Edema
Peter V. Vaitkevicius
Ragavendra R. Baliga
DEFINITIONS
Edema is an increase in the interstitial fluid volume and is typically first noted in the lower extremities. Often more than 4 kg of excess total body fluid may be present before the development of edema. Therefore it is typical to have a weight gain of several kilograms before the overt findings of swelling on the physical examination. The distribution of edema is generally proportional to the extent of collected interstitial fluid and may be diffuse or localized. Anasarca, or dropsy, defines a large and generalized accumulation of edema fluid. Depending on the mechanisms, both anasarca and smaller amounts of lower-extremity edema may be associated with ascites (accumulation of fluid in the peritoneal cavity) or a pleural effusion (accumulation of fluid in the pleural cavity). Dependent edema is the collection of fluid at specific sites in response to the hydrostatic effects of gravity and often first appears in the feet and ankles of ambulatory patients. Dependent edema in bed-bound patients is best assessed by examination of the posterior surfaces of the calves and sacrum. Pitting edema is demonstrated when the thumb is pressed into the skin against a bony surface—for example, over the tibia, fibula, or sacrum. When pressure is removed, an indentation persists, the depth of which should be estimated in millimeters as a means to score its severity. Lymphedema results from the obstruction of lymphatic channels and is often indistinguishable from edema produced by other mechanisms. When chronic, lymphedema is often nonpitting. Brawny edema defines a nonpitting fibrotic thickening of the subcutaneous tissues, which results from chronic tissue swelling (1).
PRINCIPLES OF EDEMA FORMATION (STARLING FORCES)
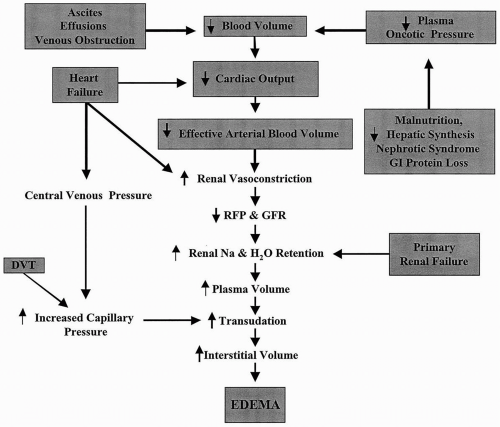
One third of the total body water is confined to the extracellular space (Fig. 4.1). The plasma volume constitutes 25% of the extracellular volume, and the remaining 75% is made up of the interstitial fluid volume. The hydrostatic pressure within the vascular system and the colloid oncotic pressure within the interstitial fluid facilitate the movement of fluid out of the vascular compartment and into extravascular space. The tissue tension (plasma colloid oncotic pressure and interstitial hydrostatic pressure) promotes the movement of fluid from the extravascular space into the vascular compartment. These forces are usually balanced, but if the oncotic or hydrostatic pressures are adversely altered, then the movement of fluid into the interstitial space or a body cavity occurs (2,3).
An increase in the capillary pressure may result from an elevation of venous pressure caused by a local obstruction in venous drainage. The increased venous pressure may be generalized, as with congestive heart failure (CHF), or localized, as with a deep venous thrombosis (DVT) (4). The plasma colloid oncotic pressure may be altered by hypoalbuminemia from malnutrition, liver disease, urinary protein loss, or a severe catabolic state. The reduction in oncotic pressure lessens the movement of interstitial fluid into the vascular compartment.
A decrease in the cardiac output (e.g., as in CHF) reduces the effective arterial blood volume and systolic blood pressure (hypotension) and decreases renal blood flow. Compensatory activation of the sympathetic nervous system and renin-angiotensin system promotes renal vasoconstriction, a reduction in renal salt and water excretion, and an expansion of the extracellular volume with edema formation. In addition, the mechanisms responsible for maintaining a normal serum osmolality are activated, promoting thirst and secretion of antidiuretic hormone. If the increase in total body salt and water is insufficient to restore and maintain an appropriate effective arterial volume, then the stimuli promoting renal salt retention are not turned off, and the severity of the edema is progressive.
The nephrotic syndrome and hepatic cirrhosis are associated with a severe reduction in serum albumin by either an increase in the loss of protein or a reduction in protein synthesis. The reduction in the plasma colloid oncotic pressure reduces plasma volume and the effective arterial blood volume, further promoting renal salt and water reabsorption (5).
Damage to the capillary endothelium increases vascular permeability and the movement of fluid and protein into the interstitial space. The vascular injury is often the result of infection, drugs, hypersensitivity reactions, or thermal or mechanical damage. This manner of vascular damage usually results in a nonpitting edema with associated inflammation. In addition, an occlusion of the lymphatic drainage of a specific site results in edema.
KEYS TO THE HISTORY
Distribution
Unilateral edema (Table 4.1) is a common clinical complaint, particularly of the lower extremities, and is routinely seen in the outpatient setting. Most patients with unilateral lower extremity edema should be considered for venous Doppler assessment to screen for the presence of a deep venous thrombosis (DVT), regardless of whether it is associated with pain (Chapter 32). Rectal, pelvic, and regional lymph node examinations should be conducted if a malignancy is suspected (6,7,8).
Besides a DVT, mechanisms for a painful unilateral swelling may include the following. The postphlebitic syndrome commonly follows a DVT (9). A ruptured popliteal (Baker) cyst produces posterior knee tenderness and occasionally petechiae and may clinically resemble a DVT (10). A tear or rupture of the gastrocnemius muscle is often acute and can be confused with a DVT (11). Soft tissue infections (cellulitis and fasciitis) can initially appear with swelling and pain, before the development of erythema or warmth. A psoas muscle hematoma or abscess can also produce unilateral swelling and may be associated with flank or hip pain as well as a painful leg-lift test result (psoas sign).
Bilateral lower extremity or generalized edema (Table 4.2) is the primary result of three mechanisms: an increase in central venous pressure, such as in pulmonary hypertension; renal sodium and water retention, as with a primary renal disease; or a reduction in cardiac output with activation of the sympathetic nervous system and the renin-angiotensin system, as seen with CHF. The distribution of the edema is influenced by the hydrostatic effects of gravity (dependent edema) and by the limitation in venous and lymphatic return, and the edema often accumulates in dependent structures such as the scrotum or the abdominal pannus in obese patients. Generalized edema limited primarily to above the diaphragm can result from infection, dermal irritants, or compression or obstruction of the superior vena cava and mediastinal vasculature, as is seen with chest neoplasms (12).
TABLE 4.1. Unilateral edema | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 4.2. Generalized edema | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
Chronic right ventricular failure may be the result of left ventricular dysfunction, pulmonary hypertension, or chronic lung disease. It produces marked bilateral edema, often with ascites, as a result of an increase in central venous pressure. Acute right-sided heart failure secondary to a large pulmonary embolism or a myocardial infarction also produces elevated central venous pressures.
A careful review of the history to seek evidence of chest pains consistent with angina or a prior cardiac history (myocardial infarction or angina) should be completed early in the evaluation of generalized edema. CHF resulting from left ventricular systolic or diastolic dysfunction, or both, is one of the most common mechanisms for bilateral edema and is often associated with pleural effusion or ascites. Hepatic cirrhosis is the end point of chronic liver disease (e.g., viral hepatitis, alcoholic liver disease). Edema of hepatic origin is primarily in the lower extremities and abdominal cavity and is proportional to the elevation in portal venous pressure. A history of a change in urinary frequency, hematuria, or foamy urine supports a renal process for the edema. The edema associated with the nephrotic syndrome (urinary protein loss of more than 3.0 g per day) is the result of a marked reduction in serum albumin and occasionally by venous thrombosis that results from the associated hypercoagulable state. Minimal-change disease, membranous glomerulopathies, diabetic renal disease, human immunodeficiency virus infection, glomerulosclerosis, and myeloma kidney are common causes of the nephrotic syndrome (13).
A careful review of the history to seek evidence of chest pains consistent with angina or a prior cardiac history (myocardial infarction or angina) should be completed early in the evaluation of generalized edema. CHF resulting from left ventricular systolic or diastolic dysfunction, or both, is one of the most common mechanisms for bilateral edema and is often associated with pleural effusion or ascites. Hepatic cirrhosis is the end point of chronic liver disease (e.g., viral hepatitis, alcoholic liver disease). Edema of hepatic origin is primarily in the lower extremities and abdominal cavity and is proportional to the elevation in portal venous pressure. A history of a change in urinary frequency, hematuria, or foamy urine supports a renal process for the edema. The edema associated with the nephrotic syndrome (urinary protein loss of more than 3.0 g per day) is the result of a marked reduction in serum albumin and occasionally by venous thrombosis that results from the associated hypercoagulable state. Minimal-change disease, membranous glomerulopathies, diabetic renal disease, human immunodeficiency virus infection, glomerulosclerosis, and myeloma kidney are common causes of the nephrotic syndrome (13).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree