The impact of baseline exercise capacity on clinical outcomes in patients with stable ischemic heart disease randomized to an initial strategy of optimal medical therapy (OMT) with or without percutaneous coronary intervention (PCI) in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial has not been studied. A post hoc analysis was performed in 1,052 patients of COURAGE (PCI + OMT: n = 527, OMT: n = 525) who underwent exercise treadmill testing at baseline. Patients were categorized into 2 exercise capacity groups based on metabolic equivalents (METs) achieved during baseline exercise treadmill testing (<7 METs: n = 464, ≥7 METs: n = 588) and were followed for a median of 4.6 years. The primary composite end point of death or myocardial infarction was similar in the PCI + OMT group and the OMT group for patients with exercise capacity <7 METs (19.1% vs 16.1%, p = 0.31) and ≥7 METs (13.3% vs 10.3%, p = 0.27). After adjusting for baseline covariates, the hazard ratio (99% confidence interval) for the primary end point for the PCI + OMT group versus the OMT group was 1.42 (0.90 to 2.23, p = 0.05) and for the exercise capacity subgroups of ≥7 METs and <7 METs was 0.75 (0.46 to 1.22, p = 0.13). There was no statistically significant interaction between the original treatment arm allocation (PCI + OMT vs OMT) and baseline exercise capacity. In conclusion, there was no difference in the long-term clinical outcomes in patients with exercise capacity <7 METs compared with ≥7 METs, irrespective of whether they were assigned to initial PCI. Patients with exercise capacity <7 METs did not derive a proportionately greater clinical benefit from PCI + OMT compared with those patients who received OMT alone.
In patients with coronary artery disease (CAD), exercise capacity, expressed as metabolic equivalents (METs; 1 MET = 3.5 ml/O 2 /kg/min at rest), is an inverse independent predictor of cardiovascular events, irrespective of age, sex, and race. In the Coronary Artery Surgery Study registry, in patients with 3-vessel CAD, only those who could not achieve >7 METs on a Bruce protocol exhibited better survival with coronary artery bypass surgery than with medical therapy alone, suggesting that exercise testing identified a subgroup of high-risk patients for whom surgery was the superior option. In the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial, there was no difference in the composite end point of death or myocardial infarction in patients with stable ischemic heart disease randomized to optimal medical therapy (OMT) alone or percutaneous coronary intervention (PCI) + OMT. The COURAGE trial provides an opportunity to explore the relation between baseline exercise capacity and long-term clinical outcomes. We therefore evaluated the effect of baseline exercise capacity achieved during exercise treadmill testing in patients of COURAGE trial randomized to PCI + OMT or OMT alone. We hypothesized that, compared to patients with exercise capacity ≥7 METs, those with exercise capacity <7 METs would have a higher rate of cardiac events, and hence, will derive greater benefit from an initial strategy of PCI + OMT than from OMT alone.
Methods
The rationale, design, methods, baseline characteristics, and results of the COURAGE trial (Clinical Trials no. NCT00007657 ) have been described previously. Enrollment required a stenosis of ≥70% in at least 1 major epicardial coronary artery on coronary angiography with objective evidence at baseline of myocardial ischemia or at least 1 coronary stenosis of ≥80% and classic angina in the absence of objective evidence of myocardial ischemia. Patients were excluded if they developed significant ST-segment depression (≥1.5 mm) or hypotension during stage 1 of a Bruce protocol, findings of which would be consistent with a “markedly positive” test for which angiography and revascularization were likely. Because this post hoc analysis sought to assess the relation between exercise capacity and outcomes, patients who were unable to exercise and who underwent pharmacologic stress myocardial perfusion imaging or dobutamine stress echocardiography or qualified for the trial with baseline ischemic ST-segment deviation on the resting electrocardiogram were excluded.
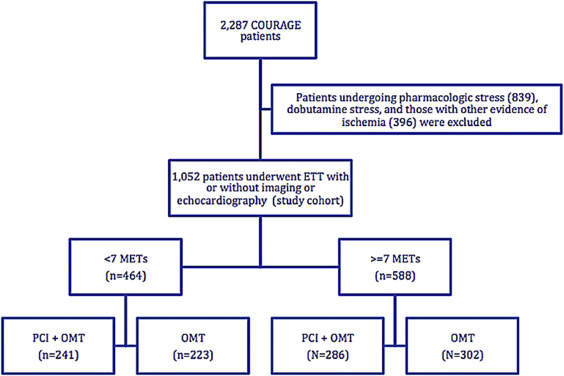
Of the 2,287 trial patients, 1,052 (46%) underwent baseline exercise treadmill testing before randomization, of whom 527 subsequently received PCI + OMT and 525 received OMT alone. Of this subgroup, 452 (43%) underwent standard exercise treadmill test with 12-lead electrocardiogram, 542 (51.5%) underwent exercise myocardial perfusion imaging, and 58 (5.5%) underwent exercise echocardiography. Patients were further categorized into 2 exercise capacity subgroups on the basis of the METs achieved during the exercise treadmill test (either <7 METs or ≥7 METs). The derivation of the study cohort is shown in Figure 1 .The primary outcome measure was a composite of all-cause death or nonfatal myocardial infarction (the COURAGE trial primary endpoint) during a median follow-up of 4.6 years (range 2.5 to 7 years) after randomization.
Exercise stress testing was performed in conformity with American College of Cardiology and American Heart Association guidelines. As per the trial protocol, the decision to perform treadmill exercise stress versus pharmacologic stress testing was at the discretion of the site principal investigators based on the clinical assessment of physical and functional status of patients. The use of nitrates and/or β-adrenergic blocking agents before exercise stress testing was discouraged by trial protocol.
Symptom-limited exercise treadmill testing used the standard Bruce protocol in patients who reported no limitations in their functional capacity at baseline. In patients with limited functional capacity, the modified Bruce, Naughton, or Balke protocols were used. Exercise duration, heart rate, blood pressure, functional capacity, and electrocardiographic response to exercise were recorded. Ischemic ST-segment depression was defined as >1-mm ST-segment deviation from baseline, ≥80 msec after the J-point. Exercise capacity was estimated from exercise workload achieved using a standard formula: ml/kg/min = (mph × 2.68) + (1.8 × 26.82 × mph × grade/100) ÷ 3.5. Exercise capacity was expressed as METs, which was calculated by dividing the estimated peak oxygen consumption (ml/kg/min) by 3.5 ml/kg/min (oxygen consumption at rest).
Continuous variables were presented as a mean ± standard deviation and compared by use of the Student t test. Dichotomous variables were presented as percentages and compared by use of the chi-square test or the Wilcoxon rank-sum test. Cumulative event-free survival curves were calculated by the Kaplan–Meier method, and the primary efficacy of PCI + OMT, compared with OMT alone, was assessed by the stratified log-rank statistic. Because of the post hoc nature of this analysis, a more rigorous estimate of the treatment effect was used, with a 99% confidence interval (CI) instead of a 95% CI surrounding the hazard ratio (HR) for the Cox proportional hazards model, with a p value for significance at <0.01. The effects in the Cox regressions were also adjusted for age, sex, body mass index, family history of CAD, angina, systolic blood pressure, and diastolic blood pressure. All statistical analyses were performed using SAS 9.3.
Results
Baseline characteristics according to METs achieved are summarized in Table 1 . In comparison to patients with exercise capacity ≥7 METS, those with <7 METs were older, more often women, less likely to have a family history of CAD, and had a significantly greater resting systolic and lower diastolic blood pressure. They were also more likely to have Canadian Cardiovascular Class II or III angina and more likely to have received calcium channel blockers. In patients with either ≥7 METs or <7 METs, there were no other statistically significant differences in the baseline characteristics and angiographic data between the treatment groups (PCI + OMT vs OMT alone; Table 1 ).
| Variable | Exercise Work Load (N=1,052) | P value between MET categories | ||||||
|---|---|---|---|---|---|---|---|---|
| <7 METs (N=464) | P value | ≥7 METs (N=588) | P value | |||||
| PCI+OMT (N=241) | OMT (N=223) | PCI+OMT (N=286) | OMT (N=302) | |||||
| Age (years) mean ± SD | 64 ± 9 | 65 ± 9 | 0.30 | 59 ± 9 | 58 ± 9 | 0.23 | <0.001 ∗ | |
| Men | 187 (78%) | 173 (78%) | 1.00 | 258 (90%) | 281 (93%) | 0.21 | <0.001 ∗ | |
| White | 209 (87%) | 196 (88%) | 0.78 | 262 (92%) | 256 (86%) | 0.03 | 0.67 | |
| BMI mean ± SD (kg/m 2 ) | 30 ± 5 | 29 ± 5 | 0.13 | 29 ± 4 | 29 ± 5 | 0.75 | 0.11 | |
| Never smoked | 48 (20%) | 52 (23%) | 0.37 | 54 (19%) | 74 (25%) | 0.10 | 0.93 | |
| Hypertension | 152 (63%) | 136 (62%) | 0.74 | 164 (59%) | 172 (58%) | 0.84 | 0.14 | |
| Diabetes mellitus | 72 (30%) | 60 (27%) | 0.50 | 66 (23%) | 85 (29%) | 0.15 | 0.34 | |
| Family history of CAD | 106 (48%) | 88 (44%) | 0.36 | 153 (58%) | 157 (56%) | 0.65 | <0.001 ∗ | |
| Myocardial infarction | 68 (29%) | 76 (35%) | 0.17 | 97 (34%) | 96 (32%) | 0.64 | 0.54 | |
| CABG | 17 (7%) | 21 (9%) | 0.35 | 27 (9%) | 19 (6%) | 0.16 | 0.83 | |
| PCI | 35 (15%) | 19 (9%) | 0.04 | 40 (14%) | 44 (15%) | 0.85 | 0.21 | |
| Angina pectoris | 217 (90%) | 200 (90%) | 0.79 | 241 (85%) | 256 (85%) | 0.94 | 0.01 ∗ | |
| CCS Angina Class | 0 | 23 (10%) | 23 (10%) | 0.46 | 44(15%) | 46 (15%) | 0.12 | <0.001 ∗ |
| 1 | 57 (24%) | 58 (26%) | 89 (31%) | 104 (34%) | ||||
| 2 | 94 (39%) | 95(43%) | 106(37%) | 123 (41%) | ||||
| 3 | 66 (28%) | 47 (21%) | 46 (16%) | 29 (10%) | ||||
| PAD | 17 (7%) | 10 (5%) | 0.25 | 9 (3%) | 13 (4%) | 0.46 | 0.11 | |
| Heart failure | 6 (3%) | 6 (3%) | 0.88 | 14 (5%) | 7 (2%) | 0.09 | 0.36 | |
| Stroke/TIA | 15 (6%) | 15 (7%) | 0.84 | 13 (5%) | 20 (7%) | 0.28 | 0.55 | |
| Renal disease | 5 (2%) | 0 | 0.03 | 6 (2%) | 7 (2%) | 0.86 | 0.16 | |
| Heart rate (bpm) mean ± SD | 64 ± 10 | 66 ± 13 | 0.08 | 64 ± 11 | 65 ± 11 | 0.39 | 0.64 | |
| SBP (mm Hg) mean ± SD | 135 ± 21 | 134 ± 18 | 0.71 | 131 ± 18 | 130 ± 18 | 0.50 | 0.002 ∗ | |
| DBP (mm Hg) mean ± SD | 64 ± 11 | 73 ± 11 | 0.83 | 76 ± 11 | 76 ± 11 | 0.99 | <0.001 ∗ | |
| Number of arteries narrowed | 1 | 80 (33%) | 65 (29%) | 0.28 | 105 (37%) | 99 (33) | 0.61 | 0.49 |
| 2 | 100 (41%) | 87 (39%) | 105 (37%) | 118 (39%) | ||||
| 3 | 61 (25%) | 71 (32%) | 76 (27%) | 85 (28%) | ||||
| Ejection Fraction | 63 ± 11% | 63 ± 10% | 0.55 | 63 ± 11% | 62 ± 9% | 0.54 | 0.28 | |
| Medications (n) | 206 | 183 | 233 | 247 | ||||
| Aspirin | 185 (90%) | 167 (91%) | 0.63 | 202 (87%) | 216 (87%) | 0.81 | 0.12 | |
| ACEi/ARB | 101 (49%) | 89 (49%) | 0.98 | 115 (49%) | 123 (50%) | 0.85 | 0.89 | |
| Beta-blocker | 155 (75%) | 129 (71%) | 0.33 | 165(70%) | 176 (71%) | 0.80 | 0.44 | |
| Calcium channel blocker | 72 (35%) | 60 (33%) | 0.68 | 59 (25%) | 61 (25%) | 0.92 | 0.003 ∗ | |
Table 2 provides the baseline exercise treadmill test characteristics of the study cohort. In patients with either <7 METs or ≥7 METs, there was no significant difference in the mean exercise duration and ischemic ST-segment depression between the PCI + OMT group and the OMT group. In patients who achieved ≥7 METs, the mean METs achieved was statistically greater in the patients randomized to PCI + OMT compared with OMT alone.
| Variable | Exercise Work Load (N=1,052) | ||||||
|---|---|---|---|---|---|---|---|
| <7 METs (N=464) | ≥7 METs (N=588) | ||||||
| PCI+OMT (N=241) | OMT (N=223) | P value | PCI+OMT (N=286) | OMT (N=302) | P value | ||
| Exercise Protocol | Bruce | 145 (60%) | 138 (62%) | 285 (99.7%) | 298 (99%) | ||
| Modified Bruce | 61(25%) | 55 (25%) | 0 | 4 (1%) | |||
| Naughton | 9 (4%) | 9 (4%) | 0 | 0 | |||
| Balke/Other | 26 (11%) | 21 (9%) | 1 (0.3%) | 0 | |||
| Exercise Duration | <5 minutes | 123 (51%) | 110 (49%) | 0 | 0 | ||
| 5-7 minutes | 77 (32%) | 77 (35%) | 71 (25%) | 97 (32%) | |||
| 7-9 minutes | 21 (9%) | 19 (9%) | 137 (48%) | 138 (46%) | |||
| >9 minutes | 20 (8%) | 17 (8%) | 78 (27%) | 67 (22%) | |||
| Exercise Duration (mean ± SD) | 5.3 ± 2.3 | 5.3 ± 2.2 | 0.99 | 8.4 ± 2.2 | 8.0 ± 1.7 | 0.02 | |
| METs achieved | <3 | 80 (33%) | 69 (31%) | 0 | 0 | ||
| 4-6 | 161 (67%) | 154 (69%) | 0 | 0 | |||
| 7-9 | 0 | 0 | 180 (63%) | 213 (71%) | |||
| >9 | 0 | 0 | 106 (37%) | 89 (29%) | |||
| METs achieved (mean ± SD) | 4.1 ± 1.3 | 4.2 ± 1.3 | 0.59 | 8.4 ± 2.1 | 8.0 ± 1.6 | 0.009 ∗ | |
| ST segment depressions (mm) | <1 | 67 (28%) | 63 (29%) | 0.80 | 95 (33%) | 101 (34%) | 0.80 |
| 1-2 | 126 (53%) | 120 (54%) | 132 (46%) | 142 (48%) | |||
| >2 | 47 (20%) | 38 (17%) | 59 (21%) | 55 (18%) | |||
During follow-up, a total of 58 patients died, and 108 patients sustained a nonfatal myocardial infarction. The event rates for the exercise capacity subgroups by randomized treatment assignment are provided in Table 3 . In patients with exercise capacity <7 METs, there was no difference in the primary end point between patients assigned to PCI + OMT versus OMT alone (19.1% vs 16.1%, p = 0.31). In patients with exercise capacity ≥7 METs, those assigned to PCI + OMT, despite achieving a higher mean MET level, had numerically more primary end points than those with OMT alone (13.3% vs 10.3%, p = 0.27). Overall, 67 patients in the OMT group crossed over to the PCI group in the first year after randomization, 27 (12%) in the <7 METs group, and 40 (13%) in the ≥7 METs group. There was no significant difference in the Kaplan–Meier cumulative event-free survival curves in patients with METs ≥7 and METs <7 by randomized treatment assignment ( Figures 2 and 3 ).



