Current guidelines recommend that >75% of patients with ST-elevation myocardial infarction (STEMI) receive primary percutaneous coronary intervention (PPCI) within 90 minutes. The goal has been hardly achievable, so we conducted a 2-year before-and-after study to determine the impact of emergency department (ED) tele-electrocardiographic (tele-ECG) triage and interventional cardiologist activation of the infarct team at door-to-balloon time (D2BT) and the proportion of patients undergoing PPCI within 90 minutes since arrival. In total 105 consecutive patients with acute STEMI (mean age 62 ± 13 years, 82% men) were studied, 54 before and 51 after the change in protocol. The 51patients in the tele-ECG group underwent tele-electrocardiography at the ED and electrocardiograms were transmitted to a third-generation mobile telephone of an on-call interventional cardiologist within 10 minutes of ED arrival. The infarct team was activated and PPCI was performed by the interventional cardiologist. Fifty-four patients with acute STEMI who underwent PPCI in the year before implementation of tele-electrocardiography served as control subjects. Median D2BT of the tele-ECG group was 86 minutes, significantly shorter than the median time of 125 minutes of the control group (p <0.0001). The proportion of patients who achieved a D2BT <90 minutes increased from 44% in the control group to 76% in the tele-ECG group (p = 0.0001). In conclusion, implementation of ED tele-ECG triage and interventional cardiologist activation of the infarct team can significantly shorten D2BT and result in a larger proportion of patients achieving guideline recommendations.
Current guidelines recommend that >75% of patients with ST-elevation myocardial infarction (STEMI) receive primary percutaneous coronary intervention (PPCI) within 90 minutes. However, this goal has been difficult to achieve. Simultaneously, telecardiology appears to be 1 of the fastest-growing fields in telemedicine and its applications can be categorized as before, during, and after hospitalization. The main purpose of prehospital 12-lead electrocardiographic (ECG) diagnosis is for early detection of acute STEMI and fast communication of the gathered information to an emergency department (ED) physician or cardiologist before a patient’s arrival to shorten the interval for activating PPCI. However, whether use of an in-hospital tele-ECG system may further improve door-to-balloon time (D2BT) and result in a larger proportion of patients receiving adequate treatment as recommended by current guidelines have not been studied. The aim of the present study was therefore to gauge the impact of implementation of ED tele-ECG triage and interventional cardiologist activation of the infarct team on D2BT and the proportion of patients undergoing PPCI within 90 minutes since arrival at the hospital. The study was approved by our institutional review board and all patients who participated in this study submitted their written consent.
Methods
In total 51consecutive patients with STEMI within 12 hours since onset of chest pain and who had undergone PPCI at the Cheng-Hsin General Hospital from January 2009 through December 2009 were recruited as the tele-ECG group in the present study. Diagnosis of STEMI was based on the presence of prolonged chest pain lasting >30 minutes, unresponsiveness to nitroglycerin, and ECG changes matching ECG criteria of STEMI. ECG criteria of STEMI were ST elevation ≥1 mm in ≥2 contiguous ECG leads. Fifty-four consecutive patients with acute STEMI underwent PPCI from January 2008 through December 2008 before implementation of the tele-ECG protocol, were retrospectively reviewed, and served as the historical control group.
Criteria for exclusion were a diagnosis of STEMI before reaching the ED (e.g., those patients who had been diagnosed in other hospitals first and then transferred to our ED with previous contacts), developing acute STEMI after arrival to the ED, or developing complications or cardiogenic shock and requiring urgent surgical interventions and cardiopulmonary resuscitation with endotracheal intubation, cardiac massage, intra-aortic balloon pump, or extracorporeal membrane oxygenation support.
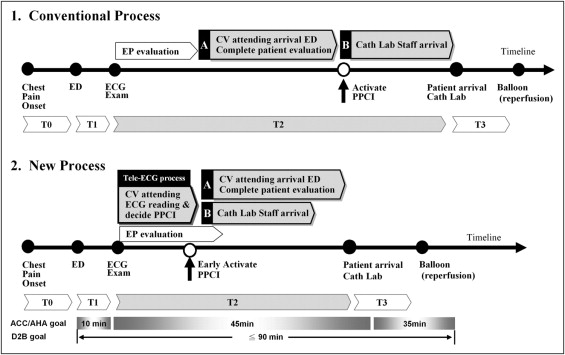
Before implementation of the tele-ECG triage system, a patient was directed to a triage nurse for a brief registration process. Moreover, if a patient mentioned chest pain, the triage nurse assessed the patient instantly and recorded an electrocardiogram. The triage nurse was also responsible for delivering the electrocardiogram to an attending ED physician for interpretation. After confirmation of STEMI by an ED physician, the on-call interventional cardiologist was informed and expected to arrive at the hospital within 30 minutes to evaluate the patient for PPCI. The infarct team was activated next by the interventional cardiologist through a central switchboard operator. All members of the infarct team were due to arrive within 30 minutes after receiving notification of an infarct ( Figure 1 ). After implementation of the tele-ECG triage system, the 12-lead electrocardiogram recorded by the triage nurse was scanned immediately, autoconverted to Joint Photographic Experts Group format, and autotransmitted using a multifunction laser printer (KX-MB788TW, Panasonic, Taiwan, Republic of China) by e-mail to a third-generation mobile telephone of the on-call interventional cardiologist. Resolution of each digital ECG image was preconfigured to an appropriate optimal quality/size ratio to decrease transmission time and prevent image distortion. Thus, each image was compressed to approximately 110 to 170 kB. One minute to 2 minutes was required to transmit each electrocardiogram to a third-generation mobile telephone (CHT 9100, HTC Group, Taiwan, Republic of China). Clinical information and any previous electrocardiogram for comparison, if available, were sent to the cardiologist by the triage nurse as part of the new routine. After confirmation of STEMI by the on-call interventional cardiologist, the infarct team was activated and the on-call interventional cardiologist was required to be at the ED within 30 minutes and evaluate the patient for PPCI; in addition, all members of the infarct team were expected to arrive within 30 minutes ( Figure 1 ).
Shortening the door-to-electrocardiography time to <10 minutes is a sure way to improve D2BT; we therefore tracked down all door-to-electrocardiography times for patients with chest pain complaints during ED registration or triage and D2BTs for all emergency catheterization alerts since the beginning of 2007. Door time was defined as registration time initiated by the triage nurse; balloon time was defined the time a coronary catheter (balloon catheter or thrombectomy device) passed the culprit lesion according to the report of the interventional cardiologist. D2BT was measured as the difference between door and balloon times. The proportion of patients meeting the guideline recommendation of a D2BT ≤90 minutes was calculated based on the number of patients with STEMI meeting the D2BT goal against the total number of patients with STEMI undergoing PPCI in the present study.
D2BT was divided into 4 subintervals: (1) door-to-electrocardiography time, defined as the difference between ECG completion and door time; (2) electrocardiography-to-infarct team activation time, defined as the interval from ECG completion to activation of the infarct team by the on-call interventional cardiologist; (3) infarct team activation-to-catheter laboratory time, defined as the interval from activation of the infarct team and a patient’s arrival at the catheter laboratory; and (4) catheter laboratory-to-balloon time, defined as the interval from a patient’s arrival at the catheter laboratory to balloon time.
Primary outcomes were D2BT and the proportion of patients undergoing PPCI within 90 minutes since arrival; changes of the 4 subintervals before and after implementation of the tele-ECG triage system were considered secondary.
In the present study, all data were retrospectively collected by trained research assistants and taken from our computerized database in a preplanned analysis. We collected data 1 year before and 1 year after implementation of the new tele-ECG process. There was no training phase. Data were then extracted from the database into SPSS 12.0 for Windows (SPSS, Inc., Chicago, Illinois). Continuous variables are expressed as mean ± SD. Intervals are expressed as median (25th to 75th percentiles). Categorical data are presented as percent frequency. Univariant comparisons of demographic parameters and intervals between these 2 groups were made with Student’s t test or Wilcoxon rank-sum test for quantitative data and with the chi-square test or Fisher’s exact test for qualitative data. A p value <0.05 was considered statistically significant.
Results
In total 139 consecutive patients with STEMI within 12 hours since onset of chest pain visited the ED of Cheng-Hsin General Hospital from January 2008 through December 2009. Five of them had been diagnosed with STEMI before ED presentation; 4 had developed acute STEMI since their arrival at the ED; 22 had had mechanical complications, left main coronary artery disease, or severe multivessel disease requiring urgent surgical intervention; and another 3 had cardiogenic shock requiring cardiopulmonary resuscitation including endotracheal intubation, cardiac massage, intra-aortic balloon pump, or extracorporeal membrane oxygenation support in the ED; all were excluded from the study population. Only the remaining 105 patients were recruited, and baseline characteristics of these patients are listed in Table 1 .
| Variable | Tele-ECG Group | Control Group | p Value |
|---|---|---|---|
| (n = 51) | (n = 54) | ||
| Age (years), mean ± SD | 61 ± 13 | 63 ± 13 | 0.618 |
| Men | 43 (84%) | 43 (77%) | 0.334 |
| Diabetes mellitus | 16 (31%) | 23 (41%) | 0.678 |
| Hypertension | 30 (59%) | 31 (58%) | 1.000 |
| Smoking | 14 (27%) | 21 (39%) | 0.206 |
| Hyperlipidemia ⁎ | 21 (41%) | 21 (39%) | 1.000 |
| Previous coronary bypass | 1 (2%) | 3 (6%) | 0.618 |
| Previous percutaneous coronary intervention | 4 (8%) | 6 (12%) | 0.742 |
| Anterior myocardial infarction | 28 (55%) | 38 (70%) | 0.111 |
| Number of diseased coronary arteries | 0.095 | ||
| 1 | 19 (36%) | 16 (22%) | |
| 2 | 16 (32%) | 10 (25%) | |
| 3 | 16 (32%) | 30 (53%) | |
| Medications on admission | |||
| Aspirin | 6 (11%) | 5 (9%) | 1.000 |
| Statins | 8 (16%) | 9 (17%) | 1.000 |
| β Blockers | 10 (20%) | 7 (13%) | 0.523 |
| Calcium channel blockers | 7 (14%) | 9 (17%) | 0.726 |
| Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker | 17 (33%) | 13 (24%) | 0.388 |
| Systolic blood pressure (mm Hg) | 127 ± 30 | 128 ± 29 | 0.888 |
| Diastolic blood pressure (mm Hg) | 74 ± 18 | 77 ± 20 | 0.677 |
| Respiratory rate (breaths/min) | 18 ± 2 | 18 ± 2 | 0.399 |
| Heart rate (beats/min) | 82 ± 18 | 70 ± 19 | 0.189 |
| Temperature (°C) | 36 ± 1 | 36 ± 1 | 0.474 |
⁎ Total cholesterol ≥200 mg/dl, low-density lipoprotein cholesterol ≥130 mg/dl, triglyceride ≥150 mg/dl, or use of lipid-lowering therapy.
Of the 105 patients with acute STEMI, 54 patients were recruited before and the other 51 after the change in protocol; that is, 51patients were in the tele-ECG group and the other 54 in the control group. There were no statistical differences in age, gender, and location of infarction between the 2 groups. Neither group showed significant differences regarding risk factors, previous stroke, previous MI, previous PCI or coronary artery bypass grafting, number of diseased vessels, medications on admission, and vital signs on presentation.
Prehospital on-scene times, defined as time from onset of showing symptoms to arrival at the ED, were similar in the tele-ECG and control groups ( Table 2 ). However, median D2BT of the tele-ECG group was 86 minutes (interquartile range 75 to 95), significantly shorter than the median time of 125 minutes (90 to 127) of the control group (median difference 39, p <0.0001). The proportion of patients who achieved a D2BT <90 minutes increased from 44% of the control group to 76% of the tele-ECG group (p = 0.0001).
| Tele-ECG Group (n = 51) | Control Group (n = 54) | Median Difference | p Value | |
|---|---|---|---|---|
| Prehospital on-scene time (hours) | 2.6 (1–9) | 4.8 (1–8) | −2.2 | 0.191 |
| Door-to-balloon time (minutes) | 86 (75–95) | 125 (90–127) | −39 | <0.0001 |
| Door-to-balloon time <90 minutes (%) | 76 | 44 | 33 | 0.0001 |
| Door-to-electrocardiography time (minutes) | 6 (2–8) | 9 (5–11) | −3 | 0.005 |
| Electrocardiography-to-infarct team activation time (minutes) | 7 (4–12) | 25 (11–45) | −18 | <0.0001 |
| Infarct team activation time to catheter laboratory time (minutes) | 42 (31–50) | 44 (35–60) | −2 | 0.018 |
| Catheter laboratory-to-balloon time (minutes) | 31 (23–38) | 35 (25–50) | −4 | 0.011 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


