Long-term data on the effects of cholesterol-lowering regimens on low-density lipoprotein cholesterol levels and cardiovascular events in patients with familial hypercholesterolemia (FH) are lacking. The present study evaluated the effectiveness of long-term intensive lipid-lowering therapy on the natural history of FH. Of approximately 1,000 adult patients with heterozygous FH treated from 1974 to 2008, the charts of 327 were randomly selected for review. FH was defined according to the Simon Broome Registry Group criteria. The recorded data included age; gender; lipid levels with diet only, with each lipid-lowering regimen, and at the most recent visit during treatment; the length of follow-up; cardiovascular events; and revascularization procedures. The lipid assay calibrations and standardization were unchanged throughout the study period. Of the 327 patients, 60% were men, the mean age at diagnosis was 38 ± 14 years, and the mean follow-up was 15 ± 8 years. The baseline and most recent low-density lipoprotein cholesterol levels during treatment were 256 ± 60 mg/dl and 116 ± 46 mg/dl, respectively, for a mean reduction of 55% from baseline (p <0.0001). At their most recent visit, 24% of all subjects were treated with statin monotherapy, 55% with a statin plus another agent, and 21% with triple therapy; 44% received a statin-ezetimibe combination. The interval between recurrent cardiovascular events tended to increase from 5.3 ± 4.8 years before treatment to 7.4 ± 6.7 years after referral (p = 0.1303). In conclusion, advances in drug therapy during the past 3 decades has led to substantial reductions in low-density lipoprotein cholesterol levels and appears to diminish the cardiovascular risk in patients with FH.
Familial hypercholesterolemia (FH) is an inherited condition that results in lifelong high low-density lipoprotein (LDL) cholesterol levels. The elevated LDL cholesterol levels are due to a number of potential genetic defects resulting in reduced LDL clearance. Foremost among these is an autosomal dominant defect in the LDL receptor. Even in the heterozygous form, the consequences of FH are a premature and significantly increased risk of coronary heart disease. Historical data analyses and registries of heterozygous FH revealed a >50% cumulative risk of fatal and nonfatal coronary heart disease by age 50 years in men and a similar rate in women a decade or so later. Although placebo control outcome trials have not been performed in the FH population, numerous subjects with heterozygous FH were included in long-term lipid-lowering trials such as the Lipid Research Clinics Coronary Primary Prevention Trial (LRC-CPPT) and the Scandinavian Simvastatin Survival Study (4S). These trials showed that LDL cholesterol level reduction with bile acid sequestrant resins and simvastatin against placebo resulted in a significant cardiovascular (CV) risk reduction in the primary and secondary prevention settings, respectively. The goals of the present study were to evaluate the effectiveness of long-term, intensive, lipid-lowering therapy on the LDL cholesterol levels and its effect on the natural history of FH.
Methods
The charts of 327 of approximately 1,000 adults with heterozygous FH (>18 years old at the first visit), who were treated at the Cholesterol Treatment Center (Cincinnati, Ohio) from 1974 to 2008, were randomly selected and reviewed. FH was defined clinically according the Simon Broome Registry group criteria.
The following data were recorded for each patient: gender; age at diagnosis; lipid levels with diet only, with each lipid-lowering medication, and at the most recent visit during treatment; and the length of follow-up. Symptomatic CV events, including revascularization procedures before treatment at the center and during follow-up, were also recorded (events were recorded in years; thus, 2 events occurring in the same year were counted as 1 event).
The routine lipid analyses (total cholesterol, high-density lipoprotein cholesterol, triglycerides, and calculated LDL cholesterol using the Fredrickson formula) were assayed at a Centers for Disease Control and Prevention-National Heart, Lung Blood Institute, part III, standardized laboratory that maintained Part 3 Standardization using calibrators either supplied by the Centers for Disease Control and Prevention or extensively assayed and assigned target values by the Centers for Disease Control and Prevention lipid STB branch. The laboratory focused on long-term clinical trials, and the extensive qualities efficiency was maintained and showed minimal drift for 30 years.
The demographic characteristics are presented as the mean ± SD for quantitative variables and as the count and percentage for categorical variables. The mean ± SD were provided for the summary of lipid parameters (i.e., total cholesterol, LDL cholesterol, high-density lipoprotein cholesterol, and triglycerides) for the initial untreated levels and for the most recent treated levels. The percentage of change between the 2 values was calculated.
The mean number of CV events, mean age at the first event, mean number of subjects with recurrent events, and mean number of years between recurrent events were recorded before and during the diagnosis/follow-up period. An analysis of variance model was used to determine whether a significant difference was present in the mean number of years between recurrent events between the 2 groups.
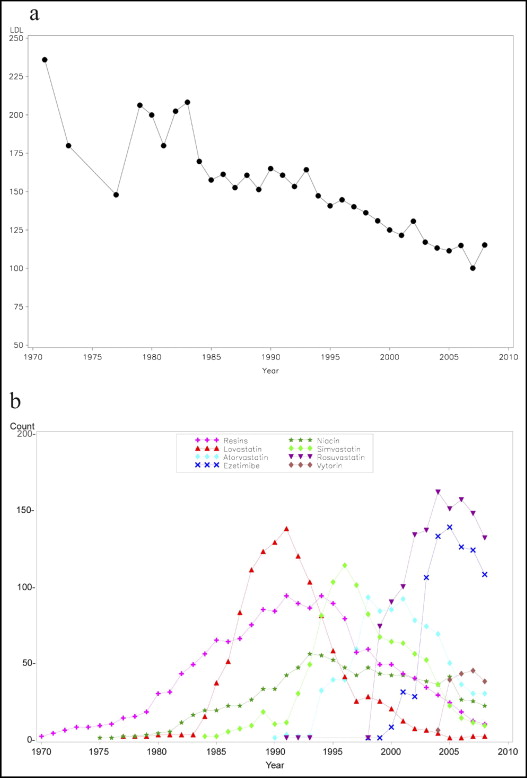
The mean LDL cholesterol levels were plotted by year and prescribed medications.
Results
Data were collected from 327 patients, approximately 1/3 of the 1,000 patients with heterozygous FH at our center. Of these, 195 (60%) were men and 132 (40%) were women. The demographic characteristics are listed in Table 1 . No significant differences were found in the demographics between genders (data not shown). The mean follow-up period was 15 ± 8 years (range 1 to 35).
| Parameter | Value |
|---|---|
| Gender | |
| Men | 195 (60%) |
| Women | 132 (40%) |
| Mean age at diagnosis (years) (n = 305) | 38 ± 14 (range 2–73) |
| Mean age at first visit (years) (n = 327) | 45 ± 13 (range 19–77) |
| Smoking status at first visit | |
| Nonsmoker | 195 (60%) |
| Smoker | 33 (10%) |
| Past smoker | 59 (18%) |
| No data | 40 (12%) |
| Duration of follow-up (years) (n = 327) | 15 ± 8 (range 1–35) |
The untreated and most recent lipid levels during treatment and the percentage of change are listed in Table 2 . The serum total cholesterol and LDL cholesterol levels with diet alone were reduced by 42% and 55% (p <0.0001), respectively, at the most recent follow-up visit with treatment. No significant difference was found between genders either at baseline or during treatment (data not shown). The LDL cholesterol level during treatment was <130 mg/dl in 60%, <100 mg/dl in 30%, and <70 mg/dl in 10%.
| Variable | Initial Untreated Level | Most Recent Treated Level | Change (%) | p Value |
|---|---|---|---|---|
| Total cholesterol (mg/dl) | 340 ± 68 | 195 ± 51 | −42% | <0.0001 |
| LDL cholesterol (mg/dl) | 256 ± 60 | 116 ± 46 | −55% | <0.0001 |
| HDL cholesterol (mg/dl) | 49 ± 14 | 54 ± 16 | +8% | <0.0001 |
| Triglycerides (mg/dl) | 146 ± 86 | 123 ± 71 | −15% | 0.3747 |
At the most recent visit, 24% of all subjects were treated with statin monotherapy, 55% with statin plus 1 other agent, and 21% with a statin and 2 other agents. Of the patients taking statins, 51% were taking rosuvastatin, and 44% were treated with a statin-ezetimibe combination regimen. The most common combination was rosuvastatin and ezetimibe (25%). Niacin and resins were mainly used as a third medication ( Table 3 ).
| Variable | Value |
|---|---|
| Patients taking single medication | 76 (24%) |
| Rosuvastatin | 37 (11%) |
| Atorvastatin | 21 (6%) |
| Simvastatin | 12 (4%) |
| Patients taking statin plus 1 other agent | 180 (55%) |
| Rosuvastatin, ezetimibe | 81 (25%) |
| Simvastatin, ezetimibe | 46 (14%) |
| Atorvastatin, ezetimibe | 15 (5%) |
| Patients taking statin and 2 other medications | 69 (21%) |
| Rosuvastatin, ezetimibe, niacin | 13 (40%) |
The decrease in the mean LDL cholesterol levels during the 30-year period and the relation to the various lipid-lowering medications are shown in Figure 1 . Each major decrease in the mean LDL cholesterol level was accompanied by the increasing use of a new lipid-lowering agent.