16 Elective Intervention for Stable Angina or Silent Ischemia
 Introduction
Introduction
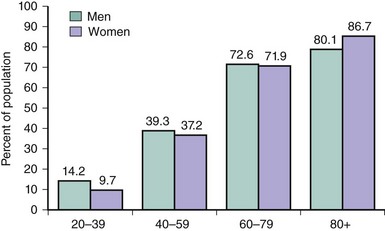
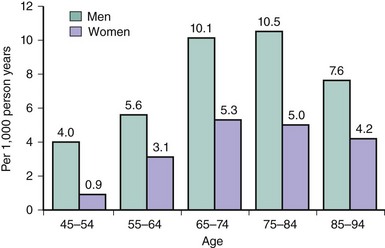
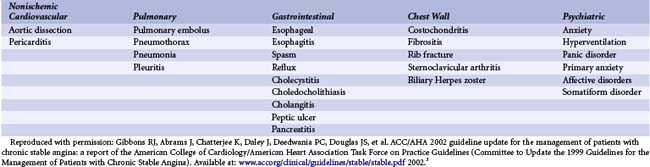
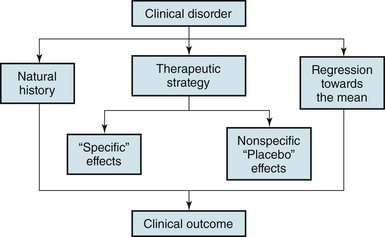
Angina pectoris affects approximately 9 million of the 16.3 million people with a diagnosis of coronary artery disease in the United States, and the prevalence increases with age for both established and symptomatic coronary disease (Figs. 16-1 and 16-2).1 In combating this disease, U.S. physicians performed an estimated 6.8 million inpatient cardiovascular procedures in 2007, an increase of 27% over the previous decade, including approximately 622,000 percutaneous coronary revascularization procedures. The mean hospital charge for percutaneous coronary intervention (PCI) was $56,015 in 2008,1 with average costs near $20,000 for a typical procedure and overnight hospitalization. While costly, appropriate revascularization in patients with chronic angina renders important prognostic benefits, contributing an estimated 5% to the total observed reduction in coronary heart disease mortality between 1980 and 2002.2 Despite this measurable success in addressing established disease, the incidence and costs associated with symptomatic coronary artery disease continue to grow throughout the world, contributing an ever-increasing proportion to the overall morbidity, mortality, and lost economic productivity in both developed and developing regions. Revascularization is intuitively central to the treatment paradigm for coronary artery disease. A mismatch between myocardial oxygen supply and demand is the predominant mechanism implicated in the development of symptoms associated with obstructive coronary artery disease. Generally, epicardial coronary lesions comprising at least 50% to 79% diameter obstruction (70%-90% by cross-sectional area measurement) are associated with impaired flow and resultant ischemia. When correlated with clinical or objective evidence of ischemia, such lesions are attractive targets for symptom management. However, the realm of patients with symptoms or signs of ischemia may also include those with abnormal coronary endothelial function, coronary vasospasm, microvascular dysfunction, and even silent, asymptomatic myocardial ischemia. In addition, symptoms reminiscent of ischemic angina may be a manifestation of a noncardiovascular process, such as gastrointestinal, musculoskeletal, or neuropsychiatric pathology (generally anything from the navel to the nose), while other patients, especially women and the elderly, may present with symptoms such as fatigue, chronic “soreness,” or dyspnea, which may not be immediately recognized as an expression of cardiovascular disease (Tables 16-1 and 16-2).3 Individuals with significant ischemia may also remain seemingly unaffected by symptoms because of the “self-regulation” of activity, essentially avoiding activities that have previously caused discomfort. Careful attention to individual patient presentation and characteristics, then, is essential for proper diagnostic triage and management. Once recognized, the goals and methods of treatment for this heterogenous syndrome include reduction in both morbidity and mortality, although anticipated benefits depend on patient characteristics and the treatment modality employed. Percutaneous revascularization has, as its principal benefit, the relief of angina. Symptom relief is the direct effect of a reduction in ischemic burden—although, especially in the setting of residual disease or incomplete abrogation of ischemia, additional complex factors no doubt play a role (Fig. 16-3).4 While improved survival and reduction of major cardiovascular events are important therapeutic objectives, there are limited data to support a major role for percutaneous revascularization in reducing adverse events in the broader population of patients with stable ischemic coronary disease (Fig. 16-4).5 In fact, a clear survival advantage for revascularization over medical therapy alone has generally been limited to patients at high clinical or anatomical risk, specifically those high-risk patients undergoing surgical revascularization for severe symptomatic triple-vessel disease, left main coronary disease, left ventricular dysfunction, and manifestations of severe ischemia.6 Numerous advances in the care of patients with established coronary disease have occurred in the interim, however, with the development of advanced medical therapies and surgical and percutaneous revascularization techniques. In the setting of appropriate and optimal medical therapy (OMT), percutaneous revascularization remains an important adjunct for symptom relief and reduction of ischemic burden.
TABLE 16-2 Ischemic Provocation or Exacerbating Factors
| Increased Oxygen Demand | Decreased Oxygen Supply |
|---|---|
| Noncardiac conditions | |
| Cardiac conditions | |
Reproduced with permission: Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for the Management of Patients with Chronic Stable Angina). Available at: www.accorg/clinical/guidelines/stable/stable.pdf 2002.3
 Revascularization in Patients with Chronic Stable Angina
Revascularization in Patients with Chronic Stable Angina
The principles and practice of modern coronary revascularization strategies are rooted in the conduct and results of studies performed in the 1970s and 1980s. These historic investigations set the framework for our current understanding of the role of both surgical and percutaneous coronary revascularization in the treatment armamentarium of chronic symptomatic ischemic coronary artery disease. While these studies provided important insight into the outcome of revascularization and medical therapy using the methodology of the time, great strides have subsequently been made in all areas of treatment, thus decreasing the applicability of these trials to guide therapy in the prevailing healthcare environment. Today, O has been clearly established as the cornerstone of treatment for coronary artery disease. The impact of medical therapy has grown with the introduction of advanced antiplatelet therapy, statins, and angiotensin converting enzyme and receptor inhibition, among other established and evolving therapies that provide important moderation of the inexorable progression of coronary disease. Indeed, appropriate application of evidence-based therapy has had important societal health implications, with a resultant measurable reduction in adverse cardiac events over the past several decades. While appropriate revascularization in patients with chronic angina contributed an estimated 5% to this observed reduction in coronary heart disease mortality between 1980 and 2002, a much larger 50% of the total reduction is attributed to improvement in the risk-factor profiles of those populations in jeopardy, largely thanks to improved agents and the greater application of this medical therapy.2 While PCI is an important adjunct for symptom control and of established value in reducing both subsequent morbidity and mortality after acute coronary syndromes, both PCI and surgical revascularization are palliative procedures, with lesion progression accounting for significant recurrent morbidity. Recent studies demonstrate the impact of lesion progression and the need for aggressive concomitant medical therapy in the setting of PCI. Mahn-Won and colleagues7 retrospectively studied 507 patients undergoing PCI and found that 16% of them underwent clinically driven repeat PCI to treat preexisting nonculprit coronary lesions during the 3-year study period. During the first year after initial PCI, 7.7% of patients in this cohort underwent non-culprit-lesion PCI, with the rate increasing to 16% at 3 years. Greater extent of disease, as manifest by a larger baseline number of significant coronary lesions, independently predicted repeat PCI (odds ratio [OR] 2.29, 95% confidence interval [CI] 1.5–3.5, P < 0.001), as did the baseline risk factors of low levels of high-density lipoprotein (<40 mg/dL; OR 2.01, 95% CI 1.01–3.98, P = 0.046), hypercholesterolemia (total cholesterol >200 mg/dL; OR 1.46, 95% CI 1.22–1.97, P = 0.04), history of PCI (OR 1.24, 95% CI 1.09–1.60, P = 0.003), and increased triglyceride levels (OR 1.003, 95% CI 1.001–1.007, P = 0.038). An additional natural history study8 of patients who underwent intravascular ultrasound evaluation after PCI for an acute coronary syndrome found that fully one-half of major subsequent adverse events at 3 years occurred at nonculprit sites. Adequate medical therapy and risk modification, then, are essential in the peri- and postinterventional setting to reduce subsequent mortality and morbidity, including symptom recurrence and need for repeat procedures associated with lesion progression and new lesion development.
 Addition of Revascularization to Optimal Medical Therapy
Addition of Revascularization to Optimal Medical Therapy
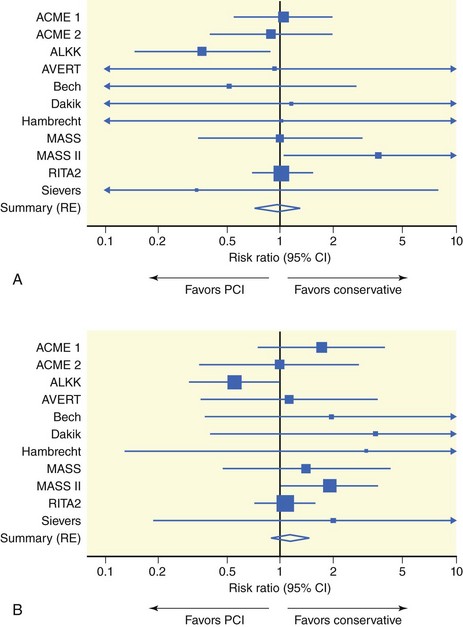
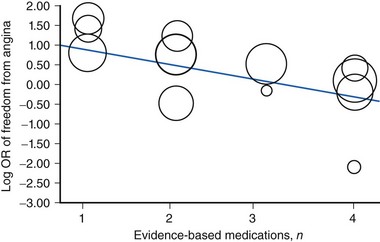
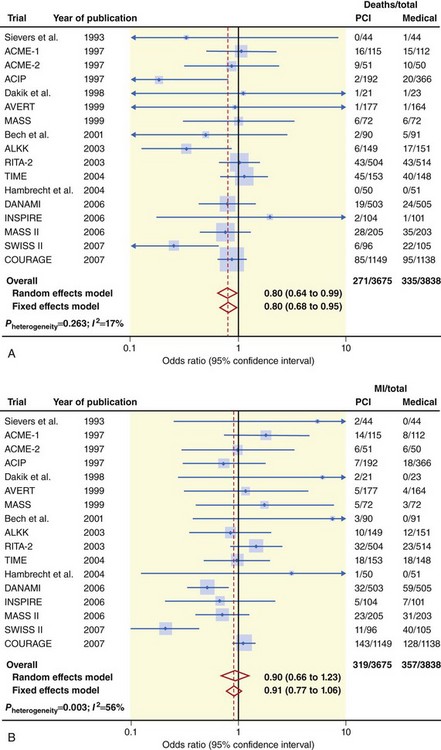
The selection of treatment strategies in patients with chronic stable angina depends on symptom status, anatomical complexity, clinical comorbidity, and risk. The main indications for revascularization are to improve symptoms that persist despite O as well as to improve prognosis. While generally suggesting a benefit for revascularization, most randomized trials comparing medical therapy to percutaneous revascularization are limited by their historical nature and entry bias. It is generally agreed that PCI affords rapid and effective symptom relief, a concept borne out in several trials as well as a recent metanalysis9 of 14 trials, which demonstrated a statistically significant benefit in angina relief with PCI compared with medical therapy (OR 1.69, 95% CI 1.24–2.30). Interestingly, there was important heterogeneity across the trials, with substantially less benefit noted in more contemporary trials of PCI versus OMT, such as COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation),10 published in 2007 (OR 1.10, 95% CI 0.81–1.49), and OAT (Occluded Artery Trial),11 published in 2006 (OR 0.83, 95% CI 0.47–1.47). Using meta-regression analysis of the treatment effects of PCI relative to medical therapy, Wijeysundera et al. were able to document an inverse relationship between freedom from angina and the number of “evidence-based” medications utilized during the conduct of a trial (Fig. 16-5).9 Subgroup analysis of the COURAGE trial12 confirmed a diminution of angina benefit over time for patients treated with PCI as an initial strategy. While there was a statistically significant difference in rates of freedom from angina between the OMT alone and OMT plus PCI groups at 3 months (42% vs. 53%, P < 0.001), this difference was no longer evident at 3 years (56% vs. 59%, P = 0.30). Although there are numerous potential reasons for this convergence of angina rates during follow-up, including crossover to revascularization from the medical arm, ascertainment bias due to small follow-up populations, and a host of other factors (Fig. 16-3),4 an important finding is that patients with the most significant anginal burden at baseline obtained the greatest benefit from PCI, whether in OMT alone or OMT-plus-PCI group. In aggregate, these data support a robust, reliable antianginal benefit for PCI in patients with persistent symptoms despite medical therapy. The benefit of percutaneous revascularization on the hard endpoints of death and myocardial infarction is more controversial and the complexities greater. The relatively low event rates among stable patients with coronary disease, particularly those healthy enough and eligible to be enrolled in randomized prospective trials, limits the discriminatory ability of individual clinical trials to identify treatment effects. Even large metanalytic studies, limited by significant heterogeneity of patient groups and inclusion of antiquated therapies (balloon angioplasty and limited medical options), have provided conflicting results. A metanalysis by Katritsis and colleagues5 incorporated data from 11 randomized trials of PCI compared with medical therapy in patients with documented coronary artery disease in the absence of a recent acute coronary syndrome. With 2,950 patients included in the analysis, no significant difference could be identified between PCI and medical therapy for overall death (Fig. 16-4A), cardiac death, and myocardial infarction (Figure 16-4B), nonfatal myocardial infarction, or subsequent revascularization. A more recent metanalysis by Schomig and colleagues13 of 17 trials involving 7,513 patients with chronic stable angina randomized over a 17-year period to PCI or OMT alone again found no significant benefit for PCI over medical therapy with regard to rates of nonfatal myocardial infarction (Fig. 16-6A). However, with selection of cardiac mortality rather than overall mortality as an endpoint, this analysis did suggest a potential advantage for a PCI-based therapeutic strategy for improving long-term outcome (Fig. 16-6B). Further analysis suggested that this benefit was most pronounced in patients who had suffered a recent (<4 weeks) myocardial infarction, as they had about a 35% reduction in the odds of death compared with an estimated risk reduction of 17% for patients with truly stable coronary disease. Both of these metanalyses, however, were limited by several factors, including significant heterogeneity of patient groups and treatments, inclusion of patients with recent acute coronary syndromes, and significant variability in treatments across studies and time periods. Another metanalysis14 comparing revascularization (surgical or percutaneous) with medical therapy over a 30-year period from 1977 to 2007 confirmed a significant reduction in all-cause mortality associated with revascularization (OR 0.74, 95% CI 0.63-0.88). When this study was stratified by revascularization type, the investigators were also able to show a reduction in mortality with both surgical (OR 0.62, 95% CI 0.50–0.77) and percutaneous (OR 0.82, 95% CI 0.68–0.99) revascularization approaches compared with OMT. This metanalysis, however, like the others, included trials encompassing a broad array of patient populations, including those with recent acute coronary syndromes; it was also limited by the historic nature of treatment algorithms spanning the 30-year study period. Trikalinos and colleagues,15 in a 20-year network analysis that took into account the evolution of interventional approaches over time, were unable to document a beneficial effect of PCI-based strategies on rates of death or myocardial infarction compared with contemporaneous medical therapy. As previously noted, a major hurdle in the assessment of survival benefits associated with revascularization trials is the relatively low overall event rate. While annualized mortality associated with chronic coronary arterial disease remains approximately 1% to 3% in contemporary series,14,16,17 the risk of adverse events increases with the degree of left ventricular dysfunction,18 ischemic burden,19 and functional limitation (Table 16-3).20 In addition, risk is increased in the presence of diabetes mellitus, chronic kidney disease, and greater severity of ischemic symptoms16 and anatomical complexity.21 It is not surprising, then that a gradient of benefit can be observed for revascularization compared with medical therapy, with greater benefit identified in those patients at greatest risk, whether due to anatomical complexity (Fig. 16-7)21 or severity of ischemic substrate (Fig. 16-8).22 Note that in the large cohort of patients identified in the Duke database (n = 18,481) who were treated with an initial strategy of revascularization (either surgical or percutaneous), significant benefit could be demonstrated across the spectrum of disease complexity compared with those patients treated initially with medical therapy alone.21
TABLE 16-3 Risk Stratification in Patients with Angina
| High-risk (>3% annual mortality rate) |
8. Echocardiographic wall motion abnormality (>2 segments) developing at low dose of dobutamine (less than or equal to 10 mg/kg per minute) or at a low heart rate (<120 beats per minute) |
| Intermediate-risk (1%–3% annual mortality rate) |