Cardiovascular risk stratification of asymptomatic patients is based on the assessment of risk factors. Noninvasive imaging of subclinical atherosclerosis may improve cardiovascular risk stratification, especially in patients with co-morbidities. The aim of this study was to investigate the effect of contrast-enhanced ultrasound (CEUS) of the carotid arteries on cardiovascular risk assessment. The study population consisted of 100 consecutive asymptomatic patients with ≥1 clinical risk factor for atherosclerosis. Cardiovascular risk was estimated by calculating the Prospective Cardiovascular Münster Heart Study (PROCAM) risk score. This score was divided into 3 subgroups: low (≤5%), intermediate (6% to 19%), and high (≥20%). Subclinical carotid atherosclerosis was assessed using standard ultrasound for intima-media thickness and plaque screening and CEUS for additional plaque screening. CEUS was performed using SonoVue contrast agent. Patients with subclinical atherosclerosis were considered to be at high cardiovascular risk. McNemar’s test was used to compare PROCAM score to ultrasound findings. The mean PROCAM risk score was 9 ± 10; the PROCAM risk score was low in 72 patients (72%), intermediate in 17 patients (17%), and high in 11 patients (11%). A total of 21 patients (21%) had abnormal carotid intima-media thickness, 77% had plaques on conventional carotid ultrasound, and 88% had plaques on standard carotid ultrasound combined with CEUS. Detection of atherosclerosis led to the reclassification of 79 patients (79%) to high cardiovascular risk (p <0.001). In conclusion, CEUS changes the risk category as estimated by a traditional risk stratification model in most asymptomatic patients. CEUS may thus be an additional method for cardiovascular risk prediction in patient groups with co-morbidities.
Noninvasive imaging may substantially improve cardiovascular risk assessment. The current guidelines recommend the use of ultrasound for the measurement of carotid intima-media thickness (CIMT) to evaluate cardiovascular risk in asymptomatic patients. Recent data indicate that cardiovascular risk assessment by carotid ultrasound may be further refined by carotid plaque screening. Still, the sensitivity and specificity of carotid ultrasound for the assessment of atherosclerotic plaque is suboptimal. Contrast-enhanced ultrasound (CEUS) is an enhanced form of ultrasound imaging that has a favorable safety profile and may reduce the need for riskier and more expensive diagnostic testing. CEUS has been demonstrated to improve carotid plaque assessment, but information on the role of CEUS in cardiovascular risk evaluation is lacking. Therefore, the aim of this study was to investigate the effect of carotid plaque screening using CEUS on the cardiovascular risk stratification of asymptomatic patients. The results were compared to traditional cardiovascular risk assessment, CIMT measurement, and carotid plaque screening using conventional B-mode ultrasound.
Methods
The study protocol was approved by the local ethics committee, and all study participants provided informed consent before the ultrasound examinations. From April 2010 to February 2011, 100 consecutive patients (45 women) from the outpatient clinics of vascular medicine and cardiology at a university medical center were included in this prospective study. Patients were asked to participate in the study if they were asymptomatic, had no known cardiovascular disease, and had increased cardiovascular risk profiles. Inclusion criteria were ≥1 clinical risk factor for atherosclerosis and age ≥18 years. Risk factors were dyslipidemia (such as familial hypercholesterolemia), hypertension, type 2 diabetes mellitus, smoking, and a family history of cardiovascular disease. Dyslipidemia was defined as total serum cholesterol ≥200 mg/dl. Systemic hypertension was defined as blood pressure ≥140/90 mm Hg or treatment with antihypertensive medication. Exclusion criteria were contraindications for the use of ultrasound contrast agent, such as hemodynamic unstable condition, known right-to-left shunts, and known allergy to microbubble contrast agents. A structured clinical interview and physical examination were performed. All patients underwent CIMT measurement and a standard carotid ultrasound examination in conjunction with CEUS.
Patients were risk stratified using the Prospective Cardiovascular Münster Heart Study (PROCAM) cardiovascular risk score. This risk score is based on age, gender, history of diabetes, family history, smoking habit, systolic blood pressure, and lipid profile. The PROCAM score gives an estimation of the global risk for a heart attack or dying from an acute coronary event within the next 10 years. For the PROCAM cardiovascular risk score, patients were stratified as low risk (PROCAM score ≤5%), intermediate risk (PROCAM score 6% to 19%), or high risk (PROCAM score ≥20%).
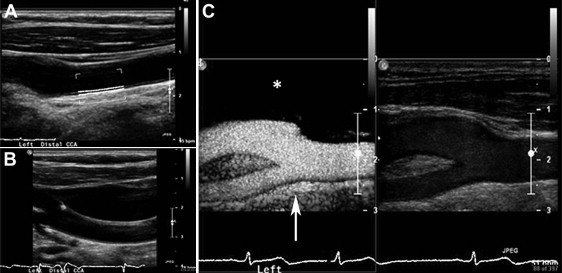
Standard carotid ultrasound, including color Doppler, and CEUS were performed using a Philips iU-22 ultrasound system (Philips Medical Systems, Bothell, Washington), equipped with an L9-3 transducer. Image acquisition was performed by a trained sonography technician using a standard scanning protocol according to the American Society of Echocardiography consensus statement. In short, the left and right carotid arteries were examined with the patient in a supine position with the head supported at a 45° angle turned to the contralateral side. The left and the right common carotid artery, carotid bifurcation, internal carotid artery, external carotid artery, and vertebral arteries were imaged using B-mode ultrasound, color Doppler, and pulse-wave Doppler. All anatomic sites were examined from different angles of view, and each site was scanned in cross-sectional view and longitudinal view. Presets of the ultrasound system were as follows: gain 30%, compression 60, and imaging depth 3.0 cm. These settings were adjusted per patient to obtain optimal ultrasound images. Each side was extensively evaluated for the presence of carotid plaques ( Figure 1 ).
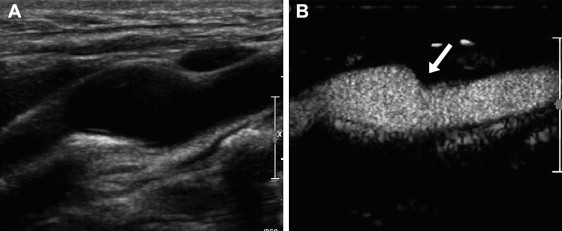
After standard carotid ultrasound, CEUS was performed using intravenous administration of SonoVue contrast agent (Bracco S.p.A., Milan, Italy). The contrast mode of the ultrasound system, using amplitude modulation and a mechanical index of 0.06 to 0.08, was used to optimize the CEUS examination. CEUS clips were recorded with a dual display mode for simultaneous standard B-mode ultrasound and CEUS view. Before injection of the ultrasound contrast agent, the intravenous access was flushed with a 5.0-ml sodium chloride 0.9% solution bolus injection. The ultrasound contrast agent was injected in boluses of 0.5 ml. The 2 carotid arteries were examined using a standard acquisition protocol. Still frames and cine clips were digitally stored for off-line analysis.
Standard ultrasound and CEUS were reviewed off-line by 2 independent observers unaware of the clinical data. For each patient, the same analysis protocol was followed. First, CIMT was measured in the left common carotid artery, followed by screening for the presence of atherosclerotic plaques in the left carotid artery using the standard ultrasound clips. This analysis was repeated for the right carotid artery. Finally, CEUS clips were analyzed; first the left carotid artery was screened for the presence of atherosclerotic plaques. This analysis was repeated for the right carotid artery. In accordance with previously published studies, CIMT was measured in the far wall of the distal 1 cm of the common carotid artery. Semiautomated CIMT measurement was performed using QLAB quantification software (Philips Medical Systems, Best, The Netherlands). For each side, the CIMT measurement was performed 3 times on selected still frames on different R-wave peaks of the electrocardiographic signal. The mean value of 3 measurements from the left and right carotid arteries was used in further statistical analysis. The threshold for a high CIMT value was calculated for each patient individually according to the formula reported by Jäger and Staub (threshold value [mm] = decade of life/10 + 0.2 mm). Patients were considered to have subclinical atherosclerosis if their mean CIMT was higher than this threshold value. Carotid plaque screening was performed using the standard carotid ultrasound images and color Doppler clips. Atherosclerotic plaque was defined as a focal structure encroaching into the lumen of ≥0.5 mm or 50% of the surrounding CIMT or demonstrating a thickness >1.5 mm as measured from the media-adventitia interface to the intima-luminal interface. The presence of plaques was recorded for each side. Subsequently, carotid plaque screening was performed using the CEUS images. In the CEUS images, the carotid lumen is enhanced by the presence of contrast agent, resulting in enhanced visualization of plaque and luminal morphology ( Figure 2 ). The definition of atherosclerotic plaques was identical to that used for standard ultrasound. The presence of plaques was recorded for each side. According to current guidelines, patients with atherosclerotic plaques present in the carotid arteries were considered to be at high risk for future cardiovascular events.
Statistical analysis was performed using PASW for Windows version 17.0.2 (SPSS, Inc., Chicago, Illinois). Continuous data are expressed as mean ± SD. Categorical variables are expressed as counts and percentages and/or median values. Cardiovascular risk stratification with PROCAM score and carotid ultrasound were compared using McNemar’s test.
Results
Characteristics of the study population are listed in Table 1 . Standard carotid ultrasound examinations and CEUS examinations were performed without any complications in all patients. According to the PROCAM score, 72 patients were stratified as being at low risk, 17 at intermediate risk, and 11 patients at high risk for cardiovascular events.
| Characteristic | Value |
|---|---|
| Age (yrs) | 56 ± 9 |
| Women | 45 (45%) |
| Height (cm) | 174 ± 10 |
| Weight (kg) | 83 ± 17 |
| Body mass index (kg/m 2 ) | 27 ± 5 |
| PROCAM risk sore | 5 (2–11) |
| Cardiovascular risk factors | |
| Diabetes mellitus | 22 (22%) |
| Dyslipidemia | 88 (88%) |
| Familial history of cardiovascular diseases | 51 (51%) |
| Hypertension | 33 (33%) |
| Smoking (current) | 24 (24%) |
| Smoking (former) | 23 (23%) |
| Medications | |
| Statin | 91 (91%) |
| β blockers | 18 (18%) |
| Angiotensin-converting enzyme inhibitors | 15 (15%) |
| Angiotensin receptor blockers | 14 (14%) |
| Calcium antagonists | 9 (9%) |
| Diuretics | 14 (14%) |
| Oral antidiabetic agents | 13 (13%) |
| Insulin | 15 (15%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


