Six neonates weighing ≤2,500 g with native coarctation of the aorta underwent balloon dilation. Of the 6 neonates, 4 were female and 2 were male, with a mean age of 14 days (range 9 to 20) and a mean weight of 1,900 g (range 790 to 2,500). The procedure was acutely successful in all 6 patients; the peak gradient decreased from 38 ± 19 mm Hg to 11 ± 3 mm Hg. The diameter increased from 1.5 ± 0.6 mm to 3.6 ± 0.7 mm. Of the 6 patients, 3 had required no additional intervention at a mean of 42 months after the initial dilation, and 3 had developed restenosis a mean of 2.4 months after the initial dilation and underwent successful redilation. Of the latter 3 patients, 2 developed restenosis and underwent surgical repair 37 and 68 days after the second dilation, and 1 of these patients developed recoarctation after surgery that was treated successfully with balloon dilation 54 days after the end-to-end repair. In conclusion, premature neonates weighing ≤2,500 g with coarctation of the aorta appear to respond acutely to balloon dilation. Some patients will have a successful long-term result after a single balloon dilation procedure. However, restenosis is common and tends to develop rapidly.
Coarctation of the aorta (CoA) in premature infants with a low birth weight is a therapeutic challenge. Compared to normal-size neonates, surgery for CoA in newborns weighing ≤2,500 g is associated with an increase in mortality, morbidity, and restenosis. Balloon dilation (BD) of native CoA is controversial, particularly in infants. Limited data are available on the success of BD in premature infants. We reviewed our results of BD of a relatively discrete native CoA in 6 consecutive premature infants weighing ≤2,500 g.
Methods
From September 1998 to June 2008, 6 premature newborns weighing ≤2,500 g with native CoA underwent BD ( Table 1 ). The mean gestational age was 33.5 weeks (range 26 to 37), their mean age was 14 days, and the mean weight was 1,900 g. Of the 6 patients, 3 had isolated CoA, and 3 had additional lesions, including a large ventricular septal defect and an atrial septal defect in 1, a large patent ductus arteriosus in 1, and a bicuspid aortic valve in 1. The indications for intervention were a Doppler velocity of >3 m/s or an arm-to-leg blood pressure gradient >20 mm Hg, in the absence of a patent ductus arteriosus.
| Pt. No. | Age (days) | Weight (g) | Gender | Access and Sheath Size | Gradient (mm Hg) | Diameter (mm) | Outcome | ||
|---|---|---|---|---|---|---|---|---|---|
| Before Dilation | After Dilation | Before Dilation | After Dilation | ||||||
| 1 | 9 | 790 | Female | Umbilical/3Fr | 70 | 10 | 1.0 | 3.0 | R/S/R |
| 2 | 12 | 2,400 | Female | Femoral/3Fr | 45 | 12 | 1.3 | 4.5 | N |
| 3 | 12 | 1,500 | Male | Umbilical/4Fr | 15 ⁎ | 15 | 1.5 | 3.3 | R |
| 4 | 13 | 2,000 | Female | Femoral/3Fr | 39 | 5 | 1.3 | 2.9 | R/S |
| 5 | 17 | 2,200 | Male | Femoral/4Fr | 22 | 12 | 2.5 | 4.3 | N |
| 6 | 20 | 2,500 | Female | Femoral/4Fr | 35 | 11 | 1.3 | 3.5 | N |
The BD procedure has been previously described. All the patients underwent general anesthesia. Vascular access was through an umbilical artery in 2 patients and a femoral artery in 4 patients ( Table 1 ). The pressure gradients and angiographic findings were obtained using a pigtail catheter. The balloon size was within 0.5 mm of the size of the descending aorta at the diaphragm and did not exceed the diameter of the isthmus by >0.5 mm. The size of the inflated balloon was 4 mm in 3 patients and 5 mm in 3 patients. The balloon length was 1.5 to 2.0 cm. The balloon inflation pressures ranged from 4 to 10 atm. A procedure was considered successful if the residual peak systolic gradient across the CoA was ≤20 mm Hg. Statistical analysis was performed using Wilcoxon signed ranks tests for the pre- and postprocedure parameters.
Results
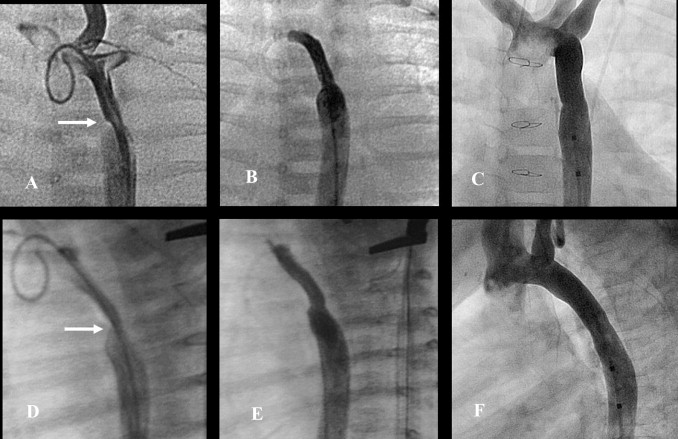
All 6 patients underwent successful initial BD. The peak systolic gradient decreased by 71%, from 38 ± 19 mm Hg to 11 ± 3 mm Hg (p <0.05). The minimum CoA diameter increased by 140%, from 1.5 ± 0.6 mm to 3.6 ± 0.7 mm (p <0.05). The balloon size/stenosis ratio was 3.2 ± 0.8. The CoA site was generally discrete. The isthmus was mildly hypoplastic in 3 patients and mildly to moderately hypoplastic in 1 patient ( Figure 1 ). One patient had a patent ductus arteriosus. After BD, all the patients had angiographic improvement; 2 developed intimal flaps ( Figure 2 ).

No complications related to the procedure developed. No extravasations of contrast material or aneurysms were observed. The 2 smallest patients (790 and 1,500 g) underwent BD through the umbilical artery. Of the other 4 patients (weight 2,000 to 2,500 g), who had undergone dilation through a femoral artery, 2 had transiently diminished distal pulses immediately after the procedure but required no therapy.
Of the 6 patients, 3 had required no reintervention at a mean of 42 months (range 31 to 57) after the initial BD ( Figures 1 and 2 ). In these patients, the subsequent clinic blood pressure gradients between the arms and legs ranged from 0 to 24 mm Hg, and the leg pulses were described as strong or normal. The most recent echocardiographic Doppler velocity distal to the CoA ranged from 1.9 to 2.4 m/s, without diastolic runoff. One patient underwent catheterization and angiography 57 months after BD for progressive subaortic stenosis; the residual gradient across the CoA was 3 mm Hg ( Figure 1 ).
The remaining 3 patients required repeat BD a mean of 71 days (range 48 to 96) after the initial BD. Of these 3 patients, 2 developed subsequent restenosis and underwent end-to-end surgical repair 37 and 68 days after the second BD. One of these patients developed restenosis, underwent a repeat BD procedure 54 days later ( Figure 3 ), and was free of additional recoarctation 58 months later.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


