The influence of volume overload on ventricular performance has been previously investigated but primarily with respect to the duration of overload. The aim of the present study was to elucidate whether the magnitude of the preoperative volume overload, represented by the ventricular volume, has any effect on ventricular performance long after the Fontan operation in patients with tricuspid atresia. We evaluated consecutive changes in hemodynamic catheterization data obtained at 1, 5, and 10 years after primary Fontan repair. The variables were compared between patients with larger (n = 20) and smaller (n = 21) ventricles (preoperative end-diastolic volume [percentage of predicted] 262 ± 33%, maximum 320% vs 182 ± 22%, minimum 133%, respectively). In a subgroup of patients (n = 33) who underwent symptom-limited exercise at 10.7 ± 3.0 postoperative years, the peak oxygen uptake was measured, and the potential predictors were interrogated. The difference in ventricular contractility between the groups tended to increase with time, with those with a larger ventricle showing poorer contraction, irrespective of whether it was assessed in a load-dependent (ejection fraction) or load-independent (end-systolic elastance) manner. The differences in these variables reached statistical significance at 10 years (p = 0.028 and p = 0.032). Multivariate analysis indicated a larger ventricle was an independent risk factor of poorer aerobic capacity (p = 0.047). In conclusion, ventricular performance was less preserved in those with a larger ventricle, which might result in suboptimal aerobic capacity. Our findings suggest not only early unloading, but also avoidance of excessive volume overload is of importance to minimize the deleterious effect of volume overload on an inherently susceptible ventricle.
The effect of volume overload on ventricular performance has been extensively investigated previously but primarily with respect to the duration. Consequently, together with the introduction of the staged Fontan approach, the current consensus has placed an emphasis exclusively on the duration of overload, favoring early unloading. Even with this approach, however, a decrease in functional capacity or premature death is still a concern. Although a variety of factors have been implicated as causative mechanisms of such continuing attrition, preserving ventricular function remains a key to success. Striving to achieve better outcome, a newer strategy, recently proposed, allows reduced pulmonary blood flow during the palliative state to address not only the duration, but also the magnitude, of volume overload. Despite its theoretical advantage, it is arguable whether such a “low-flow” strategy offers any additional benefit compared to the current one. With this controversy in mind, we evaluated consecutive changes in ventricular performance after the Fontan repair, focusing on the effect of preoperative ventricular volume as a potential predictor of the long-term outcome.
Methods
The participating institutions provided institutional ethical review and approval for the present study. All patients with tricuspid atresia who had undergone a nonfenestrated, primary Fontan operation (i.e., without a previous Glenn procedure) were identified by a search of the combined surgical database. The study subjects were eligible if they had been ≤6 years old at Fontan surgery, because a prolonged period of hypoxia could adversely affect long-term ventricular function. The subjects were deemed ineligible if they had a pacemaker, atrioventricular valvar regurgitation of mild or greater degree, or a history of ventricular septectomy that caused ventricular dysfunction. The study population was confined to those with tricuspid atresia, because the type of dominant ventricular chamber significantly affects ventricular performance. Furthermore, ventricular function differs considerably even among hearts with the same type of ventricular morphology, depending on the fundamental diagnosis. The study population was also limited to those who had undergone primary Fontan repair, because a staged approach substantially alters ventricular performance.
After a detailed review of medical record of potential candidates, 41 patients met the inclusion criteria. They were divided into 2 groups according to the percentage of predicted value of the end-diastolic volume (EDV) of the systemic left ventricle angiographically estimated before Fontan repair (smaller pre-EDV n = 21 and larger pre-EDV n = 20). The patient characteristics are listed in Table 1 . The differences between the groups were statistically significant for preoperative Qp/Qs and arterial oxygen saturation but not for previous palliation, age, or type of Fontan repair.
| Variable | Pre-EDV | p Value | |
|---|---|---|---|
| Small (n = 21) | Large (n = 20) | ||
| Female gender | 10 (48%) | 8 (40%) | 0.756 |
| Age at Fontan (years) | 2.5 ± 1.4 | 3.1 ± 1.4 | 0.132 |
| Weight (kg) | 9.9 ± 1.8 | 11.2 ± 2.4 | 0.078 |
| Height (cm) | 79.1 ± 19.4 | 87.9 ± 10.9 | 0.099 |
| Follow-up (years) | 15.0 ± 6.7 | 17.0 ± 5.5 | 0.302 |
| Palliation type | |||
| Systemic pulmonary shunt | 13 (62%) | 13 (65%) | 0.837 |
| Pulmonary arterial band | 6 (29%) | 4 (20%) | 0.523 |
| Hemodynamics | |||
| Qp/Qs | 1.1 ± 0.3 | 1.6 ± 0.6 | 0.005* |
| Mean pulmonary arterial pressure (mm Hg) | 13.1 ± 4.8 | 14.6 ± 5.7 | 0.376 |
| Hemoglobin (g/dl) | 16.4 ± 2.0 | 15.9 ± 1.5 | 0.364 |
| Arterial oxygen saturation (%) | 78.1 ± 5.2 | 81.1 ± 4.2 | 0.047* |
| Type of Fontan | |||
| Total cavopulmonary connection | 15 (71%) | 11 (55%) | 0.275 |
In our centers, Fontan survivors are routinely scheduled for repeat catheterization at 1, 5, and 10 years after surgery according to a standardized protocol. Thus, all 41 patients had undergone catheterization pre- and postoperatively, except for 6 who had not undergone the 5-year examination because of medical and/or social reasons and another 8 patients who had not yet reached 10 years postoperatively. Accordingly, 27 patients had completed the entire set of repeat catheterizations and 14 had undergone postoperative examinations twice at either 1 and 5 years or 1 and 10 years. All the patients were discharged with anticoagulants and diuretics. These medications were discontinued 1 year postoperatively unless otherwise specifically required. Using this regimen, all 41 patients were free of any cardiovascular agents at 10 years postoperatively, except for 4 (1 was taking diuretics, 2 a β blocker, and 1 a β blocker and enalapril). No patient required any type of inotropic agents.
Biplane cine-ventriculography was performed with a film speed of 60 frames/s. We used Simpson’s rule or the area-length method to estimate the left ventricular (LV) volume at the end-diastolic and end-systolic phases. The EDV of the systemic left ventricle is expressed as the percentage of the predicted normal value. The EDV and end-systolic volume were also indexed by dividing these values by the body surface area of the corresponding patient. The LV ejection fraction (EF) was calculated as the ratio of the stroke volume to the EDV. We measured the pressure in the LV chamber at the end-systolic and end-diastolic phases. The central venous pressure was also obtained. Oxygen consumption was estimated from the age, gender, and heart rate data. The cardiac index (L/min/m 2 ) was measured using the Fick principle, with the assumption that the right and left pulmonary arterial saturation were equivalent.
We performed a simulation of ventricular pressure-volume framework analysis using the method described by Tanoue et al, because this permitted us to appreciate a load-independent state of ventricular performance. The ventricular contractility (end-systolic elastance [Ees]) and ventricular afterload (effective arterial elastance [Ea]) were approximated using catheterization data. The equations used were as follows: Ees = mean arterial pressure/minimal ventricular volume, and Ea = maximal ventricular pressure/(maximal ventricular volume − minimal ventricular volume). The Ea/Ees ratio was subsequently calculated and represents the ventriculoarterial coupling. This value was then used to estimate ventricular mechanical efficiency, defined as a ratio of stroke work to the pressure–volume area. The following equation was used: stroke work/pressure–volume area = 1/(1 + 0.5 Ea/Ees).
To keep the exercise protocol consistent, the analysis on aerobic exercise capacity was confined to the patients from a single institution. Thus, 33 patients underwent symptom-limited exercise using a motor-driven, programmable treadmill (Q-5000 System, Quinton, Seattle, Washington) at a mean interval of 10.7 ± 3.0 years postoperatively. The ventilation and gas exchange were measured using a breath-by-breath method and hot-wire anemometer (Riko AS500, Minato Medical Science, Japan) connected to a mass spectrometer (MG-300, Perkins Elmer, St. Louis, Missouri). The peak oxygen uptake was measured and calculated as the percentage of the body weight-predicted normal value for the corresponding institution.
The data are expressed as the mean ± SD. p Values of <0.05 were considered statistically significant. Intergroup comparisons were made using an unpaired Student’s t test for the variables at 10 postoperative years. Multiple linear regression analysis was used to investigate the independent association of potential predictors with the percentage of the predicted peak oxygen uptake. The variables were regarded as candidate predictors in the multivariate model if the corresponding p value was <0.10. The Statistical Package for Social Sciences statistical software program, version 11.0.1J (SPSS Japan) was used for all statistical analyses.
Results
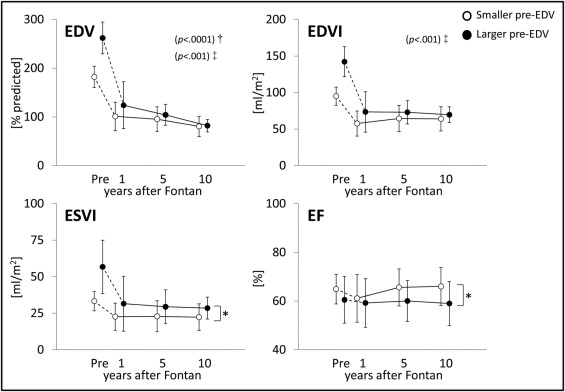
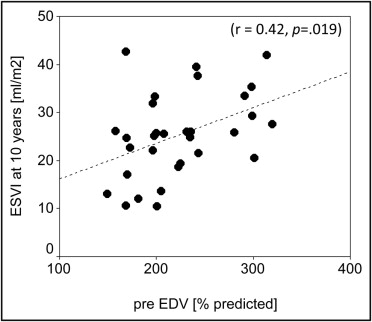
The EDV had decreased steeply at 1 year in both groups, with the patients with a larger pre-EDV experiencing a greater reduction than those with a smaller pre-EDV (change in EDV 141.1 ± 70.2% vs 80.4 ± 34.7%, respectively, p = 0.005). This sudden decrease was followed by a steady phase in which the serial change was gradual ( Figure 1 ). The mode of change in the EDV during the postoperative period appeared to be slightly different depending on the standardization type. Thus, the percentage of predicted EDV decreased slowly, and the EDV index was nearly constant. Regardless of the standardization methods, a trend was seen for a gradual decrease in the difference between the groups, yielding an almost identical EDV at 10 years for both groups. This was in marked contrast to the serial changes in the end-systolic volume. The difference in the end-systolic volume tended to persist postoperatively and had reached statistical significance at 10 years (p = 0.049). The end-systolic volume at 10 years was positively (p = 0.019) associated with the pre-EDV ( Figure 2 ). Consequently, serial changes in the EF showed a trend toward a gradual increase in the discrepancy between the 2 groups, with the difference at 10 years statistically significant (p = 0.028).
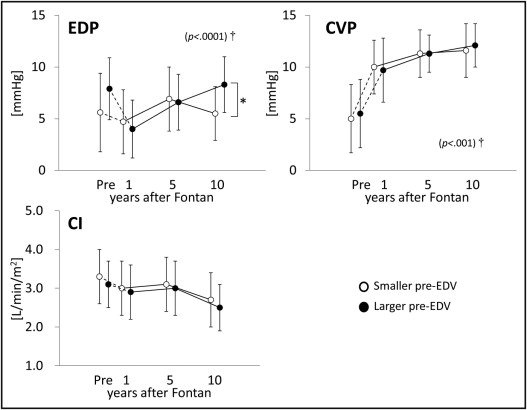
The end-diastolic pressure in those with a greater pre-EDV had decreased more significantly at 1 year than in those with a lower pre-EDV (change in end-diastolic pressure 3.9 ± 3.5 vs 1.0 ± 4.2 mm Hg, p = 0.019), yielding an almost identical end-diastolic pressure at 1 year for both groups ( Figure 3 ). A subsequent change in each group was apparently distinctive. The end-diastolic pressure in those with a greater pre-EDV steadily increased with time but did not in those with a lower pre-EDV, eventually resulting in a significant difference at 10 years (p = 0.005). In contrast, the serial changes in central venous pressure and cardiac index were virtually identical.
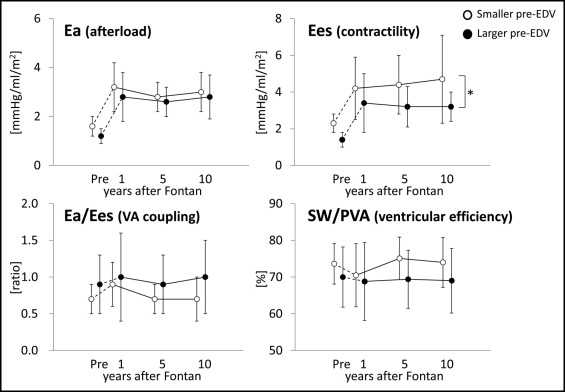
The Ea had markedly increased at 1 year in both groups, followed by persistently elevated and almost identical values for both groups ( Figure 4 ). The Ees had also markedly increased at 1 year in both groups. Unlike the Ea, however, the serial changes in Ees showed a trend toward a gradual increase in the difference between the 2 groups with time, leading to a significant difference at 10 years (p = 0.032); this also occurred with the EF. Similar tendencies were observed in the Ea/Ees and stroke work/pressure–volume area ratios, although the differences in these variables had not reached statistical significance at 10 years.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


