Cardiac resynchronization therapy (CRT) is considered a class I indication in treatment of patients with New York Heart Association (NYHA) functional class III and IV heart failure. However, only small numbers of patients in large clinical trials have been in NYHA functional class IV. Therefore, little is known about the effects of CRT in this group. Therefore, we evaluated the effects of CRT in patients with NYHA functional class IV heart failure. Of all patients referred for CRT implantation, 61 patients with symptoms according to NYHA functional class IV were included. All patients were evaluated before implantation and at 6-month follow-up for clinical changes according to the clinical composite score and changes in left ventricular (LV) volumes and function. In addition, survival was evaluated during long-term follow-up. At 6-month follow-up, 9 patients (15%) had died and 2 patients (3%) were admitted for worsening heart failure. The remaining 39 patients (64%) showed improvement according to the clinical composite score. Decreases in LV end-systolic volume (from 167 ± 88 to 147 ± 93 ml, p = 0.009) and LV end-diastolic volume (from 211 ± 100 to 199 ± 113 ml, p = 0.135) were observed, as was a significant increase in LV ejection fraction (from 22 ± 8% to 28 ± 9%, p <0.001). During a mean follow-up of 30 ± 26 months, 36 patients (59%) died, 27 (75%) from worsening heart failure. Respective 1- and 2-year mortality rates were 25% and 38%. In conclusion, CRT decreases LV volumes and improves cardiac function in patients with NYHA functional class IV heart failure. Nevertheless, (heart failure) mortality remains high in these patients.
Heart failure is a growing health care problem in the Western world. It is estimated that approximately 5 million inhabitants in the United States have heart failure and heart failure hospitalizations have increased drastically over the previous 20 years. Cardiac resynchronization therapy (CRT) has emerged as a new treatment option for patients with drug-refractory end-stage heart failure. Several large trials have demonstrated that CRT not only results in improvement in left ventricular (LV) function, heart failure symptoms, and quality of life but also in a decrease in heart failure hospitalizations and mortality in patients with severe symptomatic heart failure. Accordingly, current guidelines consider CRT a class I indication for patients in New York Heart Association (NYHA) functional classes III to IV, with decreased LV ejection fraction (LVEF) ≤35% and a wide QRS complex (≥120 ms). However, only a small percentage of patients enrolled in large multicenter trials consisted of patients with NYHA functional class IV. In brief, of 10,803 patients enrolled in these large trials, only 451 patients (4.2%) were in NYHA functional class IV. Therefore, little is known about the effects of CRT in this group. It remains to be determined whether and to which extent these patients benefit from CRT. The aim of this study was to determine the possible beneficial effects of CRT on LV volumes and function, clinical symptoms, and long-term outcome in patients in NYHA functional class IV.
Methods
Patients were referred for CRT according to current guidelines: advanced symptoms of heart failure (NYHA functional class III or IV), LVEF <35%, sinus rhythm, and a wide QRS complex (>120 ms). Patients with a recent myocardial infarction or revascularization (≤3 months) were excluded. Of all patients referred for CRT implantation, 61 patients who presented with symptoms according to NYHA functional class IV heart failure were included in the present study. Cause of heart failure was considered ischemic in the presence of significant coronary artery disease (≥50% stenosis in ≥1 major coronary artery) and/or a history of myocardial infarction or previous revascularization. Before and 6 months after CRT implantation, extensive clinical and echocardiographic evaluations were performed.
Clinical evaluation consisted of assessment of heart failure symptoms according to the NYHA classification. Assessment of quality of life was performed using the Minnesota Living with Heart Failure Questionnaire (high scores indicating poor quality of life) and, when possible, exercise capacity was measured using the 6-minute walk test.
All patients underwent echocardiography in the left lateral decubitus position before and 6 months after CRT implantation. Imaging was performed using a commercially available echocardiographic system (Vivid 7, General Electric Vingmed Ultrasound, Milwaukee, Wisconsin). Images were obtained using a 3.5-MHz transducer, at a depth of 16 cm in the parasternal (long- and short-axis) and apical (2- and 4-chamber) views. Standard 2-dimensional and color Doppler data, triggered to the QRS complex, were saved in cine-loop format. A minimum of 3 consecutive beats was recorded from each view and images were digitally stored for off-line analysis (EchoPac 108.1.5, General Electric Vingmed Ultrasound). LV end-systolic volume, LV end-diastolic volume, and LVEF were measured from apical 2- and 4-chamber images using the modified biplane Simpson rule. Severity of mitral regurgitation was assessed according to current guidelines.
The LV lead was inserted transvenously through the subclavian route. A coronary sinus venogram was obtained using a balloon catheter. Next, the LV pacing lead was inserted through the coronary sinus with the help of an 8Fr guiding catheter and positioned as far as possible in the venous system, preferably in a (postero-)lateral vein. The right atrial and ventricular leads were positioned conventionally. Nine patients (15%) received a CRT device without defibrillator, whereas 52 patients (85%) received a device with a defibrillator. Devices used were Contak Renewal, Contak TR, or Contak CD (Boston Scientific, Natick, Massachusetts), InSync Marquis, InSync III, or InSync Sentry (Medtronic, Inc., Minneapolis, Minnesota), and Lumax 340 (Biotronik, Berlin, Germany).
For assessing clinical changes after CRT, the heart failure clinical composite score (clinical composite score) was used. Clinical composite score was classified as worse (the patient died or was hospitalized for or associated with worsening heart failure, demonstrated worsening in NYHA functional class at last observation carried forward, had moderate or marked worsening of patient global assessment score at last observation carried forward, or permanently discontinued CRT because of or associated with worsening heart failure), improved (the patient had not worsened as defined earlier and demonstrated improvement in NYHA functional class at last observation carried forward or had moderate or marked improvement in patient global assessment score at last observation carried forward), or unchanged (the patient neither improved nor worsened). Other clinical measurements included change in NYHA functional class, change in distance covered in the 6-minute walk test, and change in quality-of-life score.
Echocardiographic changes after CRT were assessed by comparing LV end-systolic volume, LV end-diastolic volume, and LVEF at 6-month follow-up to baseline measurements.
During long-term follow-up, survival and heart failure hospitalizations were reported. Primary end point was all-cause mortality. Secondary end point was hospitalization for heart failure. Heart failure hospitalization was defined as admission to a hospital for intravenous diuretics and/or inotrope treatment. Outcome data were collected by chart review, device interrogation, and telephone contact.
Continuous data are presented as mean ± SD, and dichotomous data are presented as numbers and percentages. Comparison of data within patients (at baseline and follow-up) was performed using paired-samples t test. Survival was investigated with the Kaplan-Meier method. The effect of different variables on the primary end point was measured by the Cox proportional hazards model. Variables that showed a statistically significant effect in univariate analyses were entered in the multivariate Cox proportional hazards model. All analyses were performed with SPSS 16.0 for Windows (SPSS, Inc., Chicago, Illinois). All statistical tests were 2-sided. A p value <0.05 was considered statistically significant.
Results
Baseline characteristics are presented in Table 1 . Most patients were men (72%) and the underlying cause of heart failure was ischemic cardiomyopathy in 62%. Patients had severely decreased LV function (mean LVEF 21 ± 7%) with extensive LV dilatation (mean LV end-diastolic volume 215 ± 93 ml, mean LV end-systolic volume 171 ± 82 ml). Medication included diuretics in 92%, angiotensin-converting enzyme-inhibitors in 80%, and β blockers in 59%. None of the patients were on inotropic support at time of device implantation. Ten patients (16%) were already admitted for heart failure at time of implantation.
| Age (years) | 68 ± 10 |
| Men | 44 (72%) |
| Ischemic heart failure | 38 (62%) |
| Heart rate at rest | 75 ± 12 |
| Rhythm | |
| Sinus rhythm | 40 (66%) |
| Atrial fibrillation | 16 (26%) |
| Paced | 5 (8%) |
| QRS duration (ms) | 164 ± 26 |
| QRS morphology | |
| Left bundle branch block | 44 (72%) |
| Right bundle branch block | 6 (10%) |
| Ventricular pacing | 11 (18%) |
| Diabetes mellitus | 16 (26%) |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 53 ± 23 |
| 6-Minute walk test (m) | 127 ± 71 |
| Quality-of-life score | 54 ± 15 |
| Left ventricular end-systolic volume (ml) | 171 ± 82 |
| Left ventricular end-diastolic volume (ml) | 215 ± 93 |
| Left ventricular ejection fraction (%) | 21 ± 7 |
| Mitral regurgitation (grade) | 2.0 ± 1.2 |
| Medication | |
| Anticoagulants | 52 (85%) |
| Diuretics | 56 (92%) |
| Angiotensin-converting enzyme inhibitors/angiotensin II blocker | 49 (80%) |
| β blockers | 36 (59%) |
| Spironolactone | 34 (56%) |
| Digoxin | 17 (28%) |
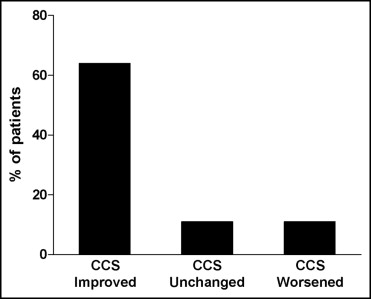
At 6-month follow-up, 9 patients (15%) had died (6 patients died from worsening heart failure, 2 patients died suddenly, and 1 patient died due to a malignancy). Furthermore, 2 patients (3%) were admitted for worsening heart failure. Therefore, these 11 patients (18%) were classified as having worsened according to the clinical composite score. Of the remaining patients, 39 (64%) were classified as improved and 11 (18%) as unchanged ( Figure 1 ). Quality-of-life score decreased from 52.8 ± 13.9 to 38.8 ± 18.8 (p <0.001) and the distance covered in the 6-minute walk test increased from 135 ± 74 to 258 ± 136 m (p <0.001). NYHA functional class decreased from 4.0 ± 0 to 2.7 ± 0.8 (p <0.001).
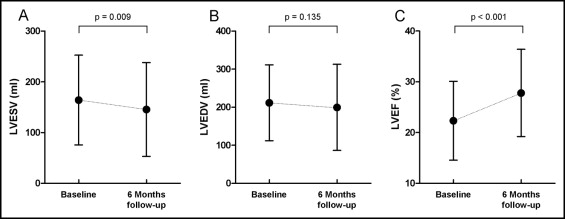
In addition to clinical changes, a significant decrease in LV end-systolic volume was observed at 6-month follow-up (from 167 ± 88 to 147 ± 93 ml, p = 0.009; Figure 2 ). There was a small, but nonsignificant, decrease in LV end-diastolic volume (from 211 ± 100 ml at baseline to 199 ± 113 ml at follow-up, p = 0.135; Figure 2 ). Mean LVEF increased from 22 ± 8% at baseline to 28 ± 9% at follow-up (p <0.001; Figure 2 ). Of note, mean QRS duration at 6-month follow-up was 156 ± 26 ms (p = 0.058 vs baseline).
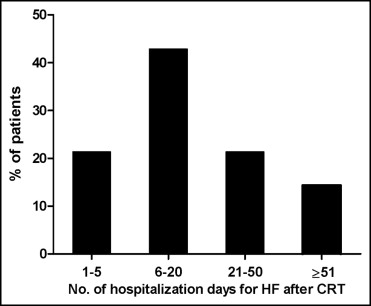
During a mean long-term follow-up of 30 ± 26 months, 14 other patients (23%) were admitted for heart failure. Of note, 7 patients were admitted 1 times, 1 patient was admitted 2 times, 3 patients had 3 admissions for heart failure, 1 patient was admitted 4 times, 1 patient was admitted 5 times, and 1 patient had 8 heart failure hospitalizations.
Mean duration of hospitalization in these patients was 26 ± 29 days ( Figure 3 ). In total, 36 patients (59%) died. Of these 36 patients, 27 (75%) died from worsening heart failure. The survival curve for all-cause mortality is displayed in Figure 4 . Respective 1- and 2-year mortality rates were 25% and 38%.
Univariate and multivariate Cox proportional hazard analyses were performed for all-cause mortality. Variables that proved to be significantly associated with outcome in the univariate Cox proportional hazards model were estimated glomerular filtration rate, 6-minute walk test, quality-of-life score, and extent of mitral regurgitation ( Table 2 ). Higher baseline estimated glomerular filtration rate resulted in superior survival, with a hazard ratio (HR) of 0.97 per milliliter per minute per 1.73-m 2 increase (95% confidence interval [CI] 0.95 to 0.98, p <0.001). More distance covered in the 6-minute walk test was also associated with better survival, with an HR of 0.99 per meter (95% CI 0.99 to 1.00, p <0.001). Higher quality-of-life score was associated with worse survival, with an HR of 1.03 per point (95% CI 1.00 to 1.05, p = 0.043). Greater extent of mitral regurgitation was associated with worse survival, with an HR of 1.51 per grade (95% CI 1.16 to 1.97, p = 0.002). Multivariate Cox proportional hazards model showed that baseline e estimated glomerular filtration rate was the only baseline characteristic that was independently associated with all-cause mortality ( Table 2 ), with an HR of 0.98 (95% CI 0.96 to 0.99, p = 0.013) per increase of 1 ml/min/1.73 m 2 .



