We assessed the long-term (>10 years) clinical course of patients with documented coronary lesions deemed nonsignificant according to fractional flow reserve (FFR) assessment and investigated whether the initial FFR value impacted on prognosis. From January 2000 to October 2003, all patients submitted to coronary angiography with FFR measurement were included in a single-center, prospective registry. Patients with an FFR value >0.80 were treated medically without revascularization. Major adverse cardiac events (MACE) (death, acute coronary syndrome (ACS), or coronary revascularization) were compared according to initial FFR value (absolute value and by category, ≤0.90 vs >0.90). Analyses were performed using a multivariable Cox model and propensity score matching. Among 257 patients (332 lesions) treated medically initially, 131 (51%, 143 lesions) had FFR ≤0.90 and 126 (49%, 189 lesions) >0.90. During follow-up (median duration, 11.6 years), 82 (31.9%) had a MACE, 38 (14.8%) died, 17 (6.6%) had ACS, 93 (36.2%) had repeat coronary angiography, and 27 (10.5%) had revascularization. There was no clinical, biologic or angiographic difference between patients with initial FFR value ≤0.90 versus >0.90. Adjusted Cox model showed no difference in relative risk of MACE, death, ACS, or revascularization. Coronary angiographies were numerically more frequent in patients with FFR ≤0.90, versus FFR >0.90. These findings were confirmed by propensity score–matched comparison. In patients with coronary narrowings left unrevascularized based on FFR, an FFR value between 0.80 and 0.90 has no impact on long-term outcome compared with those with FFR >0.90. In conclusion, patients with high FFR values should not be considered as having a lower risk of coronary event.
The safety of deferring patients with or without revascularization according to fractional flow reserve (FFR) has been demonstrated through randomized studies. Registry studies have confirmed the safety and efficacy of FFR guidance in making revascularization decisions in routine practice, with follow-up of up to 7 years. The threshold FFR value of 0.80 is widely accepted, taking into account the reproducibility of the measurement. Given the progression of atherosclerotic disease, it seems intuitive that the risk of events would gradually decrease with increasing values of FFR and that patients left without revascularization with a “low” FFR (i.e., 0.80 to 0.90) might be at higher risk of ischemia or complications than those with higher values (>0.90). We aimed to assess, in patients left without revascularization, whether the absolute value of FFR (0.80 to 0.90 vs >0.90) had any impact on the rate of clinical events in the very long term (>10 years).
Methods
From January 2000 to October 2003, among 6,288 patients submitted to coronary angiography, all patients submitted to coronary angiography with measurement of FFR in 1 or more of the 3 major epicardial vessels were included in a single-center prospective registry. FFR measurement was strongly encouraged in all patients with intermediate coronary lesions (defined as an angiographic diameter of stenosis between 40% and 70% on visual estimation) and without demonstrable ischemia. Initial FFR was measured using a wire fitted with a pressure sensor at the tip of the catheter (Volcano, San Diego, California) and analyzed according to the recommended technique, with 4Fr to 6Fr diameter catheters during maximal hyperemia induced by injection of an intracoronary bolus of adenosine (effect similar to 140 μg intravenous ). The average of 3 consecutive FFR measurements was recorded, and the decision to proceed to revascularization was made according to a threshold value of 0.80. At discharge and during follow-up, secondary prevention was given according to contemporary guidelines. In case of multivessel disease, the lesion with the lowest FFR value was considered as the primary lesion. In total, 407 patients were included, the median value of FFR was 0.85 ± 11. Based on FFR values, 136 of 407 (33.5%) immediately proceeded to revascularization, and 271 (66.5%) were treated medically. At 1 year, there was no significant difference in the rate of occurrence of adverse events, namely death, infarction, or need for revascularization. One-year follow-up of the study population has previously been published elsewhere.
The present study reports the long-term follow-up (at least 10 years) in terms of coronary clinical events of all patients with an initial FFR value >0.80 and not initially treated by revascularization. For the patient-level analysis, the primary end point was a composite of major adverse cardiac events (MACE) comprising all-cause death, acute coronary syndrome (ACS), or revascularization. Secondary end points were all-cause death, ACS, and revascularization considered separately. For lesion-level analysis, the end point was FFR site event (FFR lesion ACS or FFR lesion revascularization for stable ischemia). Follow-up information was obtained by a dedicated team of clinical research assistants who were blinded to initial management and initial FFR values. Information was obtained by direct or telephone contact with the patient, their family, or general practitioner or from hospital medical records. All patients received written information explaining the objectives of the study, and all participants gave written consent for the follow-up. The study protocol received ethics committee approval.
Quantitative data are presented as mean ± SD and qualitative data as number (percentage). The probability of MACE at 10 years was estimated using multivariate logistic regression with candidate variables including clinical characteristics (age, gender, cardiovascular risk factors, previous history of infarction, stroke, or heart failure), the indication for and outcome of coronary angiography (indication for angiography [stable/unstable angina, ACS, silent ischemia, other], number and localization of diseased vessels, left ventricular ejection fraction [LVEF]), and the discharge treatment (aspirin, clopidogrel, β blocker, angiotensin-converting enzyme inhibitor, and dose of statins). The association between initial FFR value and probability of occurrence of a MACE at 10 years was tested as follows: (1) by the proportion of patients with MACE during follow-up according to deciles of FFR value and by the correlation between FFR and the adjusted probability of MACE at 10 years and (2) by the comparison of 2 groups according to initial FFR value (0.80 to 0.90) and >0.90 (cut off selected as the median value of FFR). Groups were compared using the chi-square test or analysis of variance as appropriate. Event-free survival probability was calculated using the Kaplan-Meier method. Multivariate analysis was performed using Cox’s proportional hazards model taking into account the same variables as for the logistic regression plus the date of the event or length of follow-up. Results are given as hazard ratios (HRs) with 95% CIs. Using nonparsimonious logistic regression, a propensity score (propensity to have FFR >0.90) was calculated. A 1:1 matching was performed on the propensity score. Matched pairs were compared by conditional logistic regression. Survival curves were generated using the Kaplan-Meier method and compared with the log-rank test. Analyses were performed at patient level and repeated at lesion level. All tests were 2 sided; a p value <0.05 was considered statistically significant. All analyses were performed using SAS, version 9.3 (SAS Institute Inc., Cary, North Carolina).
Results
Among the 271 patients initially treated medically, 257 (95%) (332 lesions) had complete follow-up. During follow-up (median duration, 11.6 years), 82 patients (31.9%) had a MACE: 38 patients (14.8%) died, 17 (6.6%) had ACS, 93 (36.2%) underwent repeat coronary angiography, and 27 (10.5%) underwent revascularization. Multivariate analysis showed that age and LVEF were significantly associated with major adverse events at 10 years, whereas diabetes, hypertension, and heart failure were associated with death at 10 years.
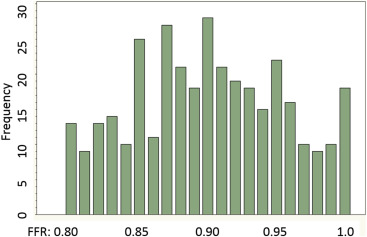
FFR values were normally distributed in patients who were initially treated by medical therapy ( Figure 1 ). The mean value was 0.90 ± 0.06 and median was 0.90 (interquartile range 0.87 to 0.95). There was no relation between FFR value and MACE. The proportion of patients with MACE during follow-up did not differ according to deciles of FFR value ( Supplementary Figure S1 ), and the correlation between FFR and the adjusted probability of MACE at 10 years was nonsignificant (y = 0.42 + 0.25 ×FFR, p = 0.66, r 2 = 0.098) ( Supplementary Figure S2 ). By adjusted Cox analysis, older age (HR 1.1, 95% CI 1.04 to 1.15 per year of age, p <0.001) and lower LVEF (HR 0.96 95% CI 0.93 to 0.98 per 1% increase of LVEF, p = 0.002) were associated with MACE but not FFR group (HR 1.03 95% CI 0.65 to 1.64 for FFR 0.80 to 0.9 vs >0.90, p = 0.88). FFR was not significantly associated with MACE, death, ACS, or revascularization analyzed individually. Lesion-level analyses yielded similar results ( Supplementary Table 1 ).
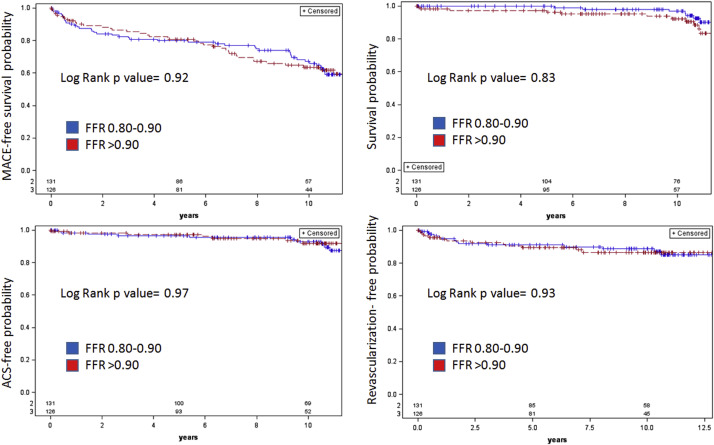
There was no significant difference in baseline characteristics according to FFR group ( Table 1 ). Discharge treatments were also comparable ( Table 2 ). The rates of MACE, death, ACS, and revascularization were comparable between groups ( Table 2 ). There was a numerically higher number of coronary angiographies in the group with lower FFR, but the difference was not significant. The Kaplan-Meier curves for MACE, death, ACS, and revascularization were similar ( Figure 2 ). Propensity score matching yielded a cohort of 182 patients (91 pairs). The comparison of baseline characteristics, treatments, and outcomes in the population of pairs matched on propensity score are presented in Table 1 . Kaplan-Meier curves for all end points were not significantly different ( Figure 3 ). Cox multivariable analysis confirmed that neither FFR absolute value nor FFR by category (0.80 to 0.90 vs >0.90) was significantly associated with MACE, death, ACS, or revascularization ( Supplementary Table 1 ).
| FFR | P value | FFR | P value | |||
|---|---|---|---|---|---|---|
| ≤0.90 (n=131) | >0.90 (n=126) | ≤0.90 (n=91) | >0.90 (n=91) | |||
| Age (years) | 62± 11 | 64 ± 11 | 0.08 | 63 ±10 | 63 ±11 | 0.78 |
| Male sex | 101 (77%) | 102 (81%) | 0.41 | 71 (78%) | 74 (81%) | 0.58 |
| Hypertension | 68 (52%) | 59 (47%) | 0.34 | 42 (46%) | 43 (47%) | 0.88 |
| Diabetes mellitus | 32 (25%) | 32 (25%) | 0.91 | 25 (27%) | 22 (24%) | 0.61 |
| Dyslipidemia | 90 (68%) | 95 (75%) | 0.20 | 64 (70%) | 67 (74%) | 0.62 |
| Left ventricular ejection fraction (%) | 60 ± 11% | 58 ± 12% | 0.55 | 60±10% | 59±11% | 0.78 |
| Indication for angiography | ||||||
| Stable/silent angina pectoris | 95 (73%) | 90 (71%) | 0.78 | 66 (72%) | 64 (70%) | 0.74 |
| Unstable angina pectoris | 7 (5%) | 13 (10%) | 0.14 | 6 (7%) | 7 (8%) | 0.77 |
| Acute myocardial infarction (non culprit lesion) | 29 (22) | 23 (18%) | 0.49 | 19 (21%) | 20 (22%) | 0.85 |
| STEMI | 9 (7%) | 7 (6%) | 6 (7%) | 7 (8%) | ||
| NSTEMI | 20 (15%) | 16 (13%) | 14 (15%) | 14 (15%) | ||
| No. of coronary arteries narrowed | ||||||
| 1 | 94 (72%) | 98 (78%) | 65(71%) | 73(82%) | ||
| 2 | 26 (20%) | 19 (15%) | 0.54 | 18(20%) | 12 (13%) | 0.37 |
| 3 | 11 (8%) | 9 (7%) | 8(9%) | 6 (7%) | ||
| Coronary artery narrowed | ||||||
| Left anterior descending | 86 (65%) | 69 (55%) | 53 (58%) | 58 (64%) | ||
| Left circumflex | 16 (12%) | 29 (23%) | 0.16 | 14 (15%) | 12 (13%) | 0.84 |
| Right | 27 (21%) | 26 (21%) | 23 (25%) | 20 (22%) | ||
| Left main | 2 (2%) | 2 (2%) | 1 (1%) | 1 (1%) | ||
| FFR value | 0.86 ± 0.04 | 0.95 ± 0.03 | <0.001 | 0.86±0.03 | 0.95±0.5 | <0.001 |
| Quantitative coronary angiography assessment | ||||||
| Diameter stenosis | 64±15 | 56 ±10 | 0.09 | 62±13 | 59±12 | 0.66 |
| Minimal lumen diameter (mm) | 1.04±0.47 | 1.16±0.30 | 0.12 | 1.04±0.5 | 1.10±0.6 | 0.30 |
| Lesion length (mm) | 10.1±3.7 | 11.0±4.7 | 0.15 | 10.6±6 | 11.2±5 | 0.55 |
| FFR | P value | FFR | P value | |||
|---|---|---|---|---|---|---|
| ≤0.90 (n=131) | >0.90 (n=126) | ≤0.90 (n=91) | >0.90 (n=91) | |||
| Discharge treatment | ||||||
| Aspirin | 108 (88%) | 110 (89%) | 0.68 | 80 (82%) | 80 (82%) | 1.0 |
| Clopidogrel | 60 (48%) | 43 (35%) | 0.06 | 42 (46%) | 37 (41%) | 0.48 |
| Antivitamin K | 8 (6) | 14 (11%) | 0.18 | 7 (8%) | 7 (8%) | 1.0 |
| ACE inhibitor | 61 (49%) | 66 (54%) | 0.44 | 42 (46%) | 42 (46%) | 1.0 |
| Beta-blocker | 95 (77%) | 89 (72%) | 0.38 | 71 (78%) | 61 (74%) | 0.66 |
| Statin at discharge | 120 (96%) | 113 (92%) | 0.19 | 86 (95%) | 87 (96%) | 0.73 |
| Statin dose | ||||||
| No statin | 5 (4%) | 10 (8%) | 0.21 | 5 (5%) | 5 (5%) | 0.93 |
| Medium intensity | 95 (76%) | 83 (67%) | 67 (75%) | 69 (76%) | ||
| High intensity | 25 (20%) | 29 (24%) | 18 (20%) | 19 (15%) | ||
| 10 year outcome | ||||||
| Death | 19 (15%) | 19(16%) | 0.93 | 14 (15%) | 12 (13%) | 0.82 |
| Acute coronary syndrome (all) | 10 (8%) | 7 (6%) | 0.50 | 4 (4%) | 4 (4%) | 1 |
| STEMI | 3 (2%) | 3 (2%) | 0.95 | 2 (2%) | 2 (2%) | 1 |
| NSTEMI | 5 (4%) | 4 (3%) | 0.55 | 2 (2%) | 2 (2%) | 1 |
| Revascularization | 14 (11%) | 13 (10%) | 0.75 | 12 (13%) | 10 (11%) | 0.46 |
| MACE | 43 (33%) | 39 (31%) | 0.78 | 30 (35%) | 26 (29%) | 0.77 |
| Coronary angiography | 54 (41%) | 39 (31%) | 0.12 | 35 (38%) | 31 (34%) | 0.33 |

In the whole population, 332 lesions were assessed by FFR; 143 had FFR between 0.80 and 0.90 (mean 0.84 ± 0.04) and 189 had FFR >0.90 (mean 0.95 ± 0.03). Group comparison at lesion-level showed more multivessel disease and more left anterior descending lesions in the group with FFR >0.90. Treatment and lesion-related events were comparable in the 2 groups ( Tables 3 and 4 ). Comparison of 58 pairs matched on the propensity to have FFR >0.90 yielded similar results. Kaplan-Meier curves for lesion-related event were similar both for univariate analysis and for matched comparison ( Figure 4 ). Multivariate analysis failed to show any association between the initial FFR value and occurrence of lesion-related events.
| FFR | P value | FFR | P value | |||
|---|---|---|---|---|---|---|
| ≤0.90 (n=143) | >0.90 (n=189) | ≤0.90 (n=58) | >0.90 (n=58) | |||
| Age (years) | 62± 11 | 64 ± 11 | 0.08 | 63 ±10 | 63 ±11 | 0.78 |
| Men | 108(76%) | 152(80%) | 0.28 | 47(81%) | 46(80) | 0.81 |
| Hypertension | 62(43%) | 87(46%) | 0.59 | 25(43%) | 28(48) | 0.56 |
| Diabetes mellitus | 42 (29%) | 51 (27%) | 0.66 | 12(21%) | 13(22) | 0.82 |
| Dyslipidemia | 104(72%) | 130(69%) | 0.49 | 42(72%) | 39(67) | 0.54 |
| Left ventricular ejection fraction (%) | 60 ± 11% | 58 ± 12% | 0.06 | 60±10% | 59±11% | 0.78 |
| Indication for angiography | ||||||
| Stable/silent angina pectoris | 121(85%) | 16(86%) | 0.82 | 17(35%) | 20(41) | 0.54 |
| Unstable angina pectoris | 16 (11%) | 15 (8%) | 0.32 | 3(6%) | 2(4) | 0.64 |
| Acute coronary syndrome | 6(4%) | 11(6%) | 0.49 | 1(2%) | 5(10) | 0.09 |
| No. of coronary arteries narrowed | ||||||
| 0 | 57(40%) | 59(33%) | 20 (34%) | 21 (36%) | ||
| 1 | 53(38%) | 54(30%) | 22 (37%) | 23 (40%) | ||
| 2 | 20(15%) | 42(23%) | 0.024 | 13 (8%) | 11 (19%) | 0.97 |
| 3 | 10(7%) | 25(14%) | 3 (5%) | 3 (5%) | ||
| Coronary artery narrowed | ||||||
| Left anterior descending | 76(52%) | 133(70%) | 32(55) | 33(57) | ||
| Left circumflex | 35(24%) | 21(11%) | 0.002 | 11(19) | 11(19) | 0.99 |
| Right coronary artery | 31(21%) | 30(16%) | 14(24) | 13(22) | ||
| Left main stem | 2(2%) | 5(3%) | 1(1) | 1(1) | ||
| Fractional flow reserve value | 0.86 ± 0.04 | 0.95 ± 0.03 | <0.001 | 0.86±0.03 | 0.95±0.5 | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


