Statins decrease postoperative atrial fibrillation (AF) if given before cardiac surgery. However, whether early administration of statins after surgery decreases the risk of postoperative AF is unknown. The association of early reinstitution of postoperative statin therapy within 48 hours to the occurrence of postoperative AF was studied in propensity-adjusted analyses of 200 consecutive patients in sinus rhythm who had undergone coronary artery bypass grafting with or without valve surgery. Postoperative AF occurred in 36 patients (18%). Of 52 patients who received a statin early after surgery, 4 (7.7%) developed AF compared to 32 (28%) of 148 patients who did not (p = 0.043). In the propensity-adjusted analyses, early postoperative statin treatment was associated with a significantly lower occurrence of AF (odds ratio 0.39, 95% confidence interval 0.15 to 0.99), irrespective of concomitant β-blocker therapy. The length of stay was shorter for the patients who received early postoperative statins (median 6.1 days, interquartile range 4 to 7, vs 7.8 days, interquartile range 5 to 8; p = 0.0031). In conclusion, of preoperative statin users undergoing coronary artery bypass grafting with or without valve surgery, early postoperative reinstitution of statins was associated with a lower occurrence of postoperative AF and a shorter length of stay. Early postoperative statin therapy might be a feasible and safe method of reducing postoperative AF.
Atrial fibrillation (AF) after cardiac surgery affects ≤50% of patients and is associated with increased mortality and costs. Recently, observational and randomized studies demonstrated that preoperative statin therapy is associated with a decreased occurrence of postoperative AF. Patients who undergo cardiac surgery, especially coronary artery bypass grafting (CABG), typically have an indication for statins. However, when statins should be started in patients after cardiac surgery remains poorly defined and is, for most, practitioners of secondary importance. We examined whether early postoperative statin therapy is associated with a decreased occurrence of AF after cardiac surgery.
Methods
The eligible study population consisted of 332 consecutive patients who had undergone CABG or valve surgery, or both, from January 2008 to September 2010, at the MetroHealth Medical Center, a large urban safety net hospital in Cleveland, Ohio. We excluded patients who had undergone isolated valve surgery (n = 53), the MAZE procedure (n = 9), vascular surgery (n = 2), or traumatic cardiac repair (n = 9). We also excluded patients who did not receive preoperative statins (n = 49) and the patients who developed AF within 48 hours after surgery in the control group (n = 10) to avoid the immortal time bias of treatment effect. Three patients died after surgery, none of whom had AF. Thus, 200 patients were available for our analyses.
Demographic, cardiac, and noncardiac co-morbidity data and procedural data were obtained from chart review. The institutional review board approved our study, without the requirement for individual written patient consent.
Preoperative medication use was obtained from medication reconciliation documentation at hospital admission or the from preceding outpatient records, if available. For patients who were admitted to the hospital before surgery, the medication administration record was used to assess medication use. Postoperative medication use was documented from the medication administration record for all patients. Early postoperative statin therapy was defined as administration of a statin within 48 hours after surgery and before any development of AF. Patients who were intubated after surgery had orogastric or nasogastric tubes placed for medication administration. No preoperative antiarrhythmic medication was given.
Postoperative AF was defined as any episode of new-onset AF requiring medical treatment with rate-controlling or antiarrhythmic medications or electrical cardioversion after surgery and before hospital discharge. This definition is consistent with that of most previous studies of postoperative AF and the Society of Thoracic Surgeons national cardiac database. AF was detected by continuous telemetry monitoring during the entire hospital stay.
The continuous variables are summarized using the mean ± SD and compared using a 2-tailed Student’s t test or Mann-Whitney U test, if skewed. Categorical variables are summarized using the frequencies and percentages and compared using a chi-square statistic. Odds ratios and 95% confidence intervals are reported for multivariate-adjusted effect sizes and compared the 25th and 75th percentile of values for continuous variables (i.e., age). For variables with a skewed distribution (i.e., length of stay, interval to postoperative statin treatment), the median and interquartile ranges are reported.
To evaluate the association between early postoperative statin therapy and the occurrence of AF, we used a nonparsimonious logistic regression model with 20 variables (see Appendix A on-line ) to calculate the propensity of early postoperative statin therapy as a score from 0 to 1. Nonlinear relations of continuous patient variables with early statin therapy were relaxed using restricted cubic splines (i.e., age, left ventricular mass, left atrial volume). The propensity score was logit-transformed, and the resulting value was used for separate propensity-adjusted logistic regression analysis.
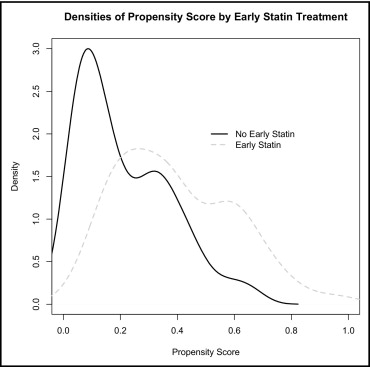
To adjust for confounding variables, we used propensity score-adjusted logistic regression analysis, adjusting for age, concomitant valve surgery, history of hypertension, diabetes, hyperlipidemia, kidney disease (defined as preoperative creatinine level >2 mg/dl), left ventricular ejection fraction, left atrial volume, and preoperative β-blocker use. Owing to the limited number of patients in the present study, we were not able to perform propensity matching, because the propensity score distribution of the 52 patients who received early statin therapy and the 148 patients who did not resulted in only 38 matched patient pairs ( Figure 1 ). In additional analyses, we added the statin type to the propensity-adjusted model to examine whether the results exhibited a drug class effect. The length of stay in patients with and without early postoperative statin treatment was evaluated in the overall sample without adjustment and by multivariate-adjusted linear regression analysis (including all variables in the logistic regression model of postoperative AF).
The study data were collected and managed using REDCap electronic data capture tools hosted at Case Western Reserve University, MetroHealth Campus. SAS, version 9.2 (SAS Institute, Cary, North Carolina) and R, version 2.9.0 (R Foundation of Statistical Computing, available at: http://www.r-project.org ) were used for statistical analyses.
Results
The baseline characteristics of the patients included in our study are listed in Table 1 . Postoperative AF occurred in 36 patients (18%) and was most frequently seen by postoperative days 2 and 3 (51%). Although 194 patients (97%) received a statin after surgery, only 52 (26%) received a statin within the first 48 hours after surgery (i.e., early postoperative statin group). Patients who did not develop AF had received their statin earlier than those who developed AF (median 2.4 days postoperatively, interquartile range 1 to 3, vs median 3.9 days, interquartile range 2 to 5.5, p <0.0068). Of the 52 patients who received postoperative statin within 48 hours after surgery, 4 (7.7%) developed AF compared to 32 (22%) of 148 patients, who did not (p = 0.041). The median length of stay was shorter for the patients who received early postoperative statin therapy (6.1 days, interquartile range 4 to 7) than for the patients who did not (7.8 days, interquartile range 5 to 8, p = 0.003).
| Variable | Early Postoperative Statin | p Value | |
|---|---|---|---|
| No (n = 148) | Yes (n = 52) | ||
| Clinical data | |||
| Age (years) | 59 ± 11 | 58 ± 10 | 0.36 |
| Body mass index (kg/m 2 ) | 31 ± 6.2 | 30 ± 5 | 0.08 |
| Men | 90 (61%) | 33 (64%) | 0.74 |
| Race | |||
| White | 90 (61%) | 43 (83%) | 0.0083 |
| Black | 50 (33%) | 7 (14%) | 0.0061 |
| Chronic obstructive pulmonary disease | 22 (15%) | 5 (9.6%) | 0.34 |
| Diabetes mellitus | 71 (48%) | 22 (42%) | 0.48 |
| Hypertension | 137 (93%) | 63 (89%) | 0.36 |
| Renal disease (creatinine >2 mg/dl) | 8 (5.4%) | 3 (5.8%) | 0.91 |
| Creatinine (mg/dl) | 1.17 ± 0.93 | 1.1 ± 0.87 | 0.48 |
| Hematocrit (g/dl) | 39 ± 4.7 | 39 ± 4.6 | 0.44 |
| Echocardiographic data | |||
| Left ventricular ejection fraction by echocardiography (%) | 53 ± 13 | 56 ± 12 | 0.23 |
| Left ventricular mass (g) | 201 ± 59 | 201 ± 12 | 0.99 |
| Left atrial volume (ml) | 32 ± 25 | 26 ± 25 | 0.19 |
| Left atrial diameter (cm) | 3.4 ± 0.71 | 3.1 ± 0.82 | 0.31 |
| Medication use | |||
| Angiotensin-converting enzyme inhibitor | 99 (67%) | 36 (69%) | 0.76 |
| β Blocker | 139 (94%) | 50 (96%) | 0.54 |
| Calcium channel blockers | 32 (22%) | 15 (29%) | 0.29 |
| Medication withdrawal | |||
| Angiotensin-converting enzyme inhibitor (days) | 2.67 ± 3 | 1.89 ± 1.1 | 0.041 |
| β Blocker (days) | 1.9 ± 2.7 | 1.3 ± 0.59 | 0.022 |
| Surgical | |||
| Isolated coronary artery bypass grafting | 137 (93%) | 50 (96%) | 0.37 |
| Concomitant valve surgery | 11 (7.4%) | 2 (3.8%) | 0.37 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


