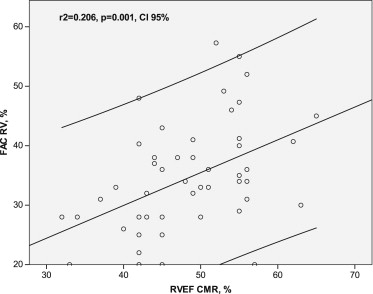
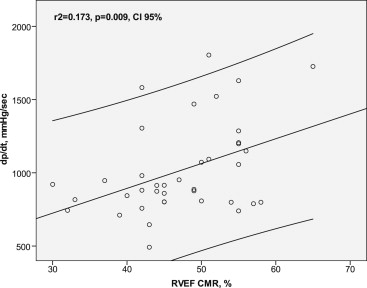
In adults with congenital heart disease and a systemic right ventricle, subaortic ventricular systolic dysfunction is common. Echocardiographic assessment of systolic right ventricular (RV) function in these patients is important but challenging. The aim of the present study was to assess the reliability of conventional echocardiographic RV functional parameters to quantify the systolic performance of a subaortic right ventricle. We compared 56 contemporary echocardiograms and cardiac magnetic resonance studies in 37 adults, aged 26.9 ± 7.4 years, with complete transposition and a subaortic right ventricle. The fractional area change (FAC), lateral tricuspid annular plane systolic excursion, lateral RV systolic motion velocities by tissue Doppler, RV myocardial performance index, and the rate of systolic RV pressure increase (dp/dt) measured across the tricuspid regurgitant jet were assessed by echocardiography and correlated with the cardiac magnetic resonance-derived RV ejection fraction (EF). The mean RVEF was 48.0 ± 7.8%. FAC (r 2 = 0.206, p = 0.001) and dp/dt (r 2 = 0.173, p = 0.009) significantly correlated with RVEF, and the other nongeometric echocardiographic parameters failed to show a significant correlation with RVEF by linear regression analysis. FAC <33% and dp/dt <1,000 mm Hg/s identified a RVEF of <50% with a sensitivity of 77% and 69% and a specificity of 58% and 87%, respectively. In conclusion, in patients with a systemic right ventricle, routine nongeometric echocardiographic parameters of RV function correlated weakly with cardiac magnetic resonance-derived EF. RV FAC and the measurement of the rate of systolic RV pressure increase (dp/dt) should be preferentially used to assess systemic systolic function in adult patients with a subaortic right ventricle.
A substantial number of adult patients with congenital heart disease have a biventricular circulation with a subaortic right ventricle (e.g., adults with congenitally corrected transposition of the great arteries or adults with a previous atrial switch procedure for complete transposition of the great arteries). Owing to its subaortic position, the right ventricle has to sustain systemic workload. The subaortic systolic right ventricular (RV) function declines with age, and reduced systemic systolic function is associated with heart failure, arrhythmias, and cardiac death. Adequate and reproducible assessment of systemic RV systolic function is important for patient management and guides medical, surgical, and device-based therapies. Just as in patients without congenital heart disease, transthoracic echocardiography is the first-line diagnostic technique to assess systemic systolic function during routine follow-up. However, echocardiographic assessment of systolic function in a subaortic right ventricle is challenging because of its complex geometry. Also, echocardiographic RV functional parameters used to assess a subpulmonary RV performance might not be applicable to a systemic right ventricle owing to different loading conditions nor any geometrical methods commonly used to quantify systolic function in a systemic left ventricle. The aim of the present study was to compare the different echocardiographic parameters of RV systolic function in adults with a subaortic right ventricle to the cardiac magnetic resonance imaging (CMR)-derived RV ejection fraction (EF) and to identify the most accurate echocardiographic parameters to detect systemic RV dysfunction in these patients, commonly defined as a CMR-derived RVEF <50%.
Methods
After approval from the ethical committee, all adult patients with complete transposition of the great arteries who had undergone an atrial switch operation in earlier life were identified from the Grown-Up Congenital Heart Disease database of the University Hospital Bern. We included all patients with regular follow-up data from 2006 to 2012, who had undergone echocardiography and CMR within 3 months, had a stable clinical course, and were in sinus rhythm at that time. Patients with a repeated CMR study and corresponding echocardiographic study within an interval of >3 years were included and analyzed as a second measure.
Echocardiograms were performed with commercially available machines (Sequoia Siemens, Erlangen, Germany, or IE33 Philips) by experienced sonographers and stored digitally (Syngo Dynamics Software, Siemens, Erlangen, Germany). A primary investigator (K.K.), who was unaware of the CMR results, performed a retrospective off-line analysis of 3 consecutive heart beat measurements of the following echocardiographic surrogates of RV function.
In an apical 4-chamber view, the RV size was traced along its endocardial border to measure the area at the end of diastole and systole. The fractional area change (FAC) was calculated as follows: (end-diastolic area − end-systolic area)/(end-diastolic area), according to the American Society of Echocardiography recommendations.
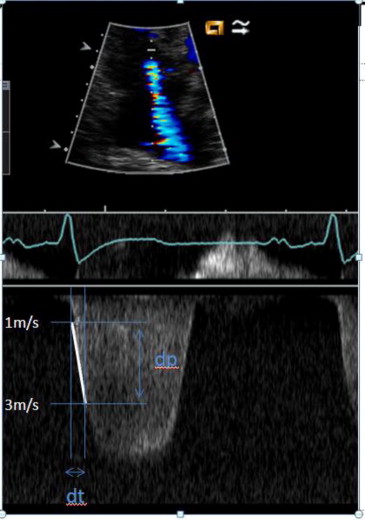
In the presence of tricuspid regurgitation, the regurgitant jet was sampled by continuous-wave Doppler in an apical 4-chamber view, using a sweep speed of ≥100 mm/s, and the baseline and scale were adjusted to maximize the spectral signal appropriately. To estimate the rate of systolic RV pressure increase (dp/dt), the time interval (dt) was calculated between the spectral envelope at 1 m/s and 3 m/s and divided by the pressure difference (dp) between those 2 measurements (i.e., 32 mm Hg according to the Bernoulli equation, Figure 1 ).
The M-mode cursor was oriented at the junction between the lateral portion of the tricuspid valve annulus and the RV free wall in the apical 4-chamber view. The lateral tricuspid valve annular systolic excursion was measured as the distance between the base and peak of the total excursion.
Pulsed-wave tissue Doppler imaging of the systolic lateral tricuspid annular motion velocity was obtained from the apical 4-chamber view with a sweep of 100 mm/s. Care was taken to obtain an ultrasound beam parallel to the direction of the tricuspid annular motion, to use minimal gain, with the high-pass filter reduced, and to eliminate noise signals. The pulsed-wave Doppler field was placed 1 cm above the tricuspid valve in the myocardial area.
Continuous-wave Doppler recordings of the systemic RV inflow and outflow signal were used to calculate the myocardial performance index. The duration of systemic atrioventricular valve regurgitation (a) and duration of systemic outflow signal (b) were measured in 3 consecutive beats but without breath hold. myocardial performance index was calculated from the averaged results according to the formula: (a − b)/b.
Interobserver variability for all echocardiographic measurements was assessed in a randomly selected set of 15 examinations by a second observer, who was unaware of both the initial echocardiographic results and the CMR data.
The CMR RVEF assessment was performed as follows. The study participants were examined in the supine position using a 1.5 Tesla (Magnetom Symphony) or a 3 Tesla (Magnetom Trio, both from Siemens Medical Solutions, Erlangen, Germany) whole body clinical magnetic resonance imaging system. Cardiac synchronization was obtained from 3 or 4 electrodes placed on the left anterior hemithorax. The ventricular short-axis stack was acquired using the cine steady state free precession technique with retrospective electrocardiographic gating. The cardiac short-axis orientation was determined from 3 scout images: a midventricular transaxial view, a cine breath-hold vertical long-axis view, and a cine breath-hold horizontal long-axis view. The basal short-axis slice was positioned beyond the level of the mitral valve plane, and the ventricles were imaged from the base toward the apex during end-expiratory breath holds in contiguous short-axis slices with an 8-mm slice thickness and no gap. CMR EF analysis was performed off-line by manually tracing the end-diastolic and end-systolic ventricular contours using commercially available software (Argus, version 4.01, Syngo MR B13, Siemens Medical Solutions) by a single experienced observer (A.W.) who was unaware of the echocardiographic results. All trabeculations were included in the RV cavity. The RV and left ventricular volumes were calculated from the area within the contours, and the slice thickness was calculated according to the modified Simpson rule (disk summation, no geometric assumption). For practical purposes, a RVEF of ≥50% was defined as normal, 40% to 49% as mildly reduced, 30% to 39% as moderately reduced, and <30% as severely reduced. However, the normal values for ventricular mass, volume, and EF in patients with a subaortic right ventricle have not yet been defined.
Data were analyzed using Stata (R) statistics data analysis, version 12.1 (StataCorp, College Station, Texas). p Values <0.05 were considered statistically significant. Correlation of echocardiographic parameters to systemic RVEF derived by CMR was calculated using linear regression analysis. The univariate predictors of CMR-derived RVEF were subsequently analyzed in a multivariate regression analysis. Stepwise backward elimination of nonsignificant predictors was performed at p >0.1. Receiver operating characteristic analysis was performed for all echocardiographic parameters to assess the diagnostic accuracy to detect normal RV function (defined as RVEF by CMR of ≥50%). Interobserver variability was calculated as the mean percentage of error, derived as the difference between 2 sets of measurements, divided by the mean observations. All data are presented as the mean ± SD.
Results
A total of 37 patients with a systemic right ventricle were identified from our database. The baseline characteristics of these patients are listed in Table 1 . A total of 56 corresponding echocardiographic and CMR studies were identified. In 16 patients with repeated CMR and echocardiographic examinations, the median interval between the first and second CMR examination was 39 months (range 32 to 47). The median interval between CMR and echocardiography was 0.6 month (range 0 to 3). In 75% of the cases, both examinations were performed the same day. The mean RVEF from the CMR study was 48.0 ± 7.8%. A preserved RV function, defined as an CMR-derived EF of ≥50%, was detected in 24 examinations, a mildly reduced RV function (EF 40% to 49%) in 26, and moderately or severely reduced RV function (RVEF <40%) in 6 examinations. New York Heart Association class ≥2 was present in 8 patients (13 examinations). One of these patients had severe regurgitation of the systemic atrioventricular valve at echocardiography (2 examinations), moderate regurgitation was present in 2 patients (2 examinations), 1 patient had a significant baffle leak (2 examinations), 1 patient had a baffle stenosis (1 examination), and 1 patient had severe pulmonary hypertension (2 examinations). No major difference was found in the CMR-derived RV systolic function in patients with New York Heart Association class ≥2 or New York Heart Association class 1 (RVEF was 44.9% vs 48.9%, respectively; p = 0.109). The corresponding mean values of the echocardiographic parameters for each category of RVEF are listed in Table 2 . FAC was obtained in 91% of examinations, lateral tricuspid annular motion velocity and tricuspid valve annular systolic excursion was measured in 93%, myocardial performance index was measured in 77%, and dp/dt in 70%.
| Male gender | 24 (65%) |
| Mean age at examination (yrs) | 26.9 ± 7.4 |
| Atrial switch operation | 37 |
| Mustard procedure | 21 |
| Senning procedure | 16 |
| New York Heart Association functional class ≥2 | 8 (22%) |
| Right Ventricular Ejection Fraction (%) | FAC (%) (n = 51) | dp/dt (mm Hg/s) (n = 39) | TAPSE (mm) (n = 52) | TVlat (cm/s) (n = 52) | MPI (n = 43) |
|---|---|---|---|---|---|
| ≥50 | 38.7 ± 9.5 (n = 22) | 1,167 ± 348 (n = 16) | 14.3 ± 3.0 (n = 24) | 9.7 ± 2.4 (n = 23) | 0.47 ± 0.2 (n = 18) |
| 40–49 | 31.8 ± 7.8 (n = 24) | 935 ± 267 (n = 18) | 12.7 ± 3.3 (n = 25) | 8.8 ± 2.7 (n = 25) | 0.48 ± 0.2 (n = 19) |
| 30–39 | 28.0 ± 4.9 (n = 5) | 828 ± 104 (n = 5) | 14.3 ± 2.3 (n = 3) | 8.3 ± 1.9 (n = 4) | 0.47 ± 0.1 (n = 6) |
Statistically significant correlations with CMR-derived RVEF were found for FAC (r 2 = 0.206, p <0.001) and dp/dt (r 2 = 0.173, p = 0.009; Figures 2 and 3 ). The results of the univariate regression analysis are listed in Table 3 . A cutoff FAC of <33% identified a CMR-derived RVEF of <50%, with a sensitivity of 77% and specificity of 58%. A dp/dt cutoff of <1,000 mm Hg/s identified a CMR RV function of <50%, with a sensitivity of 69% and specificity of 87% ( Table 4 ). The area under the curve was 0.73 for FAC and 0.72 for dp/dt ( Table 4 and Figure 4 ). No significant correlation to the CMR-derived RVEF was found for tricuspid valve annular systolic excursion, lateral right ventricular systolic motion velocities, and myocardial performance index. In a multivariate analysis with FAC and dp/dt as predictors of the RVEF, FAC (p = 0.039) was a slightly stronger predictor than dp/dt (p = 0.056).