Retrievable inferior vena cava filters (IVCFs) were designed to provide temporary protection from pulmonary embolism in high-risk situations. However, little is known about their effectiveness, and many remain permanently implanted, leading to potential complications. The aim of this study was to determine patient characteristics, indications for IVCF placement, retrieval rates, complications, and post-IVCF anticoagulation (AC) practices in patients who have received IVCFs. A retrospective review of IVCF use by 3 specialty groups from January 1, 2009, to December 31, 2011, was conducted at a tertiary referral center. Indications for IVCF, procedural success and complications, post-IVCF AC practices, and patient outcomes were assessed. Seven hundred fifty-eight IVCFs were placed. Follow-up was available for 688 patients (90.7%) at a median of 342.0 days (interquartile range 81.5 to 758.0). Indications for IVCF placement included contraindication to AC in the presence of acute venous thromboembolism (n = 287 [41.7%]) and prophylaxis (n = 235 [34.2%]). Insertion-related complications occurred in 28 patients (4.1%). After IVCF placement, adequate AC was initiated in 454 patients (66.0%) <3.0 days (interquartile range 0 to 13.0) after insertion, but the overall retrieval rate was only 252 of 688 (36.6%) within a median of 134.0 days (interquartile range 72.50 to 205.8). Significant IVCF-related complications occurred in 122 patients (17.7%) within 32 days (interquartile range 13.0 to 116.8). The most common complication (72 of 131 [55.0%]) was deep vein thrombosis. In conclusion, in a large, modern cohort of patients receiving retrievable IVCFs for a variety of indications by various specialties, IVCF insertion remains safe. However, many patients have IVCF-related complications, and often, even when IVCFs are retrieved, there is a delay between AC and retrieval. Quality improvement initiatives that facilitate the expeditious retrieval of IVCF are needed.
Venous thromboembolism (VTE) is common, with a reported incidence of 422 in 100,000 in the United States. Left untreated, pulmonary embolism (PE) will occur in as many as 40% of all patients with proximal deep vein thrombosis (DVT). The preferred treatment for VTE is anticoagulation, but it is contraindicated in many patients and fails to prevent propagation and embolization in others. Inferior vena cava (IVC) filters (IVCFs) are often used in these settings. Furthermore, although all published guidelines agree that IVCFs are indicated in patients with acute VTE who cannot receive anticoagulation or in whom adequate anticoagulation has clearly failed to prevent recurrent VTE, some indications, such as prophylactic use in high-risk trauma patients, remain controversial. Despite this therapeutic uncertainty, IVCF use is increasing. The goal of this study was to describe the current use of retrievable IVCFs and to correlate their use with meaningful clinical outcomes and complications.
Methods
We conducted a retrospective cohort study of all subjects who received retrievable IVCFs at a tertiary center from January 2009 to December 2011. Subjects were identified using International Classification of Diseases, Ninth Revision, codes 37192 and 37193. Data sources included patients’ electronic medical records, which reflected inpatient and outpatient care. All analyses are reported for the 688 (of 758) subjects (90.7%) for whom long-term follow-up was available. The data were collected in compliance with published reporting standards. Specific patient characteristics, operator specialty, indications for IVCF placement, retrieval rates, post-IVCF anticoagulation practices, and patient outcomes were reported. Indications for IVCF placement in which there is consensus in published guidelines documents were defined as “consensus” and included VTE with inability to administer anticoagulation or VTE with anticoagulation failure. Insertion- and retrieval-related complications were classified as minor or major as previously described : minor complications required little or no therapy and did not result in permanent sequelae, whereas major complications required in-hospital therapy or resulted in permanent sequelae or death. Indwelling IVCF–related complications were also documented. Of these, a subset of “significant” complications were defined as IVC thrombosis, IVC perforation, IVCF migration, or IVCF embolization as well as recurrent DVT and PE. Adverse clinical outcomes were defined as recurrent VTE, IVC thrombosis, or death. Anticoagulation was defined as “appropriately dosed” if prophylactic-dose anticoagulation was administered to a patient who received an IVCF for VTE prophylaxis or if therapeutic-dose anticoagulation was administered to a patient who received an IVCF because of an inability to receive anticoagulation or anticoagulation failure. Follow-up was terminated when one of the following was reached: IVCF retrieval, patient death, or the last available clinical and imaging follow-up visit. Institutional review board approval was obtained for this study.
Continuous measures were analyzed using 2-sample Student’s t tests or analysis of variance and are presented as mean ± SD or median (interquartile range [IQR]). Categorical traits were analyzed using chi-square tests and are summarized using percentages. The Kaplan-Meier method was used to perform a time-to-event analysis for time to anticoagulation, time to complications, and time to IVCF retrieval, and the curves were evaluated using the log-rank chi-square test. For IVCF retrieval, the multivariate model adjusted for the following variables: age, male gender, cancer, consensus indication, presence of IVCF-related follow-up, significant complication, appropriate anticoagulation, and the service performing the procedure. For IVCF-related complications, a multivariate model adjusted for the following variables: age, male gender, cancer, consensus indication, the service performing the procedure, and presence of anticoagulation at the time of the complication. Two-sided p values <0.05 indicated statistical significance. SPSS version 17.0 for Windows (IBM SPSS, New York, New York) was used for data management and analysis.
Results
In 688 patients who received retrievable IVCFs, the mean age was 59.0 ± 18.1 years, with 57.6% men and 40.4% with concurrent malignancies. IVCFs were inserted most commonly for indications for which there is guideline consensus (62.1%) and for PE prophylaxis (27.6%). Patients’ baseline characteristics are listed in Table 1 . IVCF types were Option (29.4%; Angiotech, Vancouver, British Columbia, Canada), Celect (21.0%; Cook Medical, Bloomington, Illinois), Bard G2/G2X (21.0%; Bard Medical, Covington, Georgia), Eclipse (14%; Bard Medical), Gunther tulip (11.1%; Cook Medical), OptEase (1.7%; Cordis Corporation, Hialeah, Florida), and ALN filter (0.8%; ALN Medical, Lincoln, Nebraska). Median follow-up was 342.0 days (IQR 81.5 to 758.0). During this time, 218 patients (31.7%) died. Dedicated IVCF-related follow-up visits were documented in 227 patients (33.0%).
| Indication (n = 688) | Men (n = 396) | Age (yrs) | Cancer (n = 278) | |
|---|---|---|---|---|
| Active bleeding and PE or DVT ∗ | 172 (25.0%) | 106 (61.6%) | 62.8 ± 16.2 | 66 (38.4%) |
| Surgery and acute thrombosis ∗ | 115 (16.7%) | 64 (55.7%) | 62.4 ± 16.8 | 67 (58.3%) |
| Known VTE and contraindication to AC ∗ | 119 (17.3%) | 66 (55.5%) | 64.4 ± 14.4 | 46 (38.7%) |
| Documented failure of AC ∗ | 21 (3.1%) | 13 (61.9%) | 65.1 ± 15.7 | 11 (52.4%) |
| PE prophylaxis | 190 (27.6%) | 107 (56.3%) | 50.2 ± 20.3 | 59 (31.1%) |
| PE prevention in patients with poor lung reserve | 45 (6.5%) | 26 (57.8%) | 59.0 ± 17.1 | 21 (46.7%) |
| Other | 26 (3.8%) | 14 (53.8%) | 53.8 ± 14.5 | 8 (30.8%) |
After IVCF placement, anticoagulation was started in 498 patients (72.4%), and appropriately dosed anticoagulation was started in 454 patients (66.0%) within 3.0 days (IQR 0 to 13.0) ( Figure 1 ). In the subset of patients in whom anticoagulation was contraindicated at the time of IVCF insertion (in Table 1 , patients with active bleeding and acute VTE, surgery and thrombosis, known VTE, and contraindication to anticoagulation and PE prophylaxis), appropriately dosed anticoagulation was started in 370 of 596 (62.1%) within 5.5 days (IQR 2.0 to 16.0), and in the subset of patients who did not have initial contraindications to anticoagulation, appropriately dosed anticoagulation was started in 84 of 92 (91.3%) within an average of 1.1 ± 8.1 days (median 0, IQR 0 to 0). Among the 498 patients in whom anticoagulation was started, 16 (3.2%) had major bleeding episodes within a median of 28.0 days (IQR 10.3 to 68.3).
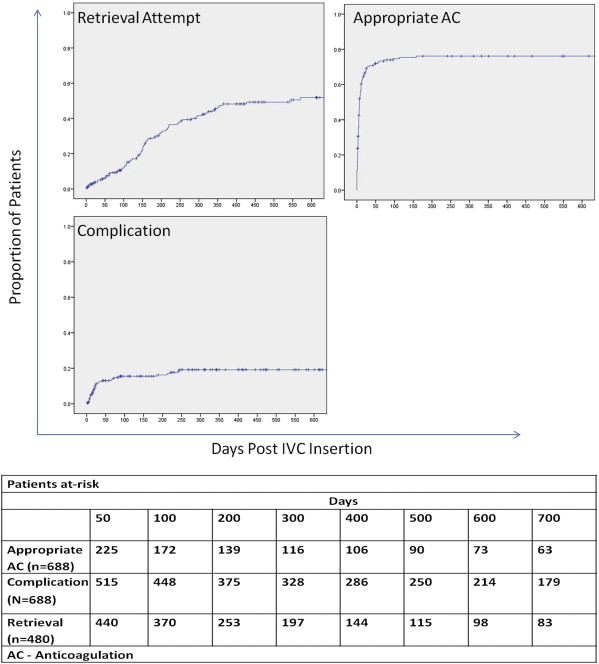
The overall IVCF retrieval attempt rate was 252 of 688 (36.6%) within a median of 134.0 days (IQR 72.50 to 205.8). Excluding patients who died within 90 days, who were lost to follow-up, and who developed permanent indications for IVCFs (as documented by the treating physician), the retrieval attempt rate was 248 of 480 (51.7%), and the actual retrieval rate was 227 of 480 (47.3%) within 134.5 days (IQR 76.0 to 206.8) ( Figure 1 ), while the success rate on the initial retrieval attempt was 218 of 248 (87.9%). Without excluding patients lost to follow-up, the retrieval rate was 227 of 523 (43.4%). The retrieval rate was 65 of 188 (34.6%) by vascular interventional radiology, 45 of 88 (51.1%) by vascular medicine, and 122 of 204 (59.8%) by vascular surgery. The median time to attempted retrieval was 144.0, 133.0, and 86.5 days for patients treated by vascular interventional radiology, vascular medicine, and vascular surgery, respectively. Time to attempted retrieval was longer than time to anticoagulation for every indication, and the median time from resuming anticoagulation to IVCF retrieval (n = 336) was 81.0 days (IQR 0.0 to 161.5).
In the univariate analysis, compared with patients in whom the IVCFs were not retrieved, patients in whom the IVCFs were retrieved were younger (53.6 ± 17.7 vs 59.1 ± 18.4 years, p = 0.001) and had more dedicated follow-up visits to consider IVCF retrieval (71.8% vs 9.9%, p <0.001). There was a trend toward less active malignancy in patients in whom the filters were retrieved (33.5% vs 41.4%, p = 0.072). The factors that were associated with IVCF retrieval in the multivariate model were age (odds ratio [OR] 0.98, 95% confidence interval [CI] 0.96 to 0.99, for every year) and dedicated IVCF follow-up (OR 52.09, 95% CI 26.65 to 101.79). IVC-related complications were not associated with retrieval (p = 0.77) ( Table 2 ).
| Covariate | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age, per yr | 0.98 (0.97–0.99) | 0.001 | 0.98 (0.96–0.99) | 0.004 |
| Male gender | 0.91 (0.63–1.31) | 0.60 | 0.67 (0.39–1.14) | 0.14 |
| Cancer | 0.71 (0.49–1.03) | 0.07 | 0.92 (0.57–1.51) | 0.75 |
| Consensus indication | 1.02 (0.71–1.46) | 0.91 | 1.56 (0.91–2.67) | 1.00 |
| Presence of follow-up | 48.28 (26.36–88.50) | <0.001 | 52.09 (26.65–101.79) | <0.001 |
| Service | ||||
| Vascular interventional radiology | 1.0 | — | 1.0 | |
| Vascular surgery | 3.46 (2.29–5.26) | <0.001 | 1.04 (0.58–1.88) | 0.90 |
| Vascular medicine | 2.61 (1.55–4.38) | <0.001 | 0.96 (0.48–1.93) | 0.92 |
| Significant complication | 1.097 (0.684–1.758) | 0.70 | 1.11 (0.57–2.16) | 0.77 |
| Appropriate anticoagulation | 1.32 (0.83–2.09) | 0.24 | 1.65 (0.93–2.94) | 0.09 |
Insertion-related complications occurred in 28 of the 688 patients (4.1%). Of these, 7 were major complications, including malposition (n = 5) and marked angulation of the IVCF (n = 2).
Indwelling IVCF–related complications occurred in 131 patients (19.0%). Significant indwelling IVCF–related complications occurred in 122 patients (17.7%) within 32 days (IQR 13.0 to 116.8) days ( Figure 1 ), including 72 DVTs (10.5%), 29 PEs (4.2%), and 26 IVC thromboses (3.8%). Less common complications included migration (0.4%), severe tilting (0.3%) and embolization, fracture, infection, and IVC stenosis (0.1% each). In patients in whom IVCFs were inserted for prophylaxis and follow-up was available, IVCF-related complications occurred in 32 of 190 (16.8%) within 21.0 days (IQR 10.0 to 67.0). Of these, 26 (81.3%) were new episodes of DVT. Associations of indwelling IVCF–related complications are listed in Table 3 . In the univariate analysis, compared with patients who did not have complications, patients who did have complications were less likely to be receiving anticoagulation at the time of the complication (44.3% vs 69.5%, p <0.001). In the multivariate model, fewer complications occurred in younger patients (OR 0.99, 95% CI 0.98 to 1.00, for each year) and in the presence of anticoagulation (OR 0.2, 95% CI 0.11 to 0.40, and OR 0.31, 95% CI 0.18 to 0.54, for prophylactic and therapeutic doses, respectively). The frequency of indwelling IVCF–related complications was not associated with the presence of active malignancy (19.0% vs 19.1%, p = 0.989).
| Covariate | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age, per yr | 0.99 (0.98–1.00) | 0.12 | 0.99 (0.98–1.00) | 0.007 |
| Male gender | 1.20 (0.81–1.76) | 0.36 | 1.26 (0.84–1.90) | 0.26 |
| Cancer | 1.00 (0.68–1.48) | 0.99 | 0.83 (0.55–1.25) | 0.37 |
| Indication | ||||
| Active bleeding and PE or DVT ∗ | 1.0 | — | 1.0 | — |
| Surgery and acute thrombosis ∗ | 1.14 (0.62–2.07) | 0.68 | 1.81 (0.91–3.62) | 0.09 |
| VTE (not acute) and contraindication to AC ∗ | 1.47 (0.83–2.59) | 0.19 | 1.43 (0.79–2.60) | 0.23 |
| Documented failure of AC ∗ | 0.76 (0.21–2.73) | 0.67 | 0.98 (0.24–3.96) | 0.97 |
| PE prophylaxis | 1.09 (0.54–1.59) | 0.77 | 0.97 (0.49–1.94) | 0.94 |
| PE prevention in patients with poor lung reserve | 1.14 (0.50–2.60) | 0.76 | 2.06 (0.80–5.32) | 0.13 |
| Other | 0.83 (0.27–2.57) | 0.74 | 1.34 (0.41–4.37) | 0.63 |
| Service | ||||
| Vascular interventional radiology | 1.0 | — | 1.0 | — |
| Vascular surgery | 0.87 (0.57–1.33) | 0.51 | 0.81 (0.50–1.31) | 0.39 |
| Vascular medicine | 0.73 (0.43–1.22) | 0.23 | 0.65 (0.37–1.16) | 0.15 |
| Anticoagulation | ||||
| None | 1.0 | — | 1.0 | — |
| Prophylaxis | 0.27 (0.15–0.46) | <0.001 | 0.2 (0.11–0.40) | <0.001 |
| Therapeutic | 0.41 (0.27–0.63) | <0.001 | 0.31 (0.18–0.54) | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


