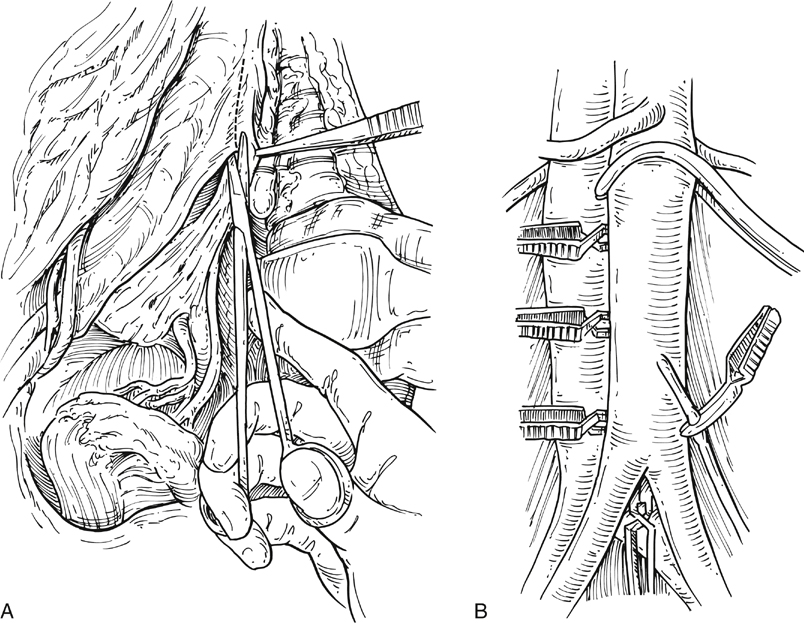
Operative exposure is obtained thorough a standard xiphoid-to-pubis midline abdominal incision. The incision in the retroperitonum over the aorta is placed toward the right of the midline and continued down along the right common iliac artery. The dissection is undertaken to preserve the periaortic nervi erigentes, which course along the left side of the aorta and left common iliac artery (Figure 1A). Aortoiliac endarterectomy requires complete mobilization of the aorta and iliac artery branches, including all of the lumbar arteries (see Figure 1B). This mobilization must be accomplished relatively atraumatically to minimize the risk of atheroembolization during the procedure.
Endarterectomy for Atherosclerotic Aortoiliac Occlusive Disease
Operative Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
