A woman with systemic lupus erythematosus and a regular supraventricular tachycardia continues to have electrocardiographic abnormalities after the spontaneous return of normal sinus rhythm.
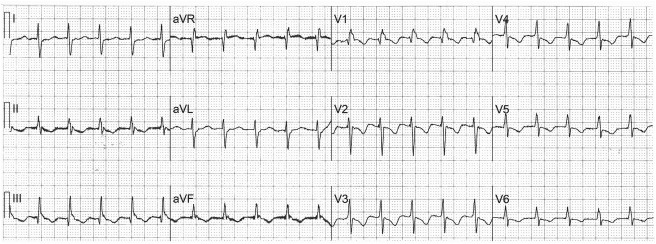
A 35-year-old woman with a 13-year history of systemic lupus erythematosus is admitted to the hospital with the sudden onset of palpitations and dyspnea, after several weeks of bilateral leg edema, and an electrocardiogram is recorded ( Figure 1 ). The palpitations and dyspnea spontaneously disappear before a second electrocardiogram ( Figure 2 ). The QRS during the tachycardia is wider than the QRS during sinus rhythm because of deformation of the terminal portion of the QRS during the tachycardia by a superimposed P wave, best seen in leads V 1 , II, III, and aVF, and the rhythm is probably the common form of atrioventricular nodal reentrant tachycardia.
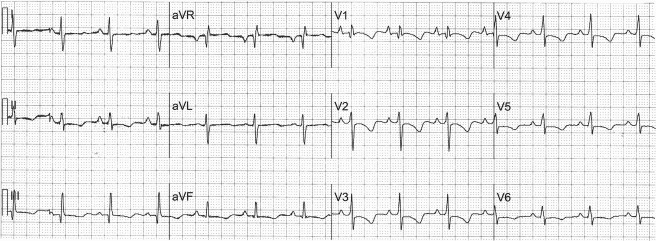
When the patient is in normal sinus rhythm ( Figure 2 ), there is evidence of right atrial enlargement (P waves in leads V 1 and V 2 are taller than 1.5 mm, when 1 mm = 0.1 mV) and right ventricular hypertrophy (a rightward QRS axis of +111° in the frontal plane; an R/S ratio >1.0 in lead V 1 with a negative T wave; and a ventricular activation time in lead V 1 >35 ms but <55 ms). The right ventricular hypertrophy is confirmed by an echocardiogram showing marked right ventricular enlargement with severe systolic dysfunction and flattening of the ventricular septum in systole and diastole suggesting both pressure and volume overload. The Doppler examination reveals pulmonary arterial systolic hypertension (∼70 mm Hg) to be the cause of the right ventricular enlargement. The inferior vena cava is dilated with poor inspiratory collapse suggesting a right atrial mean pressure of ∼20 mm Hg. Left-sided cardiac chambers are of normal size, and the left ventricular ejection fraction is >55%.
Systemic lupus erythematosus and scleroderma (systemic sclerosis) are the 2 connective tissue diseases most often associated with pulmonary arterial hypertension, but other causes, especially pulmonary emboli, must be excluded. This patient had deep vein thrombosis both before and during pregnancy many years earlier emphasizing the need for current exclusion of pulmonary emboli. On this admission, a computed tomographic angiogram using a pulmonary embolus protocol demonstrates a large main pulmonary artery, right ventricle, and right atrium; a small anterior pericardial effusion; and splenomegaly, but no evidence of pulmonary emboli. A venous ultrasound and Doppler study of the legs is normal.
The patient describes a similar episode of palpitations and dyspnea a month earlier in another city where she was given intravenous medication in the emergency department to stop the fast heart beat and then was admitted to the hospital, where pulmonary hypertension was diagnosed for the first time. Although James et al have histologically documented involvement of the cardiac conduction system in patients with systemic lupus erythematosus, this woman’s arrhythmia is probably unrelated to her lupus. Hypokalemia (2.3 mEq/L) caused by furosemide 40 mg bid and prednisone may have precipitated atrial premature complexes that resulted in atrioventricular nodal reentrant tachycardia.
Disclosures
The authors have no conflicts of interest to disclose.
See page 698 for disclosure information.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


