Cardiac resynchronization therapy (CRT) is effective for the treatment of patients with heart failure and a wide QRS duration, particularly left bundle branch block. However, subjects with right bundle branch block (RBBB) do not appear to benefit from CRT. The aim of this study was to determine whether patients with specific RBBB conduction patterns responded to CRT in the Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy (MADIT-CRT) trial. In the present post hoc analysis, patients with RBBB who received CRT with an implantable cardioverter defibrillator (n = 132) were divided into 2 groups according to the baseline QRS morphology in the inferior and high lateral leads: group 1: left anterior fascicular block (LAFB) pattern (n = 80; 60.6%); and group 2: non-LAFB pattern (n = 52; 39.4%). Subjects with RBBB who received an implantable cardioverter defibrillator served as the control group (n = 87). The primary end point was echocardiographic response to CRT, defined as percent change in left ventricular (LV) and left atrial volumes from baseline to 1 year. The secondary end point was heart failure or death. The non-LAFB group demonstrated a significantly larger percent reduction in LV end-diastolic volume, LV end-systolic volume, and left atrial volume compared to controls (−11%, p <0.0001; −17%, p <0.0001; −15%, p <0.0001, respectively) and LAFB (−5%, p = 0.028; −7%, p = 0.019; −6%; p = 0.022; respectively) by multivariate analysis. No difference was found in the 3-year crude event rates for death or heart failure among the LAFB (22%), non-LAFB (21%), or ICD-only (20%) groups (p = NS). In conclusion, conduction patterns influence echocardiographic response to CRT in patients with RBBB, with favorable reductions in the LV and left atrial volumes in those without an LAFB conduction pattern. This echocardiographic benefit did not translate into a reduction in heart failure or death during a 3-year follow-up period.
Cardiac resynchronization therapy (CRT) is an effective treatment option for patients with left bundle branch block and refractory heart failure. For unclear reasons, those with right bundle branch block (RBBB) or nonspecific intraventricular conduction delay have not derived similar benefit. Using 3-dimensional nonfluoroscopic electroanatomic contact mapping, Fantoni et al described the biventricular electrical activation patterns in RBBB and left bundle branch block. The number and location of the left ventricular breakthrough sites differed in those with RBBB and correlated with differences in the QRS morphology on the surface electrocardiogram. In the presence of RBBB, vector analysis of the initial deflection of the QRS complex on the surface electrocardiogram identifies regions of earliest activation in the left ventricle. These observations provided the premise for our study to determine whether differences in the surface electrocardiographic QRS patterns, which likely represent different breakthrough sites, alter clinical response to CRT in patients with RBBB enrolled in the Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy (MADIT-CRT) trial.
Methods
The MADIT-CRT trial was a multicenter, prospective, randomized trial designed to assess whether CRT with an implantable cardioverter defibrillator (CRT-D) with biventricular pacing would reduce the risk of death or heart failure admissions in patients with mild heart failure symptoms (New York Heart Association class I to II heart failure) due to either ischemic or nonischemic cardiomyopathy (ejection fraction ≤30%) and a QRS duration of ≥130 ms. The subjects were randomized in a 3:2 ratio to receive either CRT-D or an ICD alone. The subjects enrolled in MADIT-CRT underwent detailed clinical and echocardiographic evaluations at baseline, with a repeat echocardiogram also obtained at the 12-month follow-up visit.
The baseline electrocardiograms obtained at enrollment were classified as showing left bundle branch block, RBBB, or intraventricular conduction delay according to the QRS morphology. The electrocardiograms were identified as showing RBBB if the QRS morphology in lead V 1 consisted of R, rR′, rsR′, rSR′, or qR and a terminal S wave was present in I, aVL, or V 6 .
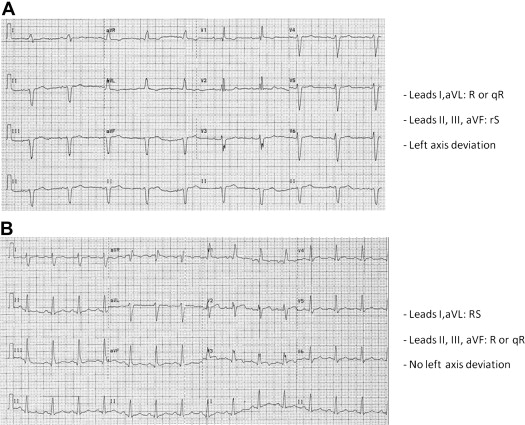
Using the electrocardiographic patterns associated with the biventricular activation maps from subjects with RBBB reported by Fantoni et al, the RBBB electrocardiograms were subdivided into 2 groups according to the QRS morphology in the inferior and high lateral leads for the present post hoc analysis. Patients with Q or rS morphology in leads II, III, and aVF and R or Rs waves in leads I and aVL were categorized as group 1, representing those with a left anterior fascicular block (LAFB) pattern, although strict axis definition was not always met for LAFB. The remaining patients with RBBB were categorized as group 2 (non-LAFB). Representative electrocardiograms from each group are shown in Figure 1 .
The primary end point for the present post hoc study was the response to CRT-D, defined echocardiographically as an overall improvement in left ventricular end-diastolic volume, left ventricular end-systolic volume, and left atrial volume from baseline to 12 months after enrollment. The secondary end point was death from any cause or nonfatal heart failure events, whichever occurred first during the 3-year follow-up period. The subjects with RBBB who received an ICD only served as the control group to provide a reference for the expected outcomes in those with RBBB who do not receive CRT-D.
Continuous variables are expressed as the mean ± SD and were compared using the paired Student t test or Wilcoxon’s rank sum test, as appropriate. Proportional variables are expressed as frequency counts or percentages, and differences were determined using the chi-square or Fisher exact test, as appropriate. The percent change in the left atrial and left ventricular volumes from baseline to the 12-month follow-up echocardiograms for both electrocardiographic patterns were estimated using multivariate linear regression models adjusted for age ≥65 years, female gender, ejection fraction ≤25%, ischemic cardiomyopathy, QRS ≥150 ms, and blood urea nitrogen >25 mg/dl. The Kaplan-Meier life-table method was used to calculate death and heart failure event rates over time according to treatment arm and electrocardiographic pattern. Cox proportional hazards regression models were used to evaluate the risk (hazard ratio) of death or heart failure events according to treatment arm and electrocardiographic pattern. The covariates adjusted for included age ≥65 years, female gender, ejection fraction ≤25%, ischemic cardiomyopathy, QRS ≥150 ms, and blood urea nitrogen >25 mg/dl. All statistical tests were 2-tailed. A p value <0.05 was considered statistically significant. Data were analyzed using Statistical Analysis Systems, version 9.3 (SAS Institute, Cary, North Carolina).
Results
A total of 219 subjects (12.5%) enrolled in the MADIT-CRT trial with technically satisfactory electrocardiograms were classified as having RBBB. Of these 219 patients, 87 received an ICD and 132 received CRT-D. The baseline characteristics of the study population are listed in Table 1 , with the CRT-D group divided into those with and without an LAFB conduction pattern. Technically adequate baseline and 12-month follow-up echocardiograms were available for 74 (85%) of the ICD control group and 79 (60%) of the CRT-D group.
| Variable | ICD (n = 87) | CRT-D (n = 132) | |
|---|---|---|---|
| LAFB Pattern (n = 80) | Non-LAFB Pattern (n = 52) | ||
| Age (yrs) | 64.3 ± 9.7 | 68.2 ± 9.9 ∗ | 63.5 ± 11.3 |
| Age ≥65 yrs | 44 (51) | 53 (66) | 29 (56) |
| Women | 6 (7) | 7 (9) | 5 (10) |
| Ischemic cardiomyopathy | 74 (85) | 69 (86) | 47 (90) |
| NYHA class I | 20 (23) | 17 (21) | 9 (17) |
| QRS duration (ms) | 150.5 ± 13.8 | 155.2 ± 15.7 † | 152.5 ± 14.0 |
| QRS ≥150 ms | 39 (45) | 51 (64) † | 29 (56) |
| Creatinine (mg/dl) | 1.30 ± 0.7 | 1.25 ± 0.3 | 1.29 ± 0.4 |
| BUN >25 mg/dl | 23 (27) | 25 (31) | 13 (25) |
| Diabetes mellitus | 30 (35) | 28 (35) | 13 (25) |
| LVEDV index (ml/m 2 ) | 113.5 ± 22.4 | 110.5 ± 22.8 | 108.6 ± 20.4 |
| LVESV index (ml/m 2 ) | 80.0 ± 17.6 | 77.5 ± 17.7 | 76.4 ± 15.7 |
| LAV index (ml/m 2 ) | 45.6 ± 10.2 | 44.4 ± 11.2 | 43.8 ± 10.1 |
| LVEF (%) | 25 ± 5 | 25 ± 5 | 26 ± 5 |
| LVEF ≤25% | 48 (55) | 51 (64) | 26 (50) |
∗ p = 0.01 LAFB versus non-LAFB.
The mean percent change between baseline and 12-month echocardiographic parameters (left ventricular end-diastolic volume, left ventricular end-systolic volume, and left atrial volume) was greater for group 2 (non-LAFB pattern) than for group 1 (LAFB pattern) or the control group ( Figure 2 ). Uniformly, the non-LAFB pattern group demonstrated a larger percent decrease in left ventricular end-diastolic volume, left ventricular end-systolic volume, and left atrial volume compared with either the control group (−11%, p <0.0001; −17%, p <0.0001; −15%, p <0.0001) or LAFB pattern group (−5%, p = 0.028; −7%, p = 0.019; −6%; p = 0.022; respectively). The percent increase in left ventricular ejection fraction after 12 months of CRT was also greater for group 2 (non-LAFB) than for the controls (+6%, p <0.001) or group 1 (+3%; p = 0.008).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


