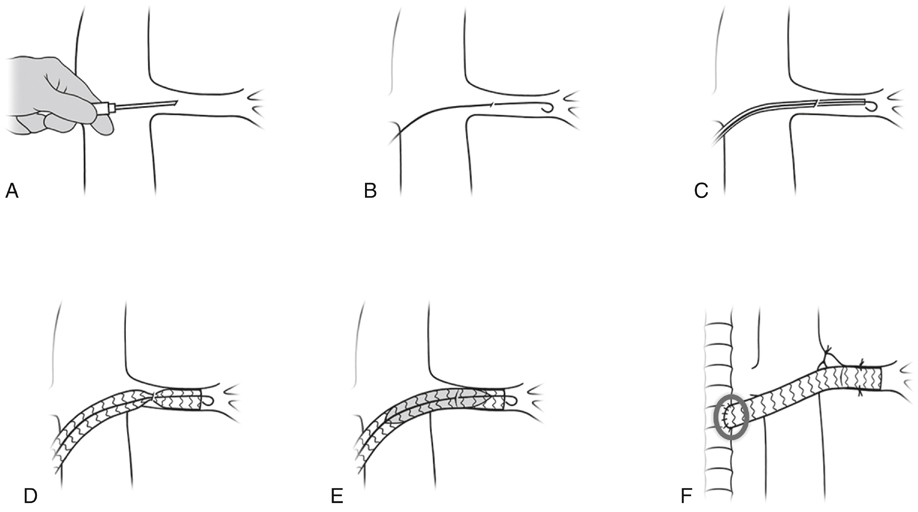
Konstantinos P. Donas, Felice Pecoraro, Thomas Pfammatter, Zoran Rancic, Dieter Mayer, Frank J Veith, Giovanni Torsello and Mario Lachat This section briefly describes the procedure for the right renal artery. Although this technique leads to considerable reduction in the technical difficulties with challenging vascular anastomoses, a sutured Viabahn-to-bypass graft anastomosis is still necessary (Figures 1 and 2). Moreover, suturing the Viabahn, a stent graft with a very thin wall, to a vascular graft proved sometimes to be difficult or resulted in bleeding from the suture lines. Introduction of the stent graft directly through the feeding bypass graft into the renal artery and deploying it as a connector from inside the bypass graft provides a solution to this problem (Figure 3). This technique allows the graft-to-vessel connection to be made in a few seconds. Furthermore, when the proximal end of the bypass graft is already attached to the vascular tree, interruption of blood flow can be kept to less than 1 minute. More recent technical improvements have allowed modifications of this procedure to be applied to almost all vessels, even if they are of small diameter and/or calcified. The target vessel is interrupted proximally with a clip or ligature and incised just enough to be sure the guidewire and Viabahn are located endoluminally (Figure 4). As an alternative, the vessel can be completely transected, allowing the introduction (approximately 1–2 cm) and deployment of the Viabahn under direct vision control (Figure 5). For deployment, a forceps has to hold the artery to prevent its retraction. Incision techniques are particularly useful to ensure correct introduction of the stent graft in vessels with a diameter of less than 4.5 mm and/or when vessel puncture or guidewire introduction appears suboptimal. The transection technique is useful in calcified arteries or dissected vessels that cannot be punctured or where an incision technique would be hazardous. In diffusely or circumferentially calcified arteries, we used eversion endarterectomy to avoid plaque rupture and consequent dissection or embolization and/or to increase the luminal diameter.
Endograft (VORTEC) Reconstruction of Aortic Branches Allowing Endovascular Treatment of Aortic Aneurysms
Original Technique

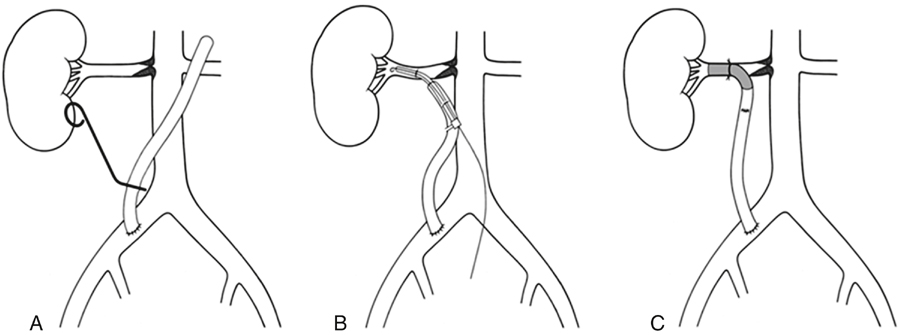
Incision and Transection Techniques
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine