Myocardial no-reflow may negate the benefit of urgent coronary revascularization in patients with acute ST-elevation myocardial infarction (STEMI). Among its pathogenetic mechanisms, distal embolization is of prominent importance and several studies have shown that a high coronary thrombotic burden is associated with distal embolization. We aimed at assessing predictors of angiographic thrombus grade in patients undergoing primary percutaneous coronary intervention. Ninety-one patients (62 ± 12 years old, 79% men) presenting for a first STEMI and undergoing urgent coronary angiography within 12 hours from onset of symptoms were consecutively included in the study. Thrombus grade was evaluated by angiography according to the Gibson score and patients were allocated to the high thrombus grade (HTG; score 4 to 5) group or to the low thrombus grade (score 0 to 3) group. Variables predicting angiographic thrombus grade were assessed among clinical, angiographic, procedural, and laboratory data. Sixty-four patients (61 ± 12 years old, 78% men) presented with HTG, whereas 27 patients (63 ± 10 years old, 80% men) presented with low thrombus grade. Patients an HTG showed a significantly higher white blood cell count (12.5 ± 4.8 vs 10.5 ± 2.9, p = 0.015). Aspirin and β-blocker therapy before admission were less frequently taken in the HTG group (5% vs 26% and 7% vs 23%, respectively, p = 0.01 and p = 0.03). At multivariate analysis, lack of previous therapy with aspirin was the only independent predictor of an HTG (odds ratio 6.14, 95% confidence interval 1.09 to 34.67, p = 0.04). In conclusion, previous aspirin therapy is associated with a decrease in angiographic thrombus grade in patients with STEMI treated with primary percutaneous coronary intervention, thus further priming efforts for appropriate use of aspirin in primary prevention of a first STEMI.
Primary percutaneous coronary intervention (PPCI) is first-choice therapy in patients with ST-segment elevation myocardial infarction (STEMI), when performed within 90 minutes from the first medical contact. However, procedural-related distal embolization may hamper the prognostic benefits of reperfusion due to the occurrence of microvascular obstruction, which is in turn associated with a worst prognosis. A high thrombotic grade has been shown to predict distal embolization, thus prompting the development of strategies aimed at decreasing thrombus grade before stent deployment such as thrombus aspiration and use of glycoprotein IIb/IIIa inhibitors. Decrease of thrombus grade may be also achieved before the percutaneous intervention. Of note, previous aspirin therapy in the thrombolytic era was associated with better prognosis. Thus, in this study we aimed at assessing factors associated with angiographic thrombotic grade in a consecutive series of patients presenting with a first STEMI treated by PPCI and the role of previous aspirin therapy in modulating thrombus grade.
Methods
We studied 91 consecutive patients with a first STEMI from September 2007 to September 2008. Inclusion criteria were acute (<12-hour) prolonged chest pain (>30 minutes) and ST elevation >0.2 mV in ≥2 contiguous leads on standard electrocardiogram in patients undergoing PPCI. We excluded patients undergoing “rescue” PCI (n = 25) and those with late presentation (>12 hours, n = 7), previous coronary artery bypass graft surgery (n = 6), saphenous vein graft as the culprit lesion (n = 4), and shock (n = 8). We also excluded 8 patients due to infections, neoplasia, immunologic disease, anti-inflammatory therapy, and recent (<3-month) surgical intervention or traumas. All patients were treated with aspirin (300 mg) and clopidogrel (600 mg) on admission in the emergency room. All PPCIs were performed through a radial or femoral access according to operator preference, using a 6-Fr catheter. A bolus of heparin 5,000 UI was administrated. Glycoprotein IIb/IIIa inhibitors were administrated after diagnostic angiography at the start of PPCI.
Predictors of thrombus grade were evaluated among clinical, angiographic, and laboratory data. Clinical data included age, gender, traditional risk factors, previous ischemic heart disease, preinfarction angina pectoris, morning onset of acute MI, and time to PCI. Arterial hypertension was defined as a systolic blood pressure >140 mm Hg and/or diastolic blood pressure >90 mm Hg in 3 nonconsecutive measurements or current antihypertensive therapy. Patients were defined diabetics when fasting blood glucose was >200 mg/dl in 1 measurement or when a positive blood glucose loading curve was present or in antidiabetic therapy. Smoking habit was considered when referred by the patients; smokers (cigarettes per year 100) were separated from ex-smokers (stopped for ≥3 months). Dyslipidemia was considered when low-density lipoprotein was >130 mg/dl, high-density lipoprotein was <45 mg/dl, triglycerides were >150 mg/dl, or total cholesterol was >200 mg/dl. Pharmacologic therapy at admission was also recorded (angiotensin-converting enzyme inhibitors, β blockers, statins, aspirin), as was ejection fraction (by 2-dimensional echocardiography). Angiographic data included culprit vessel, number of narrowed arteries (diameter stenosis >70%), Rentrop collaterals, and artery size (using diameter of 2.75 mm as a cutoff for categorization).
Laboratory data included complete hemochrome, serum glucose, serum creatinine, lipid profile, and troponin T. C-reactive protein (CRP) was measured by an ultrasensitive nephelometric method (Latex BN-2, Dade-Behring, Marburg, Germany) with a lower detection limit of 0.2 mg/L.
Coronary angiographic analysis was performed by 2 expert angiographers blinded to a patient’s identity and clinical and laboratory features. Thrombus grade was assessed according to Gibson et al. In particular, intracoronary thrombus was angiographically identified and graded. In grade 0 thrombus, there is no angiographic feature of a thrombus; in grade 1 thrombus, there is possible thrombus with angiographic features such as decreased density of contrast, haziness, irregular contours, or a smooth convex meniscus at the site of total occlusion suggestive but not diagnostic of thrombus; in grade 2 thrombus, there is a defined thrombus with greatest dimension equal to 1/2-vessel diameter; in grade 3 thrombus, there is a defined thrombus with greatest dimension >1/2- and <2-vessel diameter; in grade 4 thrombus, there is a defined thrombus with the greatest dimension >2-vessel diameter; in grade 5 thrombus, there is total occlusion. We classified thrombus grade into 2 categories, low thrombus grade (LTG) for thrombus grade ≤3 and high thrombus grade (HTG) for thrombus grades 4 to 5, to identify potential predictors at multivariable analysis. We decided to use this cut-off value according to a recent study that showed that HTG is associated with angiographic and electrocardiographic indexes of no-reflow after PPCI, thus suggesting prognostic implications of this cutoff.
Data distribution was assessed by Kolmogorov-Smirnov test. Because CRP had a non-normal distribution, comparison of CRP serum levels between groups were performed using Mann-Whitney test. Comparison between continuous variables was done by Student’s t test. Comparison between categorical variables was done by Fisher’s test. Variables that at univariable analysis had a p value <0.15 (blood glucose, mean corpuscular volume, white blood cell count, aspirin, and β blockers) were included in a multiple logistic regression model. Data were expressed as mean ± SD for continuous variables or as median ± interquartile range, as appropriate, with percentage for the categorical variable. All analyses were performed using SPSS 15 (SPSS, Inc., Florence, Italy).
Results
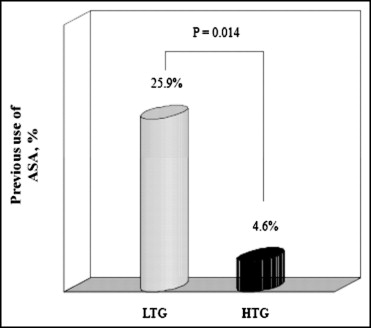
Table 1 lists demographic, clinical, and angiographic features and Table 2 lists laboratory features of the studied population. We enrolled 91 patients (72 men [79%], mean 62 ± 11.8 years old) with 17 diabetics (19%) and 10 (11%) on previous therapy with aspirin (for ≥1 year). Of note, of patients on previous aspirin therapy, 6 had previous stable angina (4 with multiple risk factors [>1] including diabetes) and 4 had previous non-STEMI (2 with previous coronary stenting) in a vessel different from the culprit of current admission. Duration of aspirin therapy was as follows: 6 of 10 patients were taking aspirin for >1 year (4 with stable angina and 2 with non-STEMI, mean 18 months), whereas 4 patients were taking aspirin for >2 years (2 with stable angina and 2 with non-STEMI, mean 29 months). Mean time to PCI was 252 ± 181 minutes (135 to 335). Sixty-four patients (70%) had a HTG, whereas 27 (30%) had an LTG. Hypercholesterolemia tended to be more frequent in the HTG group than in LTG group (31, 48.4%, vs 8, 29.6%, p = 0.10). Moreover, patients with an HTG were less frequently in previous therapy with β blockers (4, 7%, vs 6, 23%, p = 0.03) and aspirin (3, 4.6%, vs 7, 25.9%, p = 0.014; Figure 1 ).
| Variable | Population | LTG | HTG | p Value |
|---|---|---|---|---|
| (n = 91) | (n = 27) | (n = 64) | ||
| Age (years) | 62 ± 12 | 63 ± 10 | 61 ± 12 | 0.627 |
| Men | 72 (79%) | 21 (78%) | 51 (80%) | 0.839 |
| Smoker | 50 (55%) | 16 (59%) | 34 (53%) | 0.593 |
| Hypertension | 54 (59%) | 17 (63%) | 37 (58%) | 0.650 |
| Diabetes mellitus | 17 (19%) | 6 (22%) | 11 (17%) | 0.576 |
| Dyslipidemia | 39 (43%) | 8 (30%) | 31 (48%) | 0.100 |
| Known coronary artery disease | 10 (11%) | 6 (23%) | 4 (6%) | |
| Previous stable angina | 6 (7%) | 4 (15%) | 2 (3%) | 0.342 |
| Previous non–ST-elevation myocardial infarction | 4 (4%) | 2 (8%) | 2 (3%) | |
| Time to percutaneous coronary intervention (minutes) | 252 ± 181.3 (135–335) | 275 ± 178 (121–284) | 239 ± 185 (137–345) | 0.430 |
| Systolic blood pressure (mm Hg) | 129.8 ± 32.65 | 133 ± 31 | 126 ± 32 | 0.347 |
| Diastolic blood pressure (mm Hg) | 77 ± 17.44 | 80 ± 14 | 75 ± 17 | 0.171 |
| Ejection fraction (%) | 45 ± 10 | 48 ± 9 | 44 ± 10 | 0.078 |
| Statins therapy | 10 (11%) | 2 (8%) | 8 (12%) | 0.512 |
| β-blocker therapy | 10 (11%) | 6 (23%) | 4 (7%) | 0.030 |
| Angiotensin-converting enzyme inhibitor therapy | 16 (18%) | 6 (23%) | 10 (17%) | 0.485 |
| Aspirin therapy | 10 (11%) | 7 (26%) | 3 (5%) | 0.014 |
| Disease of left anterior descending coronary artery | 44 (48%) | 14 (52%) | 30 (47%) | |
| Disease of left circumflex coronary artery | 12 (13%) | 3 (11%) | 9 (14%) | 0.743 |
| Disease of right coronary artery | 35 (39%) | 10 (37%) | 25 (39%) | |
| Reference vessel diameter >2.75 mm | 71 (78%) | 19 (70%) | 52 (84%) | 0.147 |
| Number of narrowed coronary arteries | ||||
| 1 | 52 (57%) | 14 (52%) | 38 (61%) | |
| 2 | 23 (25%) | 10 (37%) | 13 (21%) | 0.867 |
| 3 | 14 (15%) | 3 (3%) | 11 (12%) |
| Variable | Data |
|---|---|
| Blood glucose (mg/dl) | 158.9 ± 65.7 |
| Creatinine (mg/dl) | 1.03 ± 0.31 |
| Troponin T (ng/ml) | 2.19 ± 6.64 |
| Fibrinogen (mg/dl) | 334.27 ± 146.9 |
| C-reactive protein (mg/L), median (25–75%) | 10.8 (5.8–16.9) |
| Triglycerides (mg/dl) | 142.6 ± 99.06 |
| Total cholesterol (mg/dl) | 185 ± 45.07 |
| Low-density lipoprotein (mg/dl) | 116.6 ± 39.6 |
| High-density lipoprotein (mg/dl) | 40.2 ± 12.09 |
| Red blood cells (10 12 /L) | 4.73 ± 0.66 |
| Hemoglobin (g/dl) | 14.1 ± 2.08 |
| Hematocrit (%) | 42.5 ± 5.86 |
| Platelet (10 9 /L) | 237.5 ± 74 |
| White blood cells (10 9 /L) | 4.73 ± 0.66 |
Among angiographic data, vessel diameter >2.75 mm tended to be more frequent in the HTG group than in the LTG group (52, 83.9%, vs 19, 70.4%, respectively, p = 0.147).
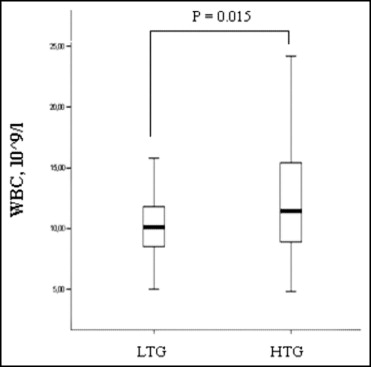
Laboratory data are presented in Table 2 . Hemochrome parameters were similar in the 2 groups, with the exception of white blood cell count, which was significantly higher in the HTG group (12.5 ± 5 vs 10.5 ± 3 × 10 9 /L, p = 0.015; Figure 2 ). Among variables included at multivariable analysis, the only independent predictor of an HTG was the absence of previous aspirin therapy (odds ratio 6.14, 95% confidence interval 1.08 to 34.67, p = 0.04), whereas a high white blood cell count had a borderline statistical significance (odds ratio 1.13, 95% confidence interval 0.99 to 1.29, p = 0.06; Table 3 ).