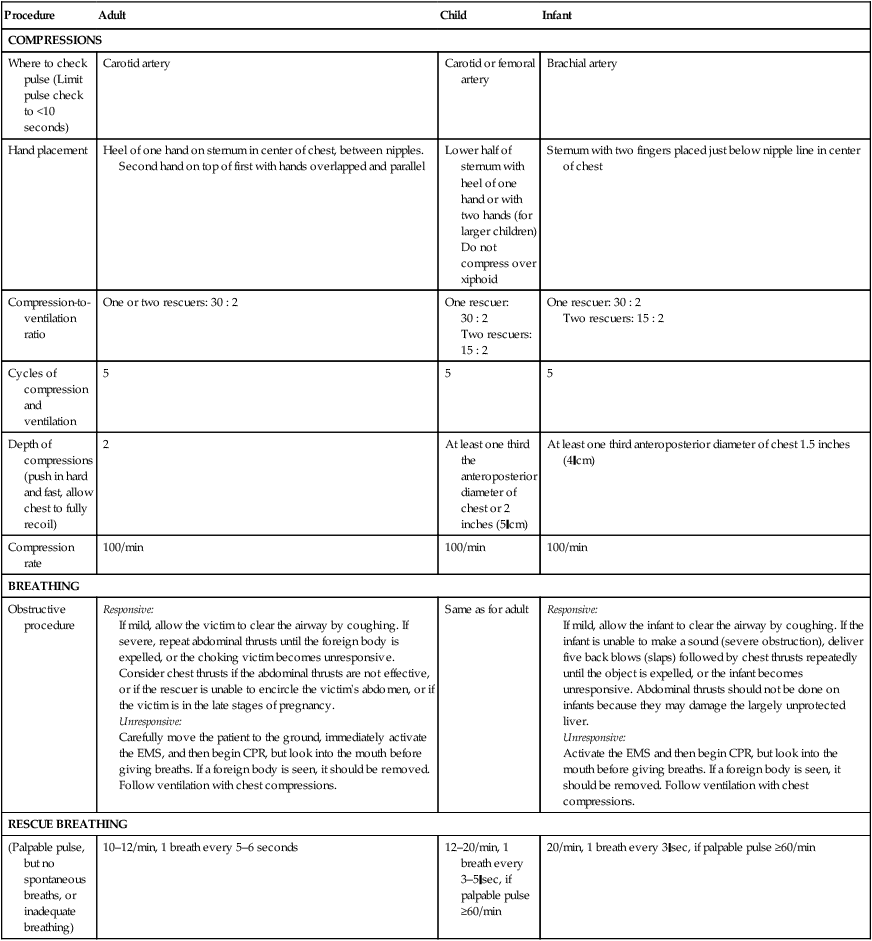
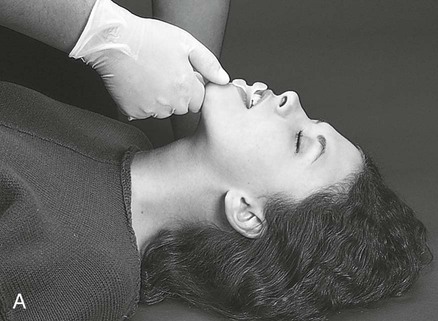
1. Manage effectively all aspects of a code. 2. Perform cardiopulmonary resuscitation (CPR) on adults, children, and infants. 3. Provide manual ventilation with a bag-mask device. 4. Describe the steps to use an automated external defibrillator (AED). 5. Describe ways of restoring ventilation. 6. Perform placement of a nasopharyngeal airway. 7. Identify complications that may result from CPR. Respiratory therapists (RTs) are involved in many aspects of patient care that may entail the need for emergency life support. Whether in an intensive care unit (ICU) or an emergency department (ED) or flying as a part of a medical transports team, RTs find themselves as key players in a patient’s care during a medical emergency. With RTs involved in airway management, especially in the emergent setting, being at the head of the bed often lends itself to managing the code. In the hospital setting, help is usually readily available. However, the RT must be familiar with the skills and practices of both one- and two-rescuer CPR for adults, children, and infants. Table 12-1 lays out the steps involved in CPR. The following is the step-by-step process for code management. TABLE 12-1 Steps for Cardiopulmonary Resuscitation in the Adult, Child, and Infant From Kacmarek RM, Stoller JK, Heuer AJ: Egan’s fundamentals of respiratory care, ed 10, St. Louis, MO, 2013, Mosby. a. Inspect for any neck or facial trauma. b. Perform either the head-tilt or the chin-lift method or the jaw thrust maneuver to open the airway. c. Perform oropharyngeal suctioning, if needed (see PA 11-1). 6. Remove the supplies from the patient’s room, and clean the area, as needed. 7. Remove PPE and perform proper hand hygiene prior to leaving the patient’s room. Management of a patient’s airway is typically the responsibility of the RT. Manual ventilation with a bag-mask device is necessary during airway emergencies, CPR, as well as transport of the mechanically ventilated patient (Figure 12-1). A bag-mask device is used most effectively when the RT is standing at the head of the bed. The components of a bag-mask device are provided in Figure 12-2
Emergency Life Support
Equipment
 AED with mannequin for defibrillation (optional)
AED with mannequin for defibrillation (optional)
 CPR mannequins for neonates, infants, and adults
CPR mannequins for neonates, infants, and adults
 Nasopharyngeal airways (various sizes)
Nasopharyngeal airways (various sizes)
» Skill Check Lists
12-1 Code Management
Procedure
Adult
Child
Infant
COMPRESSIONS
Where to check pulse (Limit pulse check to <10 seconds)
Carotid artery
Carotid or femoral artery
Brachial artery
Hand placement
Heel of one hand on sternum in center of chest, between nipples.
Second hand on top of first with hands overlapped and parallel
Lower half of sternum with heel of one hand or with two hands (for larger children)
Do not compress over xiphoid
Sternum with two fingers placed just below nipple line in center of chest
Compression-to-ventilation ratio
One or two rescuers: 30 : 2
One rescuer: 30 : 2
Two rescuers: 15 : 2
One rescuer: 30 : 2
Two rescuers: 15 : 2
Cycles of compression and ventilation
5
5
5
Depth of compressions (push in hard and fast, allow chest to fully recoil)
2
At least one third the anteroposterior diameter of chest or 2 inches (5 cm)
At least one third anteroposterior diameter of chest 1.5 inches (4 cm)
Compression rate
100/min
100/min
100/min
BREATHING
Obstructive procedure
Responsive:
If mild, allow the victim to clear the airway by coughing. If severe, repeat abdominal thrusts until the foreign body is expelled, or the choking victim becomes unresponsive. Consider chest thrusts if the abdominal thrusts are not effective, or if the rescuer is unable to encircle the victim’s abdomen, or if the victim is in the late stages of pregnancy.
Unresponsive:
Carefully move the patient to the ground, immediately activate the EMS, and then begin CPR, but look into the mouth before giving breaths. If a foreign body is seen, it should be removed. Follow ventilation with chest compressions.
Same as for adult
Responsive:
If mild, allow the infant to clear the airway by coughing. If the infant is unable to make a sound (severe obstruction), deliver five back blows (slaps) followed by chest thrusts repeatedly until the object is expelled, or the infant becomes unresponsive. Abdominal thrusts should not be done on infants because they may damage the largely unprotected liver.
Unresponsive:
Activate the EMS and then begin CPR, but look into the mouth before giving breaths. If a foreign body is seen, it should be removed. Follow ventilation with chest compressions.
RESCUE BREATHING
(Palpable pulse, but no spontaneous breaths, or inadequate breathing)
10–12/min, 1 breath every 5–6 seconds
12–20/min, 1 breath every 3–5 sec, if palpable pulse ≥60/min
20/min, 1 breath every 3 sec, if palpable pulse ≥60/min
Implementation
12-2 Manual Ventilation with a Bag-Mask Device


![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Emergency Life Support















