Isolated coronary artery ectasia (CAE) may be associated with stable or unstable coronary events despite the absence of epicardial coronary stenosis. Impaired coronary flow dynamics and myocardial perfusion have been demonstrated in stable patients with ectatic coronary arteries. We aimed to assess whether epicardial flow and tissue-level perfusion would be improved by diltiazem in myocardial regions subtended by the ectatic coronary arteries in patients with isolated CAE. A total of 60 patients with isolated CAE were identified of 9,780 patients who underwent elective coronary angiography. Patients were randomized to 5 mg of intracoronary diltiazem or saline. Coronary blood flow of the microvascular network was assessed using myocardial blush grade (MBG) technique. The thrombolysis in myocardial infarction (TIMI) flow grade and TIMI frame count (TFC) were used to assess epicardial coronary flow. MBG (from 2.4 to 2.6, p = 0.02), TIMI flow grades (from 2.4 to 2.8, p <0.001), and TFC (from 35 to 26, p <0.001) were significantly improved after diltiazem, whereas no significant change was noticed after saline (from 2.4 to 2.4, p = 0.86 for MBG; from 2.3 to 2.3, p = 0.71 for TIMI flow grade; and from 35 to 33, p = 0.43 for TFC). Diltiazem provided amelioration of the altered coronary flow dynamics, which was suggested as the pathophysiological influence of CAE. In conclusion, the favorable effects of the diltiazem on myocardial perfusion were observed at both epicardial and tissue levels.
The present study with prospective randomized design was set up to assess whether epicardial flow and tissue-level perfusion would be improved by diltiazem in myocardial regions subtended by the ectatic coronary arteries in patients with isolated coronary artery ectasia (CAE).
Methods
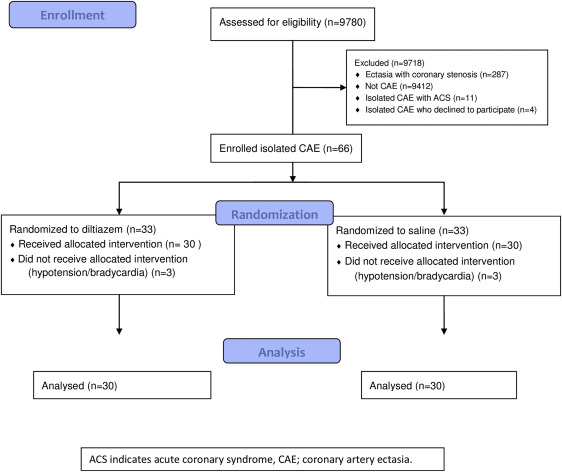
This report complies with Consolidated Standards of Reporting Trials (CONSORT) statement. Nine thousand seven hundred and eighty patients who underwent elective coronary angiography at the Ankara University Department of Cardiology from June 2012 to April 2015 were examined for CAE. The overall incidences of CAE and isolated CAE were 3.8% (368 of 9,780 patients) and 0.83% (81 of 9,780 patients), respectively. The detailed flow diagram of participants is shown in Figure 1 . Stratified block randomization was preferred, in which method age, gender, and ectatic vessel were determined as stratification factors. Randomization was performed by a researcher different from the operator of the coronary angiography. Neither the randomization researcher nor the participant was informed about which group the participant was in until the measurements had completed at the end of the study. Patients were eligible if they had isolated CAE and stable angina pectoris or positive ischemia on stress tests. The primary outcome measure of the study was specified as myocardial blush grade (MBG) which indicated the degree of myocardial microvascular perfusion. The secondary outcome measure was determined as thrombolysis in myocardial infarction (TIMI) flow grade and TIMI frame count (TFC) which demonstrated the level of coronary epicardial flow.
All the patients gave written informed consents. This study complied with the ethical guidelines of the 1975 Declaration of Helsinki, as revised in 2002, was reviewed and approved by the institutional ethics committee on human research and registered at ClinicalTrials.gov (identifier NCT02024919 ). All vasoactive medications were interrupted 24 hours before coronary angiography. Patients with acute coronary syndrome, significant valvular heart disease, heart failure, systolic blood pressure ≤90 mm Hg, heart rate ≥60, atrioventricular block (grade ≥ II), severe liver or kidney failure, significant coronary artery stenosis, and known allergy to diltiazem were excluded.
The indications of coronary angiography were stable angina pectoris and/or positive stress test suggestive of myocardial ischemia. Coronary angiography was performed using the standard technique by means of the Judkins method with 6F diagnostic catheters (Boston Scientific, Boston, Massachusetts) without use of nitroglycerin. Coronary blood flow of the microvascular network was assessed on compact disk films at 30 frames (Siemens Artis Zee, Siemens AG, Medical Solutions, Erlangen, Germany) by 2 observers who were blinded to patients’ clinical data, using the MBG technique, as previously described : grade 0, no myocardial blush; grade 1, minimal blush; grade 2, moderate myocardial blush, but less than that obtained in the same coronary territory of an age- and sex-matched control participant; grade 3, normal myocardial blush. The TIMI flow grade and TFC were assessed for each vessel using criteria defined by Chesebro et al and Gibson et al, respectively. The number of cineframes required for contrast to reach standardized distal coronary landmarks was measured. The distal coronary landmarks used for analysis were the distal bifurcation at the apex of the left anterior descending coronary artery, the distal bifurcation of the major obtuse marginal, or the main circumflex coronary artery, whichever was larger, and the site of origin of first branch at the crux for the right coronary artery. The left anterior descending coronary artery frame counts were corrected by dividing by 1.7 to obtain the corrected TFC as described earlier. Angiographic runs had to be long enough to allow filling of the venous coronary system, and backflow of the contrast agent into the aorta had to be present, to be certain of adequate contrast filling of the epicardial coronary artery. Interobserver and intraobserver variabilities were determined from a random sample of 20 coronary territories scored by reviewers. After allocation of patient, baseline TFC, TIMI flow grade, and MBG were measured. Diltiazem or saline was randomly administered. Five milligram of diltiazem was diluted with 5 ml of saline before administration. Five milliliters of saline was injected as placebo. Continuous blood pressure and heart rate monitoring were performed. Within 3 minutes after drug administration, contrast was reinjected to evaluate TFC, TIMI flow grade, and MBG.
SPSS 20 (SPSS Science, Chicago, Illinois) for Windows was used for statistical analysis. The Shapiro–Wilk test was used to evaluate whether the distribution of continuous variables was normal. All continuous variables were presented as mean ± standard deviation, if they were normally distributed. Categorical variables were described with percentage frequencies. Comparisons of variables between the 2 individual groups were performed using the Student t test (parametric) and Mann–Whitney U test (nonparametric) for continuous variables and the Pearson chi-square test for categorical variables. Comparisons of coronary flow parameters within the same group before and after diltiazem or placebo administration were performed using the paired t test and Wilcoxon test, for parametric and nonparametric variables, respectively. Sample size was calculated with assumed numbers of TFC as 36 ± 8 and 29 ± 7 in patients administered diltiazem and saline, respectively, which is in agreement with our previous pilot study. The total sample size of 50 was necessary for a 2-sided test with 0.90 statistical power and α level of 0.05. We randomized a total of 60 patients to diltiazem and saline groups. The study ended after meeting the required sample size. p <0.05 was considered statistically significant.
Results
A total of 81 (0.83%) patients with isolated CAE were identified of 9,780 patients who underwent elective coronary angiography. Twenty-one of those were excluded before and during the procedure ( Figure 1 ). Therefore, this study included 60 patients who were randomized to diltiazem and saline groups. Most of the patients were men (73%) with a mean age of 58.3 years. Comparisons of different demographic and clinical characteristics are provided in Table 1 . Baseline values for MBG (2.4 ± 0.5 vs 2.4 ± 0.7, p = 0.72), TIMI flow grades (2.4 ± 0.6 vs 2.3 ± 0.7, p = 0.54), and TFC (35 ± 8 vs 35 ± 7, p = 0.84) were similar between diltiazem and saline groups. The values of MBG (2.6 ± 0.3 vs 2.4 ± 0.7, p = 0.01), TIMI flow grades (2.8 ± 0.4 vs 2.3 ± 0.7, p = 0.001), and TFC (26 ± 8 vs 33 ± 8, p = 0.001) were significantly different after drug injection ( Table 2 for intragroup comparisons). Isolated CAE in left circumflex artery was shown in Figure 2 . Changes of TFC in each patient were demonstrated in Figure 3 . The changes in the means of the MBG and TIMI flow grades were schematized in Figure 4 . The data about intraobserver and interobserver reproducibility of the MBG and TIMI flow grade measurements were reported in Table 3 .
| Characteristics | Diltiazem (n=30) | Saline (n=30) | P |
|---|---|---|---|
| Age, (years ± SD) | 57±12 | 59±12 | 0.57 |
| Male sex | 21(70%) | 23(77%) | 0.77 |
| Left ventricular ejection fraction, (% ± SD) | 61±5 | 63±6 | 0.31 |
| Hypertension | 21(70%) | 17(57%) | 0.42 |
| Diabetes mellitus | 7(23%) | 9(30%) | 0.30 |
| Smoker | 11(37%) | 13(43%) | 0.79 |
| Body mass index, (kg/m 2 ± SD) | 27±3 | 26±4 | 0.66 |
| Fasting blood glucose, (mg/dl ± SD) | 110±34 | 114±27 | 0.73 |
| Total cholesterol, (mg/dl ± SD) | 179±47 | 175±51 | 0.74 |
| LDL cholesterol, (mg/dl ± SD) | 101±31 | 99±44 | 0.88 |
| HDL cholesterol, (mg/dl ± SD) | 40±7 | 42±10 | 0.42 |
| Triglyceride, (mg/dl ± SD) | 170±82 | 158±88 | 0.28 |
| Creatinine, (mg/dl ±SD) | 0.94±0.3 | 0.89±0.2 | 0.46 |
| Hemoglobin, (g/dl ± SD) | 14.7±1.7 | 14.1±2.0 | 0.23 |
| Baseline medications | |||
| Beta blockers | 18(60%) | 15(50%) | 0.60 |
| Statins | 26(87%) | 21(70%) | 0.21 |
| ACEi /ARB | 20(67%) | 17(57%) | 0.59 |
| Ectatic coronary artery | |||
| Left Anterior Descending | 9(30%) | 9(30%) | 1 |
| Circumflex | 6(20%) | 5(17%) | 0.89 |
| Right | 15(50%) | 16(53%) | 0.94 |
| Parameter | Diltiazem | Saline | ||||
|---|---|---|---|---|---|---|
| Before injection (n=30) (mean±SD) | After injection (n=30) (mean±SD) | p | Before injection (n=30) (mean±SD) | After injection (n=30) (mean±SD) | p | |
| Heart rate (beats/min) | 76±10 | 68±7 | <0.001 | 76±9 | 74±7 | 0.48 |
| Systolic Blood Pressure (mmHg) | 136±13 | 126±12 | 0.002 | 134±11 | 134±10 | 0.85 |
| Diastolic Blood Pressure (mmHg) | 73±6 | 68±7 | 0.004 | 73±5 | 73±5 | 0.90 |
| Myocardial Blush Grade | 2.4±0.5 | 2.6±0.3 | 0.02 | 2.4±0.7 | 2.4±0.7 | 0.86 |
| Thrombolysis In Myocardial Infarction flow grade | 2.4±0.6 | 2.8±0.4 | <0.001 | 2.3±0.7 | 2.3±0.7 | 0.71 |
| Thrombolysis In Myocardial Infarction Frame Count | 35±8 | 26±8 | <0.001 | 35±7 | 33±8 | 0.43 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


