Coronary angiography is the gold standard for defining obstructive coronary disease. However, radiation exposure remains an unwanted hazard. Patients referred for coronary angiography with abdominal circumference <45 inches and glomerular filtration rate >60 ml/min were randomized to the fluorography (n = 25) or cineangiography (n = 25) group. Patients in the fluorography group underwent coronary angiography using retrospectively stored fluorography with repeat injection under cineangiography only when needed for better resolution per operator’s discretion. Patients in the cineangiography group underwent coronary angiography using routine cineangiography. The primary end point was patient radiation exposure measured by radiochromic film. Secondary end points included the radiation output measurement of kerma-area product and air kerma at the interventional reference point (Ka,r) and operator radiation exposure measured by a dosimeter. Patient radiation exposure (158.2 mGy [76.5 to 210.2] vs 272.5 mGy [163.3 to 314.0], p = 0.001), kerma-area product (1,323 μGy·m 2 [826 to 1,765] vs 3,451 μGy·m 2 [2,464 to 4,818], p <0.001), and Ka,r (175 mGy [112 to 252] vs 558 mGy [313 to 621], p <0.001) were significantly lower in the fluorography compared with cineangiography group (42%, 62%, and 69% relative reduction, respectively). Operator radiation exposure trended in the same direction, although statistically nonsignificant (fluorography 2.35 μGy [1.24 to 6.30] vs cineangiography 5.03 μGy [2.48 to 7.80], p = 0.059). In conclusion, the use of fluorography in a select group of patients during coronary angiography, with repeat injection under cineangiography only when needed, was efficacious at reducing patient radiation exposure.
Currently, cineangiography is the standard method used to record images during fluoroscopic procedures and is a major contributor to total radiation dose administered during coronary angiography. However, current technology now allows improved visualization under fluoroscopy alone and the option to save these images for review (fluorography), thereby providing a possible lower radiation alternative to cineangiography. In this study, we aim to evaluate the efficacy and safety of fluorography imaging compared with standard cineangiography in the reduction of patient and operator radiation exposure during diagnostic coronary angiography.
Methods
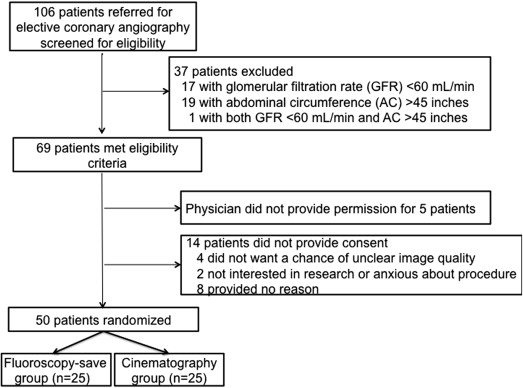
Subjects were scheduled for a diagnostic coronary angiogram at a single tertiary care center. Patients with chronic kidney disease, defined as an estimated glomerular filtration rate <60 ml/min, were excluded as it was unclear if more contrast would be used in the fluorography group compared with cineangiography group. In addition, an arbitrary abdominal circumference threshold of >45 inches was chosen as an additional exclusion criterion given that image quality decreases with increasing abdominal girth. Finally, patients undergoing emergent coronary angiography were also excluded ( Figure 1 ). New York University School of Medicine’s Institutional Review Board approved this trial, and all patients provided written informed consent. This study is registered at ClinicalTrials.gov (identifier: NCT01605045 ).
Participants were stratified by use of transfemoral versus transradial access, and randomized in blocks of 4 and 8 using opaque sealed envelopes, into 1 of 2 groups: fluorography group or cineangiography group. Patients randomized to the fluorography group had coronary angiography performed using the fluoroscopy-save function (retrospectively stored fluorography). Operators then had the option to repeat an injection of contrast under cineangiography only if they were unsatisfied with the quality of the image under fluorography alone. Patients randomized to cineangiography had coronary angiography performed and recorded using standard cineangiography.
Transfemoral or transradial access was obtained under sterile technique, followed by administration of either 500 U unfractionated heparin through a 6Fr transfemoral sheath or a cocktail of 2,500 U unfractionated heparin, 2.5 mg of verapamil, and 100 μg of nitroglycerin through a 5Fr transradial sheath. Contrast was administered by way of an automated injector (MEDRAD, MEDRAD Inc., Pittsburgh, Pennsylvania), and camera angles used were per operator discretion. Operators were asked to defer further imaging of peripheral arteries and the left ventricle and performance of percutaneous coronary intervention (PCI) until after radiation exposure measurements were collected. Pulsed fluoroscopy was used at a frame rate of 15 frames/s. The Artis zee coronary angiography system equipped with software version VC14 and lead shields (Siemens AG, Erlangen, Germany) and a ceiling-mounted lead shield were used for all procedures. The use of a RADPAD (Worldwide Innovations & Technologies Inc., Kansas City, Kansas) protective drape was encouraged when available.
Patient demographics and anthropometric data were recorded prospectively for all participants. Medical and surgical histories were obtained by way of chart review and confirmed by patient interview, and laboratory data were collected from chart review. Procedural characteristics were recorded in real time. Degree of coronary artery diameter stenosis was visually estimated by the operating attending physician.
The primary measurement was patient radiation exposure, measured by a 14″ × 17″ Gafchromic XR-RV3 film sheet (International Specialty Products, Wayne, New Jersey) placed underneath the patient during the procedure. Film sheets were quantitatively analyzed using the FilmQA-XR software (Ashland Inc., Covington, Kentucky) to quantitatively determine the amount of peak skin dose radiation exposure. Secondary measurements included kerma-area product (KAP) measured in μGy·m 2 and air kerma at the interventional reference point (Ka,r) measured in mGy by built-in software in the Siemens cardiac angiography system. Operator radiation exposure was measured in microroentgen by a dosimeter placed in the left upper pocket of the lead apron worn by the primary operator. This was converted to a dose in units of μGy using the appropriate f-factor of 115. All measurements of radiation were recorded immediately after diagnostic coronary angiography was completed.
The primary safety measurement was the rate of 30-day major adverse cardiac events, defined as a composite of all-cause mortality, occurrence of new myocardial infarction, or occurrence of repeat coronary angiography, determined by telephone interviews 30 days after the procedure. A secondary safety measurement was contrast use during coronary angiography, which was measured in real time.
Each patient had 1 image repeated in the alternate procedure with the same angulation for assessment of diagnostic quality. In the fluorography group, 1 picture not already repeated under cineangiography per operator discretion was reimaged using cineangiography. In the cineangiography group, 1 picture was repeated using fluorography. The designation of which image to repeat was determined at random before the procedure but not shared with the operator until after diagnostic imaging was complete. Once radiation data were collected, the operator was informed of which image to repeat using the alternate procedure. The fluorography and cineangiography images were then scrambled (no image appeared consecutively with its pair) and reviewed by 2 angiographers blinded to patient data, randomized group, and overall study design. The epicardial coronary artery of interest on left coronary artery injection was defined as the circumflex artery in caudal views, left anterior descending artery in cranial views, and left main artery in left anterior oblique caudal views.
Sample size was calculated based on observational data of mean radiation output (4199.4 ± 1340.4 μGy·m 2 ) during coronary angiography using standard cineangiography performed over 6 months in our catheterization laboratory. Using a 2-sided 2-sample t test, the number of patients needed in each group to observe a 25% decrease in radiation exposure in the fluorography versus cineangiography group at 80% power and a 0.05 significance level was estimated at 25 (total n = 50). Categorical variables are presented as proportions and compared using Fisher’s exact test, and skewed continuous variables (Shapiro-Wilk test) are presented as median (interquartile range) and were compared using Mann-Whitney test. Association between patient skin dose and KAP was assessed using Spearman’s correlation test. Significance level was set at 0.05, and statistical analysis was performed using SPSS 19.0 (SPSS Inc., Chicago, Illinois).
Results
Baseline demographic, clinical, and procedural characteristics, including RADPAD use, between patients in the fluorography and cineangiography groups were largely similar ( Tables 1 and 2 ), except for a greater proportion of patients with a history of PCI in the fluorography group compared with the cineangiography group.
| Variable | Fluorography (n = 25) | Cineangiography (n = 25) | p Value |
|---|---|---|---|
| Age (yrs) | 62 (53–73) | 65 (54–72) | 0.82 |
| Men | 16 (64) | 22 (88) | 0.10 |
| White | 9 (36) | 11 (44) | 0.29 |
| Black | 1 (4) | 5 (20) | |
| Hispanic | 2 (8) | 1 (4) | |
| Asian | 13 (52) | 8 (32) | |
| Body mass index (kg/m 2 ) | 26 (23–29) | 26 (22–28) | 0.29 |
| Abdominal circumference (inch) | 37 (35–42) | 38 (36–40) | 0.77 |
| Glomerular filtration rate (ml/min) | 84 (72–95) | 82 (76–100) | 0.39 |
| Previous PCI | 9 (36) | 2 (8) | 0.04 |
| Previous coronary artery bypass graft surgery | 2 (8) | 2 (8) | 1.00 |
| Indication for procedure | |||
| Atypical chest pain/dyspnea | 16 (64) | 14 (56) | 0.48 |
| Stable angina | 7 (28) | 5 (20) | |
| Unstable angina | 0 | 1 (4) | |
| Preoperative evaluation | 0 | 2 (8) | |
| Valvular disease | 2 (8) | 2 (8) | |
| Variable | Fluorography (n = 25) | Cineangiography (n = 25) | p Value |
|---|---|---|---|
| Access site | |||
| Radial | 12 (48) | 10 (40) | 0.54 |
| Femoral | 13 (52) | 14 (56) | |
| Radial-femoral crossover | 0 | 1 (4) | |
| Primary operator | |||
| First-year fellow | 9 (36) | 11 (44) | 0.08 |
| Physician’s assistant | 8 (32) | 1 (4) | |
| Interventional fellow | 6 (24) | 10 (40) | |
| Attending physician | 2 (8) | 3 (12) | |
| Difficulty navigating periphery | 1 (4) | 4 (16) | 0.35 |
| Right dominance | 23 (92) | 23 (92) | 1.00 |
| No. of views to visualize right coronary artery | |||
| 1 | 3 (12) | 6 (24) | 0.63 |
| 2 | 15 (60) | 13 (52) | |
| 3 | 5 (20) | 4 (16) | |
| No. of views to visualize left coronary artery | |||
| 3 | 2 (8) | 4 (16) | 0.58 |
| 4 | 15 (60) | 16 (64) | |
| 5 | 5 (20) | 2 (8) | |
| Radiation protection drape | 7 (28) | 7 (28) | 1.00 |
| Use of collimation | 20 (80) | 16 (64) | 0.35 |
| Degree of coronary artery narrowing | |||
| ≤30% Diameter stenosis | 12 (48) | 16 (64) | |
| 40%–69% Diameter stenosis | 6 (24) | 2 (8) | |
| No. of coronary arteries ≥70% narrowed | 0.29 | ||
| 1 | 4 (16) | 6 (24) | |
| 2 | 1 (4) | 1 (4) | |
| 3 | 2 (8) | 0 | |
| Proceed to PCI | 5 (20) | 4 (16) | 1.00 |
| Repeat injection under cineangiography | 12 (48) | — | — |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


