51 Echocardiography in Congenital Heart Disease
Transthoracic Imaging in Pediatrics
Ejection fraction is similarly calculated, using measured LV volumes.
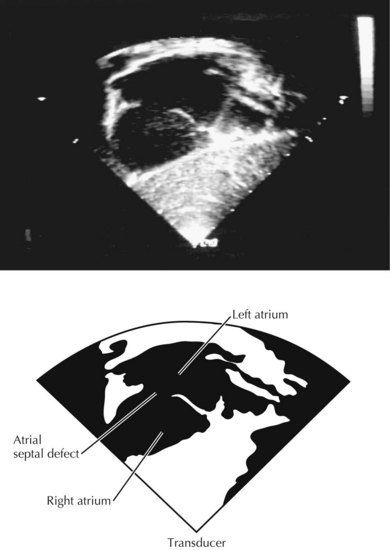
Atrial Septal Defect
TTE is often sufficient to define the size and location of an atrial septal defect (Fig. 51-1). Pulsed and color Doppler echocardiography identify the direction and amount of shunting at the atrial level. Other findings can confirm the presence of a hemodynamically significant shunt. For instance, right ventricular (RV) volume overload can produce diastolic bowing of the ventricular septum to the left during diastole, with the left ventricle assuming an elliptical shape. Partial anomalous pulmonary veins can be identified by 2D echocardiography and color Doppler, and can be corrected at the time of surgery. Echocardiography is usually sufficient to define the anatomy of the atrial septum and pulmonary veins in infants and small children. For older children and adults, TTE may be needed for full anatomic definition. Cardiac catheterization is not usually needed to evaluate atrial septal defects.
Ventricular Septal Defect
Multiple views are needed to visualize the entire interventricular septum. TTE with 2D imaging usually demonstrates the size and location of the interventricular communications. Color Doppler can be used to determine the direction of shunting across the ventricular septal defect (VSD) (Fig. 51-2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree