Chapter 16 EBUS-TBNA of Right Lower Paratracheal Lymph Node (Station 4R)
Case Description
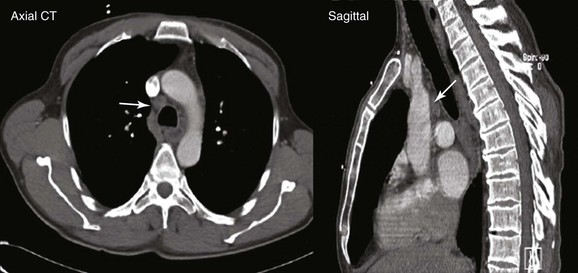
A 67-year-old Korean man with a 20–pack-year history of smoking was found to have an abnormal chest radiograph showing a right upper lobe pulmonary nodule during a routine preoperative evaluation for hernia repair. The patient had COPD (FEV1 50% of predicted) and pulmonary hypertension, presumptively related to his COPD (WHO group III*). An echocardiogram performed 3 months earlier showed a normal left ventricular ejection fraction and a pulmonary artery systolic pressure of 59 mm Hg with a tricuspid regurgitant velocity of 3.5 m/sec and an estimated right atrial pressure of 10 mm Hg. Computed tomography of the chest showed a 1.5 × 1-cm right upper lobe nodule and a 1.4-cm right lower paratracheal lymph node. He had no other past medical history and was in excellent health except for mild exertional dyspnea (NYHA class II). The patient was referred for tissue diagnosis (Figure 16-1).
Case Resolution
Initial Evaluations
Physical Examination, Complementary Tests, and Functional Status Assessment
After the pulmonary nodule was discovered on chest radiograph, this patient underwent a chest computed tomography (CT). In addition to the history and physical examination, CT scan of the chest is recommended in patients suspected of having lung cancer who are eligible for treatment, because its potential benefits for staging and treatment planning outweigh the relatively low risk of radiation-induced damage.1 CT scan of the chest should be obtained before bronchoscopy because having a more accurate appreciation of the size and location of the tumor increases the diagnostic yield of bronchoscopy, which is low, however, for peripheral pulmonary nodules smaller than 2 cm. Yield is high for diagnosis of larger nodules and for staging of mediastinal lymphadenopathy when sonographic guidance (endobronchial ultrasound–transbronchial needle aspiration [EBUS-TBNA]) is used.
This patient showed evidence of ipsilateral lymph node involvement (right lower paratracheal; 4R), but contralateral lymph node involvement was not suspected on the basis of CT. Positron emission tomography (PET)-CT has greater sensitivity for detecting metastasis in the mediastinum compared with CT, but this procedure had not been performed before the patient was referred to our institution. Nor had other diagnostic studies been performed to search for extrathoracic disease. For example, for patients with clinical stage IB-IIIB being considered for curative treatment, cranial magnetic resonance imaging (MRI) is recommended by some authorities to detect brain metastases, even if clinical examination findings are negative.1 We elected to perform additional tests on our patient for complete staging after a diagnosis had been made. We chose to recommend bronchoscopy and EBUS-guided TBNA for both diagnosis and mediastinal staging.
Comorbidities
This patient likely had pulmonary hypertension secondary to chronic obstructive pulmonary disease (COPD) based on a Doppler echocardiographic study showing a pulmonary artery systolic pressure (PASP) of 59 mm Hg with a tricuspid regurgitant velocity (TRV) of 3.5 m/sec.2 In general, pulmonary hypertension is considered likely if the PASP is greater than 50 and the TRV is greater than 3.4; unlikely if the PASP is 36 or less and the TRV is 2.8 or less, and no other suggestive findings are reported; and possible with other combinations of findings. Doppler echocardiography, however, may be misleading in patients with suspected pulmonary hypertension, especially when an inadequate tricuspid regurgitant jet cannot be properly assessed owing to a poor echocardiographic window. This was demonstrated in an observational study† of 65 patients with various types of pulmonary hypertension.3 The pulmonary arterial pressure estimated by Doppler echocardiography was at least 10 mm Hg higher or lower than that obtained by right heart catheterization in 48% of patients.* Therefore, a low threshold for right heart catheterization is warranted when patients with suspected pulmonary hypertension are evaluated. However, perioperative insertion of pulmonary artery catheters is not routinely recommended as a strategy to reduce perioperative mortality or postoperative pulmonary complications, even in high-risk surgical patients.4
Procedural Strategies
Indications
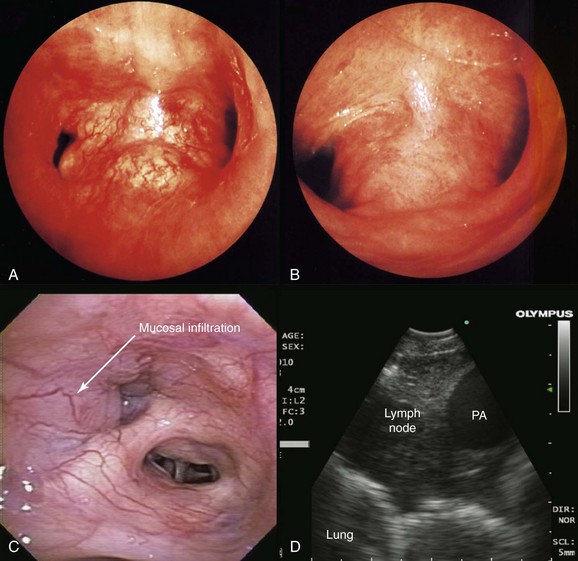
This patient likely had primary lung carcinoma. He needed a tissue diagnosis. We proposed bronchoscopy with EBUS-TBNA because the suspected N2 status (right lower paratracheal lymphadenopathy) had to be confirmed to decide on the need for further therapy: If N2 status were negative, therapy would be recommended for stage I-II non–small cell lung carcinoma (NSCLC) (with likely surgical resection once operability is determined); or for postoperative stage IIIA1* or IIIA2, according to strategies for stage IIIA. If, on the other hand, N2 status is known to be positive preoperatively, the patient would be assigned stage IIIA3 and would be treated according to the algorithm for stage IIIA. Careful white light bronchoscopic examination should be performed at the time of EBUS-TBNA because it may detect mucosal abnormalities, which may be malignant. Such findings would change the stage. For instance, in the setting of mediastinal lymphadenopathy, if the tracheal wall is involved, the tumor would be classified as T4 and therefore stage IIIB, but if no mucosal abnormalities are noted, the patient would have N2 disease, namely, stage IIIA (Figure 16-2); furthermore, if the needle passes through airway wall infiltrated with malignant cells before entering the lymph node target, the lymph node aspirate could become contaminated, and this could represent a false-positive aspirate. Thus we believe that abnormal airway mucosa at the puncture site should be biopsied (see Figure 16-2), and that bronchoscopists should do their best to avoid needle insertion through abnormal appearing tissue, if possible.†
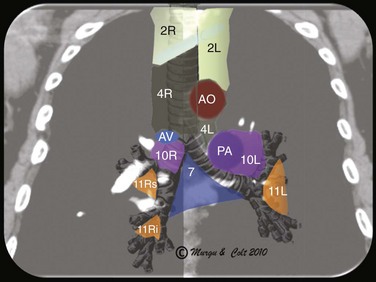
EBUS-TBNA can offer diagnosis and staging in one setting. With EBUS, one can potentially sample all stations adjacent to the trachea or bronchi (2, 4, 7, 10, 11) (Figure 16-3), but not level 5, 6, 8, and 9 lymph nodes.‡ Low-volume cytology specimens such as those obtained via EBUS-TBNA are considered adequate for molecular analysis, as with epidermal growth factor receptor (EGFR) and anaplastic lymphatic kinase (ALK).5,6 This is increasingly important because whole genome amplification enables multiple molecular analyses and may be used to expand starting deoxyribonucleic acid (i.e., DNA amplification) from low-volume lung biopsies, such as those obtained with EBUS-TBNA, for further analysis of advanced-stage NSCLC.7 It is noteworthy that even when the primary tumor (the pulmonary nodule) is biopsied and studied for gene alterations, molecular assessment of metastatic sites (e.g., lymph nodes) may change management decisions because of the possibility of genetic differences between primary tumor and metastatic sites caused by tumor heterogeneity.8,9 Mutations in genes involved in the EGFR/KRAS/BRAF pathway, for example, were shown to predict clinical response to EGFR-directed tyrosine kinase inhibitors (TKIs) in NSCLC patients. The presence of activating EGFR mutations and the absence of KRAS mutations have been shown to be favorable markers for response to EGFR-directed TKI therapy.9 One study, which compared the mutational status of EGFR, KRAS, and BRAF in primary tumors* (adenocarcinomas) with that in the corresponding lymph node metastases, found that mutations in primary tumors and lymph node metastases were identical in only 1 of 7 (14%) patients in case of EGFR mutation and in 11of 36 (31%) patients in case of KRAS mutation. Only one patient showed the same EGFR mutation in the primary tumor and corresponding lymph node metastasis. In this study, the remaining 6 patients had EGFR mutations identified in the primary tumor (3 patients) or in the lymph node metastasis (3 patients), but not in both. A different KRAS mutation in the primary tumor and the corresponding metastasis was seen in 1 patient, and 24 patients had KRAS mutations exclusively in primary (16 patients) or metastatic tumor (8 patients).9 These data suggest that the possibility of differences in the mutational status of EGFR, KRAS,† and BRAF‡ between primary tumors and corresponding lymph node metastases should be considered whenever these mutations are used for the selection of patients for EGFR-directed TKI therapy.9
Expected Results
The diagnostic rate of EBUS-TBNA for station 4R is 71% to 94%10,11 and, as has been mentioned, the likelihood of obtaining sufficient material for use in molecular analysis is high. The prevalence of genetic alterations seems to vary depending on the patient’s ethnicity; a meta-analysis of nine published studies showed that among those with adenocarcinoma, EGFR mutations were present in 48% of East Asian patients but in only 12% of those with other ethnicities.12 Relevant to our patient is that EGFR mutation is frequent among Koreans suffering from lung cancer. In one study, it was seen in 20 of 115 patients (17.4%).§13 Drugs that target mutant EGFR and ALK are now available, and it is possible that testing for prospective mutations could result in assigning a successful targeted therapy. For instance, erlotinib and gefitinib are already available to target mutant EGFR, and the ALK inhibitor crizotinib has demonstrated remarkable efficacy against ALK fusion–positive lung cancers.14
Other lung or nonlung primary tumors could be responsible for this patient’s presentation. For neuroendocrine tumors, correct classification of a tumor as small cell lung cancer (SCLC) or as large cell neuroendocrine carcinoma (LCNEC) is a particularly difficult problem because of the many overlapping features of these tumors.15 In the diagnosis of primary lung lesions, this distinction is important because of different treatment strategies. LCNEC is considered an NSCLC treated by surgical excision, whereas SCLC is usually treated with chemotherapy or chemoradiotherapy. Given the large numbers of background lymphocytes in EBUS-TBNA specimens, the distinction between lymphoid cells and a neuroendocrine tumor can be particularly difficult. If carcinoid is diagnosed, cytology specimens are often inadequate for a definitive diagnosis of typical or atypical morphology16—a crucial distinction in determining prognosis.
On a different note, the sensitivity and specificity of EBUS-TBNA for diagnosing mediastinal and hilar lymph node metastasis from nonpulmonary tumors (taken together) have been reported to be as high as 92.0% and 100%, respectively. Tumors encountered included colorectal, head and neck, ovarian, breast, esophageal, hepatocellular, prostate, renal, and germ cell cancers and malignant melanoma.17 For lymphoma, a small study evaluating patients with high pretest probability for lymphoma in a tertiary cancer center revealed an overall sensitivity of 90.9% and specificity of 100%.18 Larger, prospective studies showed that the sensitivity and the specificity of EBUS-TBNA for definitive diagnosis of lymphoma were 57% and 100%, respectively. Decreased diagnostic yield may be due in part to problems with the low-volume cytology specimens obtained via EBUS-TBNA. For example, baseline cellularity of the aspirates includes both lymphocytes and bronchial epithelial cells because specimens may be contaminated with bronchial epithelial cells captured when the needle traverses the bronchial wall; in addition, a variety of entities have overlapping cytomorphologic features, and a paucity of published literature pertains to cytomorphology of these tumors.15 For lymphoma, even though the diagnostic accuracy of EBUS-TBNA is less than that seen for other cancers, the procedure appears justified in patients with isolated mediastinal lymphadenopathy, given the significant proportion (76%) of patients with lymphoma who would thus avoid a surgical biopsy.19
Team Experience
Good communication with the cytopathologist is important to increase the yield of the procedure, because sample preparation, triage, and interpretation ultimately depend on the question being asked. The pathologist should be told whether the procedure is performed for suspected primary lung cancer, for staging purposes, or to rule out metastasis or second primaries. In patients with known or suspected lymphoma or infection, additional tests on samples may be warranted.* Failure to begin the procedure with an expected result in mind and failure of the pathologist to understand the question being asked contribute to suboptimal interpretation of cytologic findings.20
Diagnostic Alternatives
1. CT-guided percutaneous needle aspiration of the nodule: This technique has a high diagnostic rate (91%) but does not provide mediastinal staging and increases the risk for pneumothorax (5% to 60%).21
2. Esophageal ultrasound-guided fine-needle aspiration (EUS-FNA) alone: EUS alone is suitable for assessing lymph nodes in the posterior aspect of lymph node stations 4L, 5, and 7, and in the inferior mediastinum at stations 8 and 9. EUS alone has limited value for complete staging because right-sided nodes are usually inaccessible.
3. Mediastinoscopy: This approach is traditionally considered the gold standard for mediastinal staging. It is more invasive, and bronchoscopic airway inspection might still be required. Mediastinoscopy provides systematic exploration and biopsy under visual guidance of nodal stations 1, 2, 3, 4, and 7.
4. Combined EUS and EBUS followed by mediastinoscopy: Because EBUS alone provides no access to lymph node stations 5, 6, 8, and 9, a strategy combining endosonography (EUS and EBUS) and mediastinoscopy (if no nodal metastasis was detected at endosonography) resulted in greater sensitivity for mediastinal nodal metastases and fewer unnecessary thoracotomies (needed in only 1 of 7 patients) in comparison with mediastinoscopy alone.22 This study used thoracotomy with nodal dissection as the reference standard in both study groups. Although stage IIIA is likely in our patient with ipsilateral mediastinal lymphadenopathy, tissue confirmation was necessary because computed tomography is known to be inaccurate for staging purposes. In one study, up to 28% of patients with high clinical suspicion of nodal disease had mediastinal nodal metastases confirmed by mediastinoscopy despite negative EBUS-TBNA.23 Therefore, a negative EBUS-TBNA should be followed by mediastinoscopy in patients with suspected mediastinal nodal involvement based on CT or PET.
5. Thoracotomy with nodal dissection: In this patient with highly suspected mediastinal nodal disease, this technique is neither cost-effective nor therapeutically advantageous.
Risk-Benefit Analysis
No serious complications are reported in the published literature on EBUS-TBNA, but cough and bleeding at the puncture site are described infrequently, usually when procedures are performed under moderate (conscious) sedation.24 The benefits of performing this procedure were that diagnosis and staging could be done at the same time, expected yield was excellent, and specimens would be collected for genetic testing that potentially would be useful for selecting targeted therapy based on specific research protocols.
Informed Consent
After the risks, benefits, and alternatives were discussed, our patient chose to proceed with EBUS-TBNA. On further questioning, he stated he had no health care advance directives and had no intention of initiating one at that time. The importance of advance directives may not be equally appreciated by all ethnic groups. In one study, for example, a survey showed that no Korean respondents and few Hispanics had advance directives. Low rates of advance directive completion among nonwhites may reflect health care disparities, distrust of the health care system, different cultural perspectives regarding death and suffering, and differences in family dynamics and parent-child relationships.25
Techniques and Results
Anesthesia and Perioperative Care
The patient’s pulmonary hypertension could lead to perioperative complications. One study of 28 patients undergoing major or minor surgeries under general and regional anesthesia revealed a perioperative death rate of 7%.* Perioperative complications attributed to pulmonary hypertension occurred in 29% of patients, regardless of the underlying cause of the pulmonary hypertension. Most (92%) of the complications occurred in the first 48 hours following surgery, and risk factors for complications were greater for emergency and major surgery and with a long operative time (193 minutes vs. 112 minutes; P = .003).26 A larger study evaluated 145 surgical patients with pulmonary hypertension, excluding those in whom the condition was due to left heart disease.27 Complications included respiratory failure (n = 41), cardiac arrhythmia (n = 17), congestive heart failure (n = 16), renal insufficiency (n = 10), and sepsis (n = 10), and risk predictors included a history of pulmonary embolus, NYHA functional class of II or greater, intermediate- or high-risk surgery, and a duration of anesthesia greater than 3 hours.
Our patient underwent the procedure in the operating room, under general anesthesia, and was intubated with a No. 9 endotracheal tube (ETT). With this method, the EBUS scope is directed more centrally in the airway; this could make needle aspirations more difficult, especially if the nodes are laterally located. In such cases, the ETT is moved proximally in the upper trachea—a maneuver that may provide more space for manipulating the scope inside the lower trachea. Laryngeal mask airway (LMA) can also be used instead of ETT for this purpose. In addition, LMA permits evaluation of the upper paratracheal nodes, which may not be accessible if an ETT is used.†28 EBUS can also be performed under moderate sedation in the bronchoscopy suite. This may result in safety and cost savings compared with general anesthesia, but aspiration of smaller nodes is technically more difficult.29 Furthermore, at the time of this writing, most published studies of EBUS-TBNA showing high diagnostic rates were done with the patient under general anesthesia.
Technique and Instrumentation
We used a dedicated EBUS bronchoscope (BF-UC180 F, Olympus, Tokyo, Japan) with an integrated convex transducer at the tip of the scope, which scans parallel to the insertion direction of the bronchoscope, and a 22-gauge needle to perform TBNA (NA-201SX-4022, Olympus). After the lymph node had been penetrated, the internal stylet was used to push out the bronchial wall debris, which may clog the internal lumen, and then the stylet was removed. Negative pressure can be applied with a syringe and the needle moved back and forth inside the target 10 to 15 times over 30 to 60 seconds.30 In some instances, the bronchoscopist may choose to avoid suction, having obtained the specimen simply through needle insertion into the node.
Many times, the bronchoscopist notices the needle in the lesion, but aspirates are acellular, or only blood or bronchial cells are seen. From a “targeting” perspective, the node is properly accessed, but acquisition of lymph node material is suboptimal. The question that may have to be asked is not whether the needle is in the lesion, but whether the lesion is in the node.31 This means that penetration of the needle into the node does not guarantee the presence of lymph node tissue inside the needle. In this regard, the principles of any fine-needle aspiration technique include the following: (1) Ensure the cutting action of the needle by performing a fast, downstroke movement (see video on ExpertConsult.com) (Video IV.16.1![]() ); and (2) minimize the amount of blood in the sample by following a straight needle trajectory, for instance, if the node is sampled from different entry locations, the needle should be repositioned outside the target first, thus avoiding tissue tearing and minimizing suction within the target, especially for vascular nodes (i.e., renal cell carcinoma, melanoma). High negative pressure may rupture nodal capillaries (see video on ExpertConsult.com) (Video IV.16.2
); and (2) minimize the amount of blood in the sample by following a straight needle trajectory, for instance, if the node is sampled from different entry locations, the needle should be repositioned outside the target first, thus avoiding tissue tearing and minimizing suction within the target, especially for vascular nodes (i.e., renal cell carcinoma, melanoma). High negative pressure may rupture nodal capillaries (see video on ExpertConsult.com) (Video IV.16.2![]() ). Minimizing or eliminating suction altogether, while moving the needle fewer than a dozen times inside the node, reduces transit time and potentially decreases the chance for retrieving blood clot rather than a tissue sample.31 With a cytologist available for rapid on-site examination (ROSE) of the aspirates, TBNA is continued until adequate sampling is confirmed. Without ROSE, three aspirates per lymph node station or two aspirations with one core tissue specimen is recommended.32 Feedback from the cytopathologist, whether obtained at the time of ROSE or later after final results are available, is important to improve one’s technique. Operators can examine the quality of their stained smears to judge adequacy and quality of the aspirates.* In addition to technique, other reasons for false-negative aspirates have been identified, including partial tumor invasion within the lymph node. Complementary optical technologies such as spectroscopy or optical coherence tomography may have a role in the future by directly guiding needle aspiration toward abnormal zones within lymph nodes.33,34
). Minimizing or eliminating suction altogether, while moving the needle fewer than a dozen times inside the node, reduces transit time and potentially decreases the chance for retrieving blood clot rather than a tissue sample.31 With a cytologist available for rapid on-site examination (ROSE) of the aspirates, TBNA is continued until adequate sampling is confirmed. Without ROSE, three aspirates per lymph node station or two aspirations with one core tissue specimen is recommended.32 Feedback from the cytopathologist, whether obtained at the time of ROSE or later after final results are available, is important to improve one’s technique. Operators can examine the quality of their stained smears to judge adequacy and quality of the aspirates.* In addition to technique, other reasons for false-negative aspirates have been identified, including partial tumor invasion within the lymph node. Complementary optical technologies such as spectroscopy or optical coherence tomography may have a role in the future by directly guiding needle aspiration toward abnormal zones within lymph nodes.33,34
After we retrieved our specimen, the aspirated material was pushed onto a glass slide. We did not retrieve a core of tissue,* but if this had been obtained, it could have been placed on filter paper to absorb excess blood and then fixed with 10% neutral buffered formalin, so that a formalin-fixed paraffin-embedded sample would have been made and further stained with hematoxylin and eosin for histologic diagnosis.†30 The rest of the material was smeared onto glass slides for both air-dried smears and was immediately fixed with 95% ethanol smears. The air-dried smears were stained by Diff-Quick staining for ROSE or Giemsa stain solution. The ethanol-fixed smears were sent for Papanicolau staining. The contents of the EBUS-TBNA needle were washed into a tube containing saline and were used for molecular testing if warranted.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree