Emphysema of any pathogenesis (nearly always chronic obstructive pulmonary disease) verticalizes the frontal P-wave axis >60° in adults, which, as a single criterion, has screened for obstructive pulmonary disease. In patients with emphysema, the QRS was of a significantly shorter duration than that in matched control patients. We investigated whether combining these 2 criteria would better detect or screen for emphysema. From consecutive unselected daily electrocardiograms with sinus rhythm, 50 were selected with a P-wave axis of >60°. An equal control group from the same electrocardiogram continuum with a P-wave axis of ≤60° was matched for age and gender. The QRS durations were those measured by the electrocardiographic computer and manually verified individually. The charts were then reviewed for the diagnosis of chronic obstructive pulmonary disease and/or pulmonary emphysema according to the pulmonary function test and chest radiographic findings, respectively. The patients and controls were well matched demographically. Those with a vertical P axis had a strikingly greater incidence of emphysema than did the controls (86% vs 4%, respectively). The sensitivity of a P axis >60° was 96% and the specificity was 87%. The mean QRS duration with emphysema was significantly shorter (78 ± 8 vs 89 ± 6 ms, p <0.01). The combination of QRS duration <75 ms in conjunction with a P axis of >60° achieved a specificity of 100%, although the sensitivity decreased to 33%. We have reported multiple other cutpoints for each and for the combination. In conclusion, a P axis >60° can be used alone with very high sensitivity and specificity to detect emphysema. The verticality of the P axis is usually immediately visible in the limb leads; therefore, this could be a rapid screening test for emphysema. The specificity was increased when combined with a shortened QRS duration, at the cost of the sensitivity.
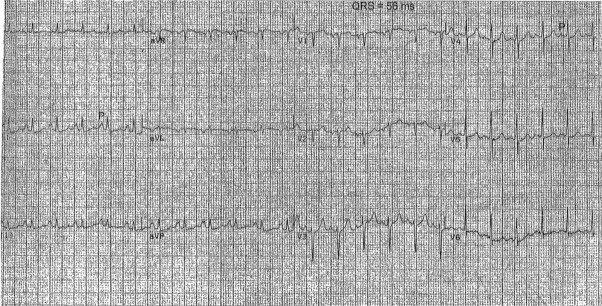
The electrocardiographic findings in adults >45 years old can sensitively and quasispecifically reflect the presence of pulmonary emphysema. Emphysema of any pathogenesis, although nearly always due to chronic obstructive pulmonary disease, has long been associated with verticalization of the frontal P axis. A vertical P axis (>60°) during sinus rhythm used as a single criterion can screen for obstructive pulmonary disease with 89% sensitivity and 96% specificity. Vertical P axes during sinus rhythm can be obvious on an electrocardiogram. Simply, an entirely inverted or dominantly negative P wave in lead aVL or P III definitely larger than P I will result in an axis >60°, making either virtually an instantaneous screening test ( Figure 1 ). Moreover, QRS complexes in patients with emphysema will be of a significantly shorter duration than QRS complexes in patients without emphysema. We investigated whether combining the P-axis and QRS duration data would provide even better criteria to detect emphysema.
Methods
From unselected, consecutive, routine, inpatient electrocardiograms, 50 with sinus rhythm and a P axis >60° were selected. An equal number of electrocardiograms with a P-wave axis of ≤60° from the same continuum were individually matched for age and gender as the control group ( Table 1 ). Patients <45 years old were excluded, because vertical P axes are the rule in healthy children and many young adults. Other exclusion criteria were rhythm other than sinus and intraventricular conduction delays (QRS duration >100 ms). The P axes were determined in the customary manner. The QRS durations were measured by the computer and manually verified individually. The charts were then reviewed for the diagnosis of chronic obstructive pulmonary disease and/or pulmonary emphysema according to the pulmonary function test findings (specifically, a reduced forced expiratory volume in 1 second) and chest radiographic findings showing emphysematous hyperlucency. Statistical analysis was done using the Statistical Package for Social Sciences, version 13.0. The Student t test was used to compare continuous variables. The Pearson chi-square test was used for categorical variables. p Values ≤0.05 were considered statistically significant.
| Variable | P Axis | p Value | |
|---|---|---|---|
| >60° (n = 50) | ≤60° (n = 50) | ||
| Age (years) | 65 ± 12 | 64 ± 13 | 0.75 |
| Gender | 0.83 | ||
| Female | 32 (64%) | 32 (64%) | |
| Male | 18 (36%) | 18 (32%) | |
| QRS (ms) | 79 ± 8 | 89 ± 6 | <0.001 |
| Emphysema | 86% | 4% | <0.001 |
Results
The entire group of 100 patients had a mean age of 65 years, 64% were women, the mean P axis was 58°, the QRS duration was 84 ms, and 55 had emphysema. Patients with vertical P axes had a strikingly greater incidence of emphysema than did the control group (86% vs 4%; Table 1 ). The sensitivity of a P axis >60° for emphysema was 96%, and the specificity was 87% ( Table 2 ). The mean QRS duration in patients with emphysema was significantly shorter (78 ± 8 vs 89 ± 6 ms; Table 3 ). A QRS duration <90 ms had a sensitivity of 100% in the present series. When using a QRS duration of <75 ms (a previous reported cutpoint ) in conjunction with a P-wave axis >60°, the specificity of the combination for emphysema approached 100%, although the sensitivity for the combined criteria decreased to only 33% ( Table 4 ).



