Results from randomized trials evaluating thrombus aspiration (TA) in patients with ST-elevation myocardial infarction (STEMI) are conflicting. We assessed 1-year survival in STEMI patients participating in the French Registry of Acute ST-Elevation and non–ST-Elevation Myocardial Infarction (FAST-MI) 2010 according to the use of TA during primary percutaneous coronary intervention (PCI). FAST-MI 2010 is a nationwide French registry that included 4,169 patients with acute myocardial infarction at the end of 2010 in 213 centers. Of those, 2,087 patients had STEMI, of whom 1,538 had primary PCI, with TA used in 671 (44%). Patients with TA were younger (61 ± 13.5 vs 63 ± 14 years), with a similar risk score of the Global Registry of Acute Coronary Events (140 ± 31 vs 143 ± 34) and a shorter median time from symptom onset (245 vs 285 minutes); location of acute myocardial infarction, history of myocardial infarction, PCI, or coronary artery bypass surgery did not differ significantly. Thirty-day mortality was 2.1% versus 2.1% (adjusted p = 0.18), and the rate of 1-year survival was 95.5% versus 94.8%. Using fully adjusted Cox multivariate analysis, hazard ratio for 1-year death was 1.13 (95% confidence interval 0.66 to 1.94). After propensity score matching (480 patients per group), 1-year survival was also similar with both strategies. In a real-world setting of patients admitted with STEMI, the use of TA during primary PCI was not associated with improved 1-year survival.
Primary percutaneous coronary intervention (PCI) is the preferred reperfusion therapy in patients with ST-elevation myocardial infarction (STEMI). When there is an evident thrombus on angiography, thrombus aspiration (TA) is commonly used with the intent to reduce distal embolization and to restore optimal myocardial reperfusion. However, several randomized trials have reported conflicting results, and even meta-analyses cannot agree on whether clinical outcomes with aspiration thrombectomy are improved (higher survival), neutral, or even worsened (increased stroke). Extremely limited data are available from registries that collect data on its real-world utilization. The aim of this study was to assess 1-year outcome in patients participating in the French Registry of Acute ST-elevation or non–ST-Elevation Myocardial Infarction (FAST-MI) 2010 treated with primary PCI for STEMI, according to the use of TA.
Methods
FAST-MI 2010 is a national, prospective multicenter registry including consecutive adult patients hospitalized for acute STEMI and non-STEMI (with symptom onset ≤48 hours) for a period of 1 month (from October 2010), with a possible extension of recruitment up to 1 additional month. Patients with acute myocardial infarction (AMI) after cardiovascular procedures were excluded. Participation in the study was offered to all French institutions with intensive care units in the capacity to receive ACS emergencies. A total of 4,169 patients in 213 centers (76% of active centers in France) were included in this registry, and patients with STEMI were selected for the present study. The registry was conducted in compliance with Good Clinical Practice guidelines, the French data protection law, and approved by the Committee for the Protection of Human Subjects in Biomedical Research of Saint-Louis University Hospital ( Clinicaltrials.gov identifier: NCT01237418 ).
STEMI was diagnosed when ST elevation ≥1 mm was seen in at least 2 contiguous leads in any location on the index or qualifying electrocardiogram or when presumed new left bundle branch block (LBBB) or new Q waves were observed. In this registry, manual TA devices were used as per current practice in the centers and decision of whether to use them depended on operators.
Baseline characteristics were collected prospectively on computerized case record forms by dedicated research technicians sent in each of the centers at least once a week. The degree of coronary flow was classified by Thrombolysis In Myocardial Infarction (TIMI) grade flow as assessed by the investigators. The presence of a “significant amount of thrombus” was reported by the physicians, but it was not precisely quantified. In-hospital complications (recurrent myocardial infarction [MI], stent thrombosis, ventricular fibrillation, atrial fibrillation, bleed, or transfusion) were collected. Stent thrombosis was defined as definite or probable according to the Academic Research Consortium definition. In addition, 30-day and 1-year mortality were also collected. One-year follow-up was 99% complete.
Statistical analysis was performed using SPSS 20.0 software (SPSS Inc., Chicago, IL). For quantitative variables, means and SDs were calculated. Medians with interquartile ranges were calculated when appropriate. Discrete variables are presented as number of events and percentages. Comparisons were made with chi-square or Fisher’s exact tests for discrete variables and by unpaired t tests, Wilcoxon sign-rank tests, or 1-way analyses of variance for continuous variables. Survival curves were estimated using the Kaplan-Meier estimators and compared using log-rank tests. In addition, a propensity score (PS) for getting TA rather than stand-alone primary PCI was calculated using multiple logistic regressions and used to build 2 cohorts of patients (480 patients each) matched on the PS. The variables used were those listed in Table 1 , antithrombotic medications used at the acute stage, and baseline TIMI flow. Correlates of 1-year survival were determined using a multivariate backward stepwise Cox analysis. Cumulative hazard functions were computed to assess proportionality. Three models were used: model 1, adjusted on the risk score of the Global Registry of Acute Coronary Events (GRACE); model 2, adjusted on the PS for getting TA; and model 3, adjusted on the most important preprocedural variables (sex, GRACE score, time from onset to angiography, baseline TIMI score, admission to a community hospital, risk factors, history of heart failure, peripheral artery disease, or stroke, anterior location of MI, LBBB at entry, and use of glycoprotein IIb-IIIa, low–molecular weight heparin, or prasugrel). In addition, to specifically assess the long-term impact of TA, we analyzed 1-year outcomes in patients discharged alive. We also included in-hospital complications and medications prescribed at discharge in the multivariate model. For subgroup analyses, we used the GRACE risk score and the PS for getting TA as covariates. Collinearity was tested by calculation of variance inflation factors. For all analyses, a p value <0.05 was considered significant.
| Variable | Stand-alone pPCI (n=867) | Thrombus aspiration (n=671) | P value |
|---|---|---|---|
| Age (years) | 62.9 ± 14.1 | 61.1 ± 13.5 | 0.01 |
| Women | 223 (26%) | 131 (19.5%) | 0.004 |
| Body mass index (kg/m²) | 26.7 ± 4.5 | 26.9 ± 4.4 | 0.59 |
| Hypertension | 409 (47%) | 277 (41%) | 0.02 |
| Diabetes mellitus | 133 (15%) | 88 (13%) | 0.22 |
| Current smoker | 375 (43%) | 305 (45.5%) | 0.39 |
| Dyslipidemia ∗ | 353 (41%) | 256 (38%) | 0.31 |
| Previous myocardial infarction | 85 (10%) | 64 (9.5%) | 0.09 |
| Previous percutaneous coronary intervention | 78 (9%) | 75 (11%) | 0.16 |
| Previous coronary artery bypass grafting | 41 (5%) | 36 (5%) | 0.57 |
| Previous heart failure | 19 (2%) | 8 (1%) | 0.14 |
| Previous stroke | 19 (2%) | 19 (3%) | 0.42 |
| Peripheral artery disease | 41 (5%) | 26 (4%) | 0.42 |
| Chronic renal failure | 16 (2%) | 10 (1.5%) | 0.59 |
| History of cancer | 68 (8%) | 50 (7.5%) | 0.78 |
| GRACE score | 143 ± 34 | 140 ± 31 | 0.10 |
| Left ventricle ejection fraction | 51 ± 10.9 | 49 ± 10.0 | 0.003 |
| Anterior myocardial infarction | 349 (40%) | 292 (43.5%) | 0.20 |
| Admission Killip class 1 | 733 (86%) | 584 (89%) | 0.24 |
| Aspirin before admission | 129 (15%) | 97 (14.5%) | 0.82 |
| Clopidogrel before admission | 49 (6%) | 40 (6%) | 0.80 |
| Beta-blockers before admission | 163 (19%) | 106 (16%) | 0.12 |
| Statins before admission | 193 (22%) | 125 (19%) | 0.08 |
| Angiotensin-converting enzyme-inhibitors before admission | 106 (12%) | 68 (10%) | 0.20 |
| Diuretics before admission | 158 (18%) | 95 (14%) | 0.03 |
| Calcium channel blockers before admission | 121 (14%) | 84 (12.5%) | 0.41 |
∗ Included patients with previously documented diagnosis of hypercholesterolemia be treated with diet or medication or new diagnosis made during this hospitalization with elevated total cholesterol >160 mg/dl; did not include elevated triglycerides.
Results
Of the 4,169 patients included in the registry, 2,087 had STEMI or LBBB, of whom 1,538 had primary PCI. Forty-four percent of patients were treated with TA ( Table 1 ). Both groups (with or without TA) did not differ in many respects, in particular regarding the GRACE score, location of AMI, history of MI, PCI, or coronary artery bypass grafting, and time from symptom onset to first call. However, patients with TA were younger, less often admitted to general hospitals, time from symptom onset to coronary intervention was shorter, and more often had TIMI flow 0/1 before the procedure, with a greater thrombus burden ( Table 2 ). The rate of radial approach was similar in both groups. The use of drug-eluting stent was higher in patients treated with TA. Finally, fewer patients with TA had TIMI flow 0/1 after the procedure. The use of anticoagulants was generally similar in the 2 groups. Patients with TA received more GP IIb-IIIa and prasugrel. Treatment by statins, β blockers, or ACE (angiotensin-converting enzyme) inhibitors during the first 24 hours was similar in the 2 groups. Finally, the use of TA was associated with lower LVEF and higher peak of cardiac biomarkers (creatine kinase [CK] total: 2,251 ± 2,053 vs 1,588 ± 1,867, p <0.001; troponine Ic: 91 ± 106 vs 62 ± 91, p <0.001; troponine T: 16 ± 55 vs 5 ± 7, p = 0.006).
| Variable | Stand-alone pPCI (n=867) | Thrombus aspiration (n=671) | P value |
|---|---|---|---|
| Time to first call (minutes) | |||
| Median (IQR) | 75 [30;201] | 70 [30;240] | 0.99 |
| No. of patients | [n=849] | [n=643] | |
| Admission to community hospital | 354 (41%) | 206 (31%) | <0.001 |
| Time to primary PCI (minutes) | |||
| Median (IQR) | 285 [180;640] | 245 [165;500] | 0.001 |
| No. of patients | [n=789] | [n=629] | |
| Radial approach | 596 (69%) | 490 (73%) | 0.09 |
| No. of patients | [n=862] | [n=670] | |
| Culprit coronary vessel | 0.008 | ||
| – Left anterior descending | 359 (41%) | 303 (45%) | |
| – Left circumflex | 146 (17%) | 75 (11%) | |
| – Right | 339 (39%) | 285 (42.5%) | |
| – Left main | 9 (1%) | 1 (0.1%) | |
| – Bypass graft | 4 (0.5%) | 5 (1%) | |
| – Undetermined | 10 (1%) | 2 (0.3%) | |
| TIMI flow before | <0.001 | ||
| -0/1 | 449 (59%) | 526 (82%) | |
| -2 | 98 (13%) | 67 (10%) | |
| -3 | 212 (28%) | 50 (8%) | |
| No. of patients | [n=759] | [n=643] | |
| High thrombus burden | 184 (21%) | 494 (73%) | <0.001 |
| No. of patients | [n=864] | [n=668] | |
| DES | 268 (31%) | 149 (22%) | <0.001 |
| BMS | 581 (67%) | 494 (74%) | 0.02 |
| TIMI flow after | <0.001 | ||
| -0/1 | 16 (2%) | 9 (1%) | |
| -2 | 20 (2.5%) | 37 (6%) | |
| -3 | 768 (95.5%) | 608 (93%) | |
| No. of patients | [n=804] | [n=654] | |
| Clopidogrel first | 674 (78%) | 489 (73%) | 0.03 |
| Prasugrel first | 189 (22%) | 181 (27%) | 0.02 |
| Glycoprotein IIb-IIIa inhibitors | 447 (52%) | 446 (66.5%) | <0.001 |
| Fondaparinux before/during angiography | 25 (3%) | 16 (2%) | 0.55 |
| Bivalirudine before/during angiography | 57 (7%) | 45 (7%) | 0.92 |
| LMWH before/during angiography | 377 (43.5%) | 290 (43%) | 0.92 |
| UFH before/during angiography | 504 (58%) | 399 (59.5%) | 0.60 |
| Statins in first 24 hours | 703 (81%) | 539 (80) | 0.71 |
| Beta-blockers in first 24 hours | 535 (62%) | 425 (63%) | 0.51 |
| ACE-inhibitors in first 24 hours | 357 (41%) | 275 (41%) | 0.94 |
In-hospital mortality, nonfatal recurrent MI, stroke, and TIMI major bleeding were not significantly different between both strategies ( Table 3 ). There was a trend in favor of stand-alone PCI regarding stent thrombosis, and ventricular fibrillation was more frequent in patients with TA.
| Variable | Stand-alone pPCI (n=867) | Thrombus aspiration (n=671) | Odds ratio (95% CI) | P Value |
|---|---|---|---|---|
| Death | 18 (2.1%) | 14 (2.1%) | 1.95 (0.73-5.19) | 0.18 |
| Recurrent-MI | 3 (0.3%) | 6 (0.9%) | 1.99 (0.47-8.35) | 0.35 |
| Stroke | 2 (0.2%) | 3 (0.4%) | 2.20 (0.34-14.04) | 0.40 |
| Death, recurrent MI or stroke | 23 (2.7%) | 23 (3.4%) | 1.83 (0.91-3.68) | 0.09 |
| Stent thrombosis | 4 (0.5%) | 8 (1.2%) | 3.45 (0.98-12.11) | 0.053 |
| Ventricular fibrillation | 19 (2.2%) | 30 (4.5%) | 2.52 (1.33-4.79) | 0.005 |
| TIMI major bleeding | 14 (1.6%) | 16 (2.4%) | 1.94 (0.90-4.20) | 0.09 |
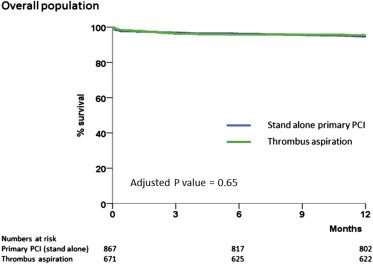
At 1 year, rate of death was similar with both strategies. Using Cox multivariate analysis, the use of TA was not associated with a reduced risk of death (vs stand-alone primary PCI): model 1 (GRACE score adjusted), hazard ratio (HR) 0.98, 95% confidence interval (CI) 0.60 to 1.61; model 2 (PS adjusted), HR 0.96, 95% CI 0.54 to 1.71; and model 3 (fully adjusted), HR 1.13, 95% CI 0.66 to 1.94 ( Figure 1 ). In addition, the use of TA was not associated with a significant reduction in 1-year mortality (HR 0.79; 95% CI 0.30 to 2.09) in patients discharged alive. A subgroup analysis of 1-year mortality (PS adjusted) as a function of TA, according to the age group, sex, time to call, GRACE score at admission, initial TIMI flow, or concomitant use of GP IIb-IIIa inhibitors is presented in Figure 2 . No heterogeneity was observed in any of the subgroup analyses. Finally, we performed additional analyses on patients who had an occluded artery (TIMI 0/1 flow) on the initial angiogram, 1-year mortality was 4.8% in patients with TA and 5.6% in patients without TA (fully adjusted model, HR 1.32, 95% CI 0.69 to 2.53, p = 0.41), and an analysis limited to patients with a high thrombus burden, 1-year mortality was 4.3% for both patients with or without TA (fully adjusted model, HR 1.11, 95% CI 0.33 to 3.68).