It is well established that myocardial infarction (MI) associated with coronary artery bypass grafting (CABG) predicts a poor outcome. Nevertheless, cardioprotective therapies to limit myocardial injury after CABG are lacking. Previous studies have shown that curcuminoids decrease proinflammatory cytokines during cardiopulmonary bypass surgery and decrease the occurrence of cardiomyocytic apoptosis after cardiac ischemia/reperfusion injury in animal models. We aimed to evaluate whether curcuminoids prevent MI after CABG compared to placebo. The 121 consecutive patients undergoing CABG were randomly allocated to receive placebo or curcuminoids 4 g/day beginning 3 days before the scheduled surgery and continued until 5 days after surgery. The primary end point was incidence of in-hospital MI. The secondary end point was the effect of curcuminoids on C-reactive protein, plasma malondialdehyde, and N-terminal pro–B-type natriuretic peptide levels. Baseline characteristics were comparable between the curcuminoid and placebo groups. Mean age was 61 ± 9 years. On-pump CABG procedures were performed in 51.2% of patients. Incidence of in-hospital MI was decreased from 30.0% in the placebo group to 13.1% in the curcuminoid group (adjusted hazard ratio 0.35, 0.13 to 0.95, p = 0.038). Postoperative C-reactive protein, malondialdehyde, and N-terminal pro–B-type natriuretic peptide levels were also lower in the curcuminoid than in the placebo group. In conclusion, we demonstrated that curcuminoids significantly decreased MI associated with CABG. The antioxidant and anti-inflammatory effects of curcuminoids may account for their cardioprotective effects shown in this study.
Curcuminoids, the polyphenols responsible for the yellow color of the curry spice turmeric, have been used to treat a variety of diseases in traditional Chinese and Indian medicine. The major curcuminoids present in turmeric are curcumin (curcumin I), demethoxycurcumin (curcumin II), and bisdemethoxycurcumin (curcumin III). Modern scientific research has confirmed the good therapeutic effects of the curcuminoid complex and its pharmacologic safety has been well established. A previous study has shown that curcuminoids suppress proinflammatory cytokines during cardiopulmonary bypass surgery and decrease the occurrence of cardiomyocytic apoptosis after cardiac ischemia/reperfusion injury in an animal model. Furthermore, a histopathologic study has demonstrated that curcuminoid treatment decreases the degree of myocardial necrosis in isoproterenol-administered rats. The well-known anti-inflammatory, antioxidant, and membrane-stabilizing effects of curcuminoids may help preserve cellular viability during cardiopulmonary bypass surgery. Therefore, curcuminoids may have a potential role in the limitation of myocardial ischemia/reperfusion injury after coronary artery bypass grafting (CABG). The present study evaluated whether curcuminoids prevent myocardial infarction (MI) after CABG compared to placebo.
Methods
The present study was a randomized, prospective, double-blinded, placebo-controlled trial performed at Maharaj Nakorn Chiang Mai Hospital, Chiang Mai University. We prospectively studied 121 consecutive patients undergoing CABG without valve surgery from September 2009 to December 2011. Informed consent was obtained from each patient to participate in the study. Patients were excluded if they had emergency cardiac surgery or any increase in creatine kinase-MB above the upper limit of the normal range at time of randomization. Because curcuminoids are mainly metabolized by the liver, patients with cholesteric jaundice (total bilirubin higher than twofold the upper normal limit) or severe liver disease (aspartate aminotransferase or alanine aminotransferase higher than threefold the upper normal limit) were not included in the study.
Curcuminoids and placebo used in the present study were provided in caplet form by the Research and Development Institute, the Government Pharmaceutical Organization, Bangkok, Thailand. One curcuminoid capsule contained curcuminoids 250 mg, which consisted of curcumin, demethoxycurcumin, and bisdemethoxycurcumin, in a ratio of 1.0:0.6:0.3, respectively, confirmed by high-performance liquid chromatography/mass spectrometry.
Enrolled patients were randomly allocated to receive placebo or curcuminoids 4 capsules 4 times/day (4 g/day) in addition to standard therapy beginning 3 days before the scheduled surgery and patients continued to receive the assigned treatment until 5 days after surgery. To assign patients to curcuminoids or placebo, a block randomization sequence was obtained by a statistical consultant who was not involved in the study. Assigned therapy was fully blinded; surgeons and investigators performing postoperative assessment were not aware of the randomization assignment.
All patients undergoing CABG were treated with standard therapy according to their physicians. Three surgeons performed CABG in the present study. The surgical techniques were determined at the discretion of the individual surgeons. On-pump CABG procedures were performed in 62 patients (51.2%), of whom 31 (25.6%) underwent on-pump CABG with the heart beating and 31 (25.6%) underwent on-pump CABG with conventional cardioplegic arrest. Myocardial protection was done with antegrade and retrograde cold blood cardioplegia. Off-pump CABG was performed in the remaining patients. The conduits used in patients in this study included the internal mammary arteries, radial arteries, and saphenous veins.
Twelve-lead electrocardiograms were recorded before surgery, 24, 48, and 72 hours after surgery, and 30-day follow-up visit. Serial creatine kinase-MB levels were assessed before surgery, at 8, 16, 24, 48, and 72 hours after intensive care unit arrival, and whenever an ischemic event was suspected. N-terminal pro–B-type natriuretic peptide (NT–pro-BNP) level was assessed before surgery and on the 5th postoperative day.
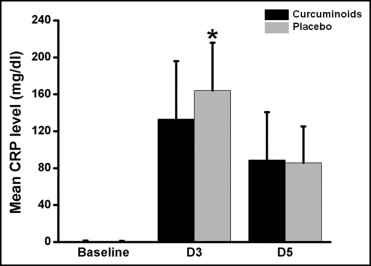
To examine the effects of curcuminoids on inflammatory response and oxidative stress after surgery, C-reactive protein (CRP) level was assessed before surgery and on postoperative days 3 and 5. In addition, plasma malondialdehyde (MDA) level, a marker for oxidative stress, was assessed before surgery and on postoperative day 5 using the high-performance liquid chromatographic method.
The primary end point of the study was to demonstrate that curcuminoids decrease the incidence of in-hospital MI compared to placebo. The secondary end point was to examine the effects of curcuminoids on CRP, MDA, and NT–pro-BNP levels after surgery.
The diagnosis of Q-wave MI was determined by the presence of new pathologic Q waves according to Minnesota Code criteria or new-onset left bundle branch block and creatine kinase-MB increase more than fivefold the upper normal limit of the investigators’ local laboratory within 24 hours of CABG. In the absence of the aforementioned electrocardiographic findings, creatine kinase-MB increase >10-fold the upper normal limit within 24 hours of CABG was considered indicative of non–Q-wave MI. If MI was suspected >24 hours after CABG, a creatine kinase-MB increase >2 times the upper normal limit with chest pain or an increase >3 times the upper normal limit was considered indicative of MI.
All analyses were done on an intention-to-treat basis. Demographic and perioperative variables were compared between groups with t test for normally distributed values; otherwise the Mann–Whitney U test was used. Proportions were compared by chi-square test or Fisher’s exact test when appropriate. Continuous variables are presented as mean ±SD or median ± interquartile range when appropriate. Categorical variables are displayed as percentages. Hazard ratios and 95% confidence intervals to assess the risk of the primary end point according to potential confounding variables were determined by logistic regression. Multivariate analyses were performed for variables with a p value <0.1 in univariate analysis using the logistic regression procedure. A p value <0.05 (2-tailed) was considered statistically significant.
Results
Demographic and perioperative variables are presented in Tables 1 and 2 , respectively. From September 2009 to December 2011, 121 consecutive patients who met the inclusion criteria were randomly divided to a curcuminoid group (n = 61) or a control group (n = 60). Baseline characteristics of patients in the 2 treatment groups were comparable including age, gender, co-morbidities, and previous percutaneous coronary revascularization ( Table 1 ). Perioperative features were not different between the curcuminoid and placebo groups ( Table 2 ).
| Characteristics | Curcuminoid | Placebo | p Value |
|---|---|---|---|
| (n = 61) | (n = 60) | ||
| Age (years) | 61.0 ± 9.1 | 61.1 ± 8.2 | 0.966 |
| Men | 34 (55.7%) | 35 (58.3%) | 0.917 |
| Body mass index (kg/m 2 ) | 24.1 ± 3.4 | 24.8 ± 4.8 | 0.290 |
| New York Heart Association class | 1.9 ± 0.5 | 2.0 ± 0.5 | 0.224 |
| Canadian Cardiovascular Society class | 1.9 ± 0.6 | 2.0 ± 0.5 | 0.194 |
| Serum creatinine (mg/dl) | 1.3 ± 0.4 | 1.4 ± 0.6 | 0.380 |
| Preoperative creatine kinase-MB (ng/ml) | 4.5 ± 4.1 | 5.5 ± 6.8 | 0.308 |
| Preoperative C-reactive protein (mg/dl) | 0.4 ± 0.5 | 0.5 ± 0.9 | 0.313 |
| Preoperative malondialdehyde (mmol/ml) | 7.4 ± 1.4 | 7.4 ± 1.1 | 0.908 |
| Preoperative N-terminal pro–B-type natriuretic peptide (pg/ml) ⁎ | 410.9 ± 577.2 | 533.4 ± 1,529.7 | 0.219 |
| Diabetes mellitus | 23 (37.7%) | 30 (50.0%) | 0.238 |
| Hypertension † | 55 (90.2%) | 54 (90.0%) | 1.000 |
| Dyslipidemia ‡ | 55 (90.2%) | 52 (86.7%) | 0.751 |
| Previous myocardial infarction | 17 (27.9%) | 15 (25.0%) | 0.879 |
| Current smoker | 8 (13.1%) | 4 (6.7%) | 0.378 |
| Heart failure | 5 (8.3%) | 6 (10.0%) | 1.000 |
| Previous coronary angioplasty | 4 (6.6%) | 1 (1.7%) | 0.371 |
| Left ventricular ejection fraction (%) | 54.8 ± 14.4 | 51.6 ± 15.1 | 0.483 |
| Preoperative medications | |||
| Aspirin or clopidogrel | 55 (90.2%) | 59 (98.3%) | 0.125 |
| β blocker | 48 (78.7%) | 48 (80.0%) | 0.891 |
| Statin | 56 (91.8%) | 56 (93.3%) | 1.000 |
| Angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker | 42 (68.9%) | 44 (73.3%) | 0.732 |
⁎ Median ± interquartile range.
† Blood pressure ≥140/90 mm Hg or currently treated with antihypertensive drugs.
‡ Low-density lipoprotein cholesterol >100 mg/dl, high-density lipoprotein cholesterol <40 mg/dl, or triglyceride >150 mg/dl.
| Characteristics | Curcuminoid | Placebo | p Value |
|---|---|---|---|
| (n = 61) | (n = 60) | ||
| Vessel involvement | |||
| Left main coronary artery stenosis | 12 (20.3%) | 17 (28.3%) | 0.422 |
| 3-Vessel disease | 45 (76.3%) | 49 (81.7%) | 0.619 |
| Off-pump coronary artery bypass grafting | 32 (52.5%) | 27 (45.0%) | 0.523 |
| On-pump coronary artery bypass grafting | 29 (47.5%) | 33 (55.0%) | |
| On-pump with beating heart | 14 (23.3%) | 17 (28.3%) | |
| On-pump with cardioplegic arrest | 15 (24.6%) | 16 (26.7%) | |
| Cardiopulmonary bypass duration (minutes) | 108.5 ± 48.1 | 106.6 ± 43.0 | 0.872 |
| Cross-clamp duration (minutes) | 80.0 ± 27.7 | 71.4 ± 26.3 | 0.379 |
| Temporary ventricular pacing | 24 (39.3%) | 19 (31.8%) | 0.231 |
| Number of bypass grafts | 3.5 ± 1.3 | 3.7 ± 1.0 | 0.374 |
| Myocardial infarction after coronary artery bypass grafting | 8 (13.1%) | 18 (30.0%) | 0.028 |
| Non–Q-wave myocardial infarction | 8 (13.1%) | 15 (25.0%) | |
| Q-wave myocardial infarction | 0 (0%) | 3 (5.0%) |
Incidence of the primary outcome (in-hospital MI) was decreased from 30.0% in the placebo group to 13.1% in the curcuminoid group (unadjusted hazard ratio 0.35, 0.14 to 0.89, p = 0.028). Most MI events were non–Q-wave MI ( Table 2 ). Apart from curcuminoid treatment, other predictors of in-hospital MI were identified. We found that on-pump CABG was significantly associated with a higher incidence of MI compared to off-pump surgery (35.5%, 22 of 62, vs 6.8%, 4 of 59, respectively, p <0.001). After multivariate analysis, we found that curcuminoid therapy remained the independent protective factor of in-hospital MI and that on-pump CABG was the independent predictive factor of in-hospital MI ( Table 3 ). Of 121 patients, 57 patients underwent echocardiography 1 month after surgery. Incidence of postoperative left ventricular dysfunction (left ventricular ejection fraction <40%) was significantly higher in the placebo group than in the curcuminoid group (25.9%, 7 of 27, vs 3.3%, 1 of 30, respectively, p = 0.021).
| Risk Factor | OR (95% CI) | p Value |
|---|---|---|
| Curcuminoid therapy | 0.35 (0.13–0.95) | 0.038 |
| On-pump coronary artery bypass grafting | 5.23 (1.92–14.28) | 0.001 |
Baseline preoperative CRP, MDA, and NT–pro-BNP levels were not different between the curcuminoid and placebo groups. However, mean increase in CRP level on postoperative day 3 compared to baseline level was significantly greater in the placebo group than in the curcuminoid group (difference +161.8 ± 54.1 vs +128.6 ± 60.5 mg/dl, respectively, p = 0.031; Figure 1 ). Plasma MDA level was increased after CABG in the placebo group but was decreased significantly after CABG in the curcuminoid group (difference +0.8 ± 1.4 vs −5.7 ± 1.5 mmol/ml, respectively, p <0.001; Figure 2 ). Furthermore, mean increase in postoperative NT–pro-BNP level compared to preoperative level was greater in the placebo group than in the curcuminoid group (difference +2,542.2 ± 2,631.2 vs +1,822.1 ± 2,102.9 pg/ml, respectively, p = 0.015).