CC chemokine receptor 2 (CCR2), expressed on the surface of circulating monocytes, and its ligand monocyte chemoattractant protein–1 (MCP-1; also known as CC-chemokine ligand 2) are present in atherosclerotic plaques and may have important roles in endothelial monocyte recruitment and activation. MLN1202 is a highly specific humanized monoclonal antibody that interacts with CCR2 and inhibits MCP-1 binding. The aim of this randomized, double-blind, placebo-controlled study was to measure reductions in circulating levels of high-sensitivity C-reactive protein, an established biomarker of inflammation associated with coronary artery disease, on MLN1202 treatment in patients at risk for atherosclerotic cardiovascular disease (≥2 risk factors for atherosclerotic cardiovascular disease and circulating high-sensitivity C-reactive protein >3 mg/L). Additionally, patients were genotyped for the 2518 A→G polymorphism in the promoter of the MCP-1 gene to investigate the correlation between this polymorphism and reduced C-reactive protein levels with MLN1202 treatment. Patients who received MLN1202 exhibited significant decreases in high-sensitivity C-reactive protein levels, beginning at 4 weeks and continuing through 12 weeks after dosing. Patients with A/G or G/G genotypes in the MCP-1 promoter had significantly greater reductions in high-sensitivity C-reactive protein levels than patients with the wild-type A/A genotype. In conclusion, MLN1202 treatment was well tolerated in this patient population and resulted in significant reductions in high-sensitivity C-reactive protein levels.
Numerous inflammatory biomarkers have been clinically associated with the development and progression of atherosclerotic cardiovascular disease, and among these, C-reactive protein (CRP) has been prospectively validated. Monocyte chemoattractant protein–1 (MCP-1; also known as CC-chemokine ligand 2) is an emerging inflammatory biomarker of atherosclerotic cardiovascular disease and is a major ligand for CC chemokine receptor 2 (CCR2). CCR2 is found on the surface of monocytes and other immune cells. In vitro studies and animal models of atherosclerosis indicate that recruitment of monocytes via MCP-1 has an important causal role in this disease. MCP-1 blood level at the time of an acute coronary syndrome event was predictive of future events in the Orbofiban in Patients With Unstable Coronary Syndromes–Thrombolysis In Myocardial Infarction 16 (OPUS-TIMI 16) trial. In addition, serial measurement of MCP-1 in the larger Aggrastat to Zocor (A to Z) study of patients with acute coronary syndromes showed significant, independent predictive value of baseline and on-treatment MCP-1 levels that was additive to the prognostic information provided by CRP and other clinical risk indicators. MCP-1 levels are genetically determined, and single-nucleotide polymorphisms (SNPs) of the MCP-1 promoter (synonymously identified as either -2578 A>G or -2518 A>G) have been associated with increased MCP-1 expression and an increased risk for atherosclerotic cardiovascular disease. Thus, along with CRP, MCP-1 may be an attractive therapeutic target in the primary and secondary prevention of atherosclerotic cardiovascular disease. MLN1202 is a human monoclonal antibody directed against CCR2, the receptor for MCP-1, and is in clinical development for the treatment of various inflammatory disorders. This study was designed to test the hypothesis that blockade of CCR2 by MLN1202 would reduce serum CRP levels in patients with risk factors for atherosclerotic cardiovascular disease and to determine if SNPs of the MCP-1 promoter could be predictive of response.
Methods
Men and women aged ≥35 years were eligible for enrollment if they had ≥2 risk factors for atherosclerotic cardiovascular disease, and high-sensitivity CRP levels >3.0 mg/L on >1 occasion within the preceding 12 months, the most recent value being <2 weeks before enrollment. Patients receiving lipid-lowering therapy were required to have been taking stable doses for ≥2 months before enrollment. Patients were excluded if they had histories of stroke, coronary artery disease, or congestive heart failure; neoplasms; or any chronic infection or inflammatory condition.
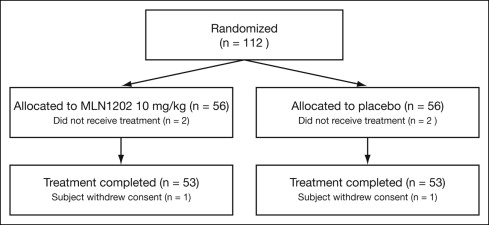
This randomized, double-blind, placebo-controlled study was conducted at 8 study centers from August 16, 2005, to April 5, 2006. Eligible subjects were randomized centrally in a 1:1 ratio to receive MLN1202 10 mg/kg or matching placebo as a single intravenous infusion ( Figure 1 ). Randomization was not stratified by any baseline characteristics. Venipuncture samples for laboratory assessments were obtained at screening, predose, and on days 3, 8, 15, 29, 43, 57, 71, 85, and 113.
CRP, lipid profiles, and standard clinical chemistry and hematology analyses were performed at Covance Central Laboratories (Indianapolis, Indiana). An enzyme-linked immunosorbent assay was used to measure serum MCP-1 levels (MCP-1 Quantikine Kit; R&D Systems, Minneapolis, Minnesota). The upper and lower limits of quantitation were 2,000 and 20 pg/mL, respectively. The inter- and intra-assay variability was <6% and <7%, respectively.
MLN1202 serum concentrations were measured by enzyme-linked immunosorbent assay (developed internally at Millennium Pharmaceuticals, Inc., Cambridge, Massachusetts) at PPD Development (Richmond, Virginia). CCR2 saturation was assessed by indirectly measuring the ability of MLN1202 to inhibit binding and internalization of the fluorescence-labeled functional ligand of CCR2, MCP-1, on CD14 + monocytes and memory CD4 + T cells (CD4 + /CD45RO + ) in a ligand-internalization assay. Deoxyribonucleic acid for SNP genotyping was isolated from whole-blood samples collected at baseline. Deoxyribonucleic acid sample concentration and purity were determined at Covance Central Laboratories. Polymorphisms in the MCP-1 promoter (rs102461 [dbSNP, http://www.ncbi.nlm.nih.gov/SNP ]) corresponding to MCP-1-2518 (also previously called MCP-1-2578) were determined using the TaqMan assay (Applied Biosystems, Inc., Foster City, California) and the following context sequence: GAGCAGAAGTGGGAGGCAGACAGCT[A/G]TCACTTTCCAGAAGACTTTCTTTTC.
The study was conducted in compliance with the Declaration of Helsinki and was consistent with Good Clinical Practice guidelines. The investigational review board at each site approved the study, and all patients gave written informed consent.
The primary efficacy end point was the change in median CRP level from baseline to day 57. The changes in CRP levels in SNP-positive subjects (A/G and G/G combined) were compared with those in SNP-negative subjects (A/A genotype). Secondary efficacy end points included the number of days from baseline until the first 1.0 mg/L decrease in CRP level and changes from baseline to other study visits.
The intent-to-treat population, defined as all randomized subjects who received any study drug (MLN1202 or placebo) and who had baseline and ≥1 postbaseline efficacy assessment, was used for the primary efficacy analyses. For patients who did not have day 57 measurements, the last observation was carried forward in the primary analysis. The pharmacokinetic and pharmacodynamic population was defined as all subjects who received the dose of study drug and for whom pharmacokinetic and pharmacodynamic data for a designated time point were available. The safety population was defined as all subjects who received study drug treatment (MLN1202 or placebo).
Because CRP levels are known to be highly skewed, the primary end point was based on the median change in CRP, and Wilcoxon’s rank-sum test was used for the primary analysis of the primary efficacy end point. Analyses of covariance on log-transformed data were the secondary analyses of the primary end point, adjusting for baseline CRP level as a covariate. All primary and secondary analyses for CRP change were prespecified at the 1-sided significance level of 0.05. An exploratory subgroup analysis was conducted to assess the effect of MCP-1 SNP type on the primary end point.
Between-group comparisons of Kaplan-Meier curves were made using a stratified log-rank test adjusting for baseline CRP as a dichotomous variable (≤5.0 vs >5.0 mg/L). Cox regression modeling was used to adjust for baseline CRP as a continuous variable. It was anticipated that the change in CRP from baseline to day 57 would be approximately 1.0 mg/L for the MLN1202 dose group and that there would be no change in CRP level for the placebo group. To detect the treatment difference with a 1-sided α level of 0.05 and 80% power using Wilcoxon’s rank-sum test, 54 subjects per group would be needed on the basis of simulations. Serum concentration versus time data for the MLN1202 group were subjected to noncompartmental analysis using WinNonlin version 5.0 (Pharsight Corporation, Mountain View, California).
Results
A total of 243 subjects were screened, of whom 112 were randomized to receive study drug. Two subjects in each treatment group were randomized in error and discontinued before receiving the single dose of MLN1202 or placebo. The remaining 108 subjects (54 in each group) constituted the intent-to-treat population for analyses of baseline and efficacy data and the safety population for analyses of safety. Two subjects, 1 in the placebo group and 1 in the MLN1202 group, withdrew consent before completing all study procedures. The remaining 106 subjects, 53 subjects in each treatment group, completed the study. Baseline demographic characteristics of the intent-to-treat population are listed in Table 1 . Most patients in each group were women, with 11% more women in the placebo group than in the MLN1202 group. The percentages of subjects who had histories of hypertension or who were being treated with angiotensin-converting enzyme inhibitors were also greater in the placebo group. The mean age in the placebo group was 4.7 years greater than in the MLN1202 group (p = 0.01, t test), although post hoc analyses of the primary end point did not show any interaction between age and treatment effect. Baseline characteristics were otherwise similar between the 2 treatment groups. In contrast to previous observations, SNP-negative and SNP-positive patients had similar MCP-1 levels at baseline ( Table 1 ).
| Variable | Placebo | MLN1202 |
|---|---|---|
| (n = 54) | (n = 54) | |
| Men | 20 (37%) | 14 (26%) |
| Women | 34 (63%) | 40 (74%) |
| Black | 6 (11%) | 7 (13%) |
| White | 46 (85%) | 46 (85%) |
| Other | 2 (4%) | 1 (2%) |
| Age (years) | 63.3 ± 9.4 | 58.6 ± 10.0 |
| Body mass index (kg/m 2 ) | 32.7 ± 7.1 | 33.9 ± 7.2 |
| High-sensitivity CRP (mg/L) | 6.2 (4.6–8.2) | 5.8 (4.1–10.0) |
| SNP of MCP-1 promoter ⁎ | ||
| Positive (AG or GG) | 29 (53.7%) | 27 (51.9%) |
| Negative (AA) | 25 (46.3%) | 25 (48.1%) |
| Serum MCP-1 level (pg/mL) | ||
| Positive (AG or GG) | 508 ± 157 | 462 ± 142 |
| Negative (AA) | 496 ± 151 | 452 ± 179 |
| Risk factors for atherosclerotic cardiovascular disease | ||
| Age | 48 (89%) | 37 (69%) |
| Body mass index ≥30 kg/m 2 | 32 (59%) | 41 (76%) |
| Current or past smoker (≥20 packs/year) | 14 (26%) | 16 (30%) |
| History of hypertension | 38 (70%) | 26 (48%) |
| History of hypercholesterolemia | 36 (67%) | 40 (74%) |
| Diabetes mellitus | 9 (17%) | 8 (15%) |
| Medication use | ||
| Lipid-lowering therapy | 21 (39%) | 25 (46%) |
| Angiotensin-converting enzyme inhibitors | 15 (28%) | 4 (7%) |
| Angiotensin receptor blockers | 6 (11%) | 4 (7%) |
| Nonsteroidal anti-inflammatory drugs | 21 (39%) | 20 (37%) |
| Aspirin and other antiplatelet agents † | 23 (43%) | 17 (31%) |
| β blockers | 6 (11%) | 8 (15%) |
| Corticosteroids | 1 (2%) | 4 (7%) |
⁎ Excludes 2 subjects with no data.
In the intent-to-treat population, the median change in CRP from baseline to day 57 was 0.2 mg/L in the placebo group, compared with −1.4 mg/L in the MLN1202 group (p = 0.027, Wilcoxon’s rank-sum test; Table 2 ). The difference in the median change in CRP between the MLN1202 and placebo groups was statistically significant (p <0.05) from 4 weeks through 12 weeks postdose ( Figure 2 ). A total of 36 (67%) subjects in the placebo group and 46 (85%) in the MLN1202 group experienced 1.0 mg/L reductions in CRP level. The median time to a 1.0 mg/L decrease in CRP level was 30 days in the placebo group and 16 days in the MLN1202 group (p = 0.018, 1-sided Cox regression model after adjusting for baseline CRP values).
| Variable | Placebo | MLN1202 | p Value ⁎ |
|---|---|---|---|
| (n = 54) | (n = 54) | ||
| Baseline † | |||
| Mean ± SD (mg/L) | 8.2 ± 7.7 | 8.6 ± 7.1 | |
| Median (mg/L) | 6.2 | 5.8 | |
| Day 57 | |||
| Mean ± SD (mg/L) | 7.7 ± 6.0 | 8.5 ± 10.0 | |
| Mean ± SD change (mg/L) | −0.5 ± 5.3 | −0.2 ± 8.2 | |
| Mean percentage change ± SD (mg/L) | 1.5 ± 38.5 | 16.8 ± 159.8 | |
| Median (mg/L) | 6.0 | 5.2 | |
| Median of changes ‡ (mg/L) | 0.2 | −1.4 | 0.027 |
| Median percentage change (%) | 2.5 | −24.2 | 0.009 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


