The REgistry on Cardiac rhythm disORDers assessing the control of Atrial Fibrillation (RecordAF) is the first worldwide, 1-year observational, longitudinal study of the management of paroxysmal/persistent atrial fibrillation (AF) in recently diagnosed patients. The study was conducted at 532 sites in 21 countries across Europe, America, and Asia; recruitment was completed in April 2008. The primary objectives were to prospectively assess the therapeutic success and clinical outcomes in rhythm- and rate-control strategies. The study design and patient baseline data are reported. A total of 5,814 patients with AF were registered, and 5,604 were eligible for evaluation. Rhythm- and rate-control strategies were applied to 55% and 45% of patients, respectively, at study inclusion. Rhythm-control patients mainly received class III agents (45%) or β blockers (51%), except for sotalol, and rate-control patients mainly received β blockers (72%), except for sotalol, or cardiac glycosides (34%). Patients receiving a rhythm-control strategy were younger, had a lower resting heart rate, were more frequently symptomatic, and were more likely to have recently diagnosed AF or paroxysmal AF compared to patients receiving a rate-control strategy. A rate-control strategy was more common in patients with a history of heart failure or valvular heart disease and persistent AF. Rate-control patients more often had previous electrocardiographic evidence of AF and were not in sinus rhythm at inclusion (p <0.01 for both end points). Patients were followed at 6 and 12 months, and changes in therapeutic strategy and clinical outcomes were recorded. In conclusion, the RecordAF study results will provide a global perspective on current AF treatment strategies.
Although improvements have occurred in the primary and secondary prevention of cardiovascular disease, the prevalence of atrial fibrillation (AF) is projected to more than double by 2050 in the United States. The initial AF management strategy according to the guidelines involves either rate or rhythm control. Several antiarrhythmic drugs are effective at reducing the recurrence of AF. However, no difference in mortality has been observed with either rhythm or rate control using current treatment strategies, which are often limited by adverse events. In terms of healthcare costs, the Cost of Care in Atrial Fibrillation survey highlighted that hospitalization represents a large proportion of the cost of treating AF: 52% versus 23% for drug therapy. The Euro Heart Survey provided prospective data on the management of AF in Europe and highlighted a lack of agreement between AF guidelines and clinical practice. A more recent survey has drawn attention to the differences between the internal medicine physicians’ perceptions of treatment strategies for AF and the guidelines. The REgistry on Cardiac rhythm disORDers (RecordAF) study is the first worldwide, prospective, observational study of the real-life management of AF in patients recently diagnosed with AF with 1 year of follow-up.
Methods
RecordAF is an international (Europe, North and South America, and Asia), observational, prospective, 1-year longitudinal cohort study of patients with AF. The study was conducted at 532 sites in 21 countries. Recruitment started in May 2007 and was completed in April 2008. The study was conducted in accordance with the Helsinki principles, guidelines for Good Epidemiological Practice, and local regulations. Physicians were randomly selected from an initial representative and exhaustive global list (≥10 times the total number of physicians required to participate) of office- or hospital-based cardiologists. The physicians were randomly selected in ratios reflecting the office- or hospital-based cardiology practice in each country.
Patients aged ≥18 years who presented with AF or a history of AF (≤1 year from diagnosis, irrespective of whether AF was treated and the rhythm at inclusion), diagnosed by standard electrocardiographic or electrocardiographic Holter monitoring findings, who were eligible for pharmacologic treatment of AF by rhythm- or rate-control agents, were considered for enrollment in the present study. Patients meeting any of the following criteria were not eligible for inclusion: AF resulting from a transient cause; postcardiac surgery AF (<3 months); life expectancy of <1 year owing to a severe disease; unable to understand or sign the written informed consent because of mental disability; unable to comply with follow-up visits; had a pacemaker or an implantable cardioverter defibrillator; scheduled for pulmonary vein isolation, atrioventricular node/His bundle ablation, or pacemaker implantation; participation in an AF clinical trial in the previous 3 months; or pregnant or lactating. Patients scheduled for ablation or who had had devices fitted were not eligible because of the difficulties in interpreting their rhythm/rate-control strategies.
Physicians included eligible patients who met the inclusion criteria regardless of the purpose of the visit to the cardiologist or the hospitalization. A total of 10 to 30 consecutive patients (after quality assessment of the first 20 patients) were enrolled at each site. The patients gave written informed consent to participate in the present study. The primary objectives were to prospectively assess the therapeutic success within 1 year in patients attending clinics or specialized practices and to assess the clinical outcomes in the rhythm- versus rate-control strategies.
The study had 2 primary outcome parameters. The first was assessment of therapeutic success defined for a given patient at 12 ± 3 months of follow-up as follows:
For patients with a rhythm-control strategy chosen at baseline, the presence of sinus rhythm (recorded during the final visit); or for patients with a rate-control strategy at baseline, a resting heart rate in the target range of ≤80 beats/min.
No incidence of clinical outcomes (see following definitions) at the end of the follow-up.
No crossover between rhythm- and rate-control strategies during the whole follow-up duration.
The other co-primary outcome parameter was the assessment of clinical outcomes in rhythm- and rate-control strategies at 12 ± 3 months’ follow-up. The clinical outcomes were defined as cardiovascular death, stroke, transient ischemic attack leading to hospitalization, myocardial infarction, hospitalization or prolongation of hospitalization for arrhythmic or proarrhythmic events, other cardiovascular events, and major complications of an ablative procedure.
The main secondary objectives at 1 year of follow-up were as follows:
To assess the control of AF (presence of sinus rhythm, recorded during the final visit, for patients with a rhythm strategy chosen at baseline or achievement of a ventricular rate target of ≤80 beats/min at rest for patients with a rate strategy chosen at baseline).
To assess treatment effectiveness, defined as follows:
Proportion of patients in sinus rhythm (recorded during the visit) or at the rate-control target (≤80 beats/min at rest)—depending on the baseline strategy, with no symptoms of AF, still taking the baseline medication (antiarrhythmic and/or rate control), with no reports of treatment-related adverse events, clinical outcomes, cardioversion (electric or pharmacologic), or ablation.
To describe the key demographics and treatment modalities of patients with AF treated by cardiologists worldwide.
To collect information on suspected adverse reactions to prescribed treatment for AF.
The data were collected at baseline, 6 ± 2 months, and 12 ± 3 months during the routine follow-up visits. The patients’ quality of life was assessed using the EuroQoL EQ-5D questionnaire at baseline and 12 months. Quality of life was also assessed in a substudy in the United States, United Kingdom, Germany, Spain, Colombia, Mexico, Sweden, and France using the Atrial Fibrillation Severity Scale (AFSS) questionnaire.
The patients were ineligible for the analyses if they did not meet the inclusion or exclusion criteria. Baseline data were described for eligible patients globally and according to the therapeutic strategy selected at the inclusion visit. The descriptive information has been summarized as the mean ± SD and as the number of nonmissing data for quantitative data. The categorical data have been summarized as the number and percentage of the population with nonmissing data. Comparisons between strategies were made using the chi-square test or Fisher’s exact test for qualitative variables and analysis of variance or the Wilcoxon test for quantitative variables. To identify the factors associated with the choice of a rhythm strategy rather than a rate strategy, multivariate stepwise logistic regression analysis was performed, entering in the model the variables with p ≤0.20 in the univariate analysis. The variables remained in the model only if the associated p value was <0.05; a random effect was used for the country. The analyses were performed using Statistical Analysis Systems statistical software, version 9.2 (SAS Institute, Cary, North Carolina). To estimate the success rate of about 50% at 1 year with a precision of 5% for the 95% confidence intervals, a sample size of 384 evaluable patients per geographic unit of interest (region within a country, a country, or a group of countries) was needed. Initially, 11 regions of interest were identified, for a total of about 4,600 evaluable patients needed and 6,100 patients included (with a maximum expected lost-to-follow-up rate of 25%).
Results
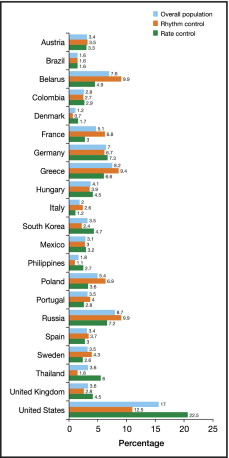
Of the 5,814 patients included in the study, 5,604 (96%) were eligible for evaluation, of whom 3,076 (55%) received a rhythm-control strategy at inclusion and 2,528 (45%) a rate-control strategy. The distribution of eligible patients by country is illustrated in Figure 1 . The greatest number of patients were from the United States (n = 955) and Russia (n = 487).
The demographic data, physical measurements, and vital signs are listed in Table 1 . The patients’ mean age was 66 years. The patients receiving rhythm-control strategies were younger (p <0.001), mainly white (p <0.001), and had a lower heart rate at rest (p <0.001). Most patients had a history of arterial hypertension (68%), and 42% had a history of dyslipidemia. A history of stroke (p = 0.008), heart failure (p <0.001), valvular heart disease (p <0.001), or diabetes (p = 0.006) was significantly more frequent among those receiving rate-control strategies. Among the patients with heart failure in the rate-control group, nonischemic heart disease was the suspected cause in 473 patients (63%; Table 2 ).
| Variable | Rhythm-Control Strategy | Rate-Control Strategy | Total | p Value |
|---|---|---|---|---|
| Age (years) | 64 ± 12.0 (n = 3,076) | 67 ± 11.6 (n = 2,528) | 66 ± 11.9 (n = 5,604) | <0.001 ⁎ |
| Gender | 3,076 | 2,528 | 5,604 | 0.751 † |
| Male | 1,755 (57%) | 1,453 (58%) | 3,208 (57%) | |
| Female | 1,321 (43%) | 1,075 (43%) | 2,396 (43%) | |
| Race | 2,865 | 2,451 | 5,316 | <0.001 † |
| White | 2,578 (90%) | 1,990 (81%) | 4,568 (86%) | |
| Black | 31 (1%) | 57 (2%) | 88 (2%) | |
| Asian | 167 (6%) | 352 (14%) | 519 (10%) | |
| Other | 89 (3%) | 52 (2%) | 141 (3%) | |
| Body mass index (kg/m 2 ) | 28.6 ± 5.3 (n = 3,063) | 28.3 ± 5.7 (n = 2,503) | 28.4 ± 5.5 (n = 5,566) | 0.008 ‡ |
| Seated systolic blood pressure (mm Hg) | 133.5 ± 18.9 (n = 3,075) | 132.3 ± 20.0 (n = 2,525) | 133.0 ± 19.4 (n = 5,600) | |
| Seated diastolic blood pressure (mm Hg) | 79.7 ± 10.9 (n = 3,074) | 79.5 ± 11.5 (n = 2,525) | 79.6 ± 11.1 (n = 5,599) | |
| Heart rate at rest (beats/min) | 76.6 ± 20.9 (n = 3,071) | 80.6 ± 19.1 (n = 2,525) | 78.4 ± 20.2 (n = 5,596) | <0.001 ‡ |
| Variable | Rhythm-Control Strategy | Rate-Control Strategy | Total | p Value |
|---|---|---|---|---|
| Family history of premature cardiovascular disease ⁎ | 573 (21%; n = 2,776) | 438 (20%; n = 2,200) | 1,011 (20%; n = 4,976) | 0.524 † |
| Smoking status ‡ | 3,074 | 2,526 | 5,600 | 0.004 † |
| Never | 1,702 (55%) | 1,318 (52%) | 3,020 (54%) | |
| Current | 412 (13%) | 304 (12%) | 716 (13%) | |
| Former | 849 (28%) | 793 (34%) | 1,642 (30%) | |
| Unknown | 111 (4%) | 111 (4%) | 222 (4%) | |
| History of | ||||
| Coronary artery disease | 509 (18%; n = 2,864) | 452 (19%; n = 2,373) | 961 (18%; n = 5,237) | 0.235 † |
| Myocardial infarction | 240 (8%; n = 3,054) | 233 (9%; n = 2,506) | 473 (9%; n = 5,560) | 0.056 † |
| Stroke | 151 (5%; n = 3,057) | 166 (7%; n = 2,515) | 317 (6%; n = 5,572) | 0.008 † |
| Transient ischemic attack | 100 (3%; n = 3,048) | 105 (4%; n = 2,492) | 205 (4%; n = 5,540) | 0.067 † |
| Peripheral artery disease with ischemic symptoms (claudication) | 83 (3%; n = 3,017) | 81 (3%; n = 2,470) | 164 (3%; n = 5,487) | 0.253 † |
| Carotid stenosis | 56 (2%; n = 2,750) | 72 (3%; n = 2,268) | 128 (3%; n = 5,018) | 0.011 † |
| Arterial hypertension § | 2,096 (68%; n = 3,075) | 1,737 (69%; n = 2,526) | 3,833 (68%; n = 5,601) | 0.629 † |
| Heart failure ¶ | 692 (23%; n = 3,075) | 760 (30%; n = 2,525) | 1452 (26%; n = 5,600) | <0.001 † |
| Suspected cause of heart failure | 688 | 751 | 1,439 | |
| Ischemic | 333 (49%) | 281 (38%) | 614 (43%) | <0.001 ‖ |
| Nonischemic | 357 (52%) | 473 (63%) | 830 (58%) | <0.001 ‖ |
| History of | ||||
| Dyslipidemia # | 1,328 (43%; n = 3,071) | 1,044 (41%; n = 2,519) | 2,372 (42%; n = 5,590) | 0.176 † |
| Valvular heart disease | 472 (16%; n = 3,047) | 594 (24%; n = 2,486) | 1066 (19%; n = 5,533) | <0.001 † |
| Peripheral embolic events | 47 (2%; n = 3,049) | 39 (2%; n = 2,500) | 86 (2%; n = 5,549) | 0.956 † |
| Arrhythmia other than atrial fibrillation | 425 (14%; n = 3,015) | 293 (12%; n = 2,480) | 718 (13%; n = 5,495) | 0.013 † |
| Carotid stenosis | 56 (2%; n = 2,750) | 72 (3%; n = 2,268) | 128 (3%; n = 5,018) | 0.011 † |
| Family history of atrial fibrillation | 304 (10%; n = 3,068) | 212 (8%; n = 2,522) | 516 (9%; n = 5,590) | 0.0534 † |
| Diabetes mellitus | 445 (15%; n = 3,074) | 434 (17%; n = 2,526) | 879 (16%; n = 5,600) | 0.006 † |
| Thyroid disease | 272 (9%; n = 3,022) | 215 (9%; n = 2,461) | 487 (9%; n = 5,483) | 0.732 † |
| Renal disease | 166 (5%; n = 3,054) | 161 (7%; n = 2,487) | 327 (6%; n = 5,541) | 0.103 † |
⁎ If <55 years for males or <65 years for females (mother, father, brother, sister, or children).
‡ Current, patient smoked or had smoked within previous 12 months, ≥1 cigarette/day; former, patient had stopped smoking >12 months before entry into study.
§ Blood pressure >140/90 mm Hg.
¶ New York Heart Association class I, II, III, or IV.
# Low-density lipoprotein >155 mg/dl and high-density lipoprotein <40 mg/dl in men and <48 mg/dl in women.
At baseline, 5% of patients had a first diagnosis of AF. Of those diagnosed in the previous year (before baseline), 52% of patients had paroxysmal AF and 48% had persistent AF. A total of 81% were symptomatic at baseline. The left ventricular ejection fraction was >50% in 78% of patients ( Table 3 ). Significantly more patients receiving rhythm-control strategy had a new diagnosis of AF (p = 0.050), history of lone AF (p <0.001), or symptomatic AF (p <0.001). Paroxysmal AF was the most common diagnosis in the previous year in patients receiving rhythm-control strategies. Patients with electrocardiographic evidence of AF and not in sinus rhythm at baseline were more likely to be receiving a rate-control than a rhythm-control strategy (p <0.001). More patients with a left ventricular ejection fraction of ≤50% received a rate-control strategy, and more patients with a left ventricular ejection fraction of >50% received a rhythm-control strategy (p <0.001). Patients with a first diagnosis of AF at the baseline visit were more likely to receive a rhythm-control therapy. Among those patients with AF diagnosed before the baseline visit (in the previous year), rhythm control was the most commonly used strategy for those with paroxysmal AF, and rate control was the most commonly used strategy for patients with persistent AF ( Figure 2 ).



