Chapter 19 Dyspnea
Mechanisms of Dyspnea
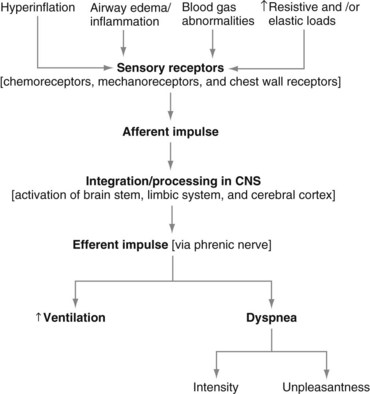
The neurophysiologic pathways that mediate the control of breathing (to supply oxygen, to eliminate carbon dioxide, and to maintain acid-base balance) also are relevant to the mechanisms of dyspnea (Figure 19-1). In simple terms, nerve fibers (sensory receptors) send electrical signals (afferent impulses) to the spinal cord, which in turn transmits these signals to the brain.
The Language of Dyspnea
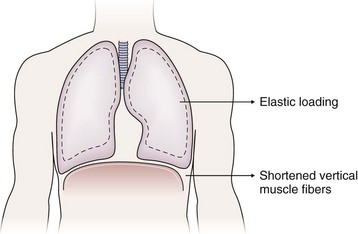
The sense of respiratory work or effort commonly is reported by patients with various conditions including asthma, COPD, interstitial lung disease, and neuromuscular disease. The descriptor “work/effort” of breathing difficulty probably is related to activation of respiratory muscle afferents imposed by mechanical loads (airway narrowing → added resistance; parenchymal edema/infiltrates → added elastance) imposed by certain diseases as well as respiratory muscle weakness. For example, in patients with COPD, the lungs typically hyperinflate during the performance of physical tasks. This dynamic hyperinflation results in two major consequences that contribute to dyspnea: (1) an added elastic load and (2) functional weakening of the diaphragm by shortening of the vertical muscle fibers (Figure 19-2). Although patients with acute asthma initially may experience chest tightness, they typically report that the increased work or effort of breathing develops as airway narrowing progresses as a result of subsequent lung hyperinflation.
Acute Dyspnea
Initial Evaluation
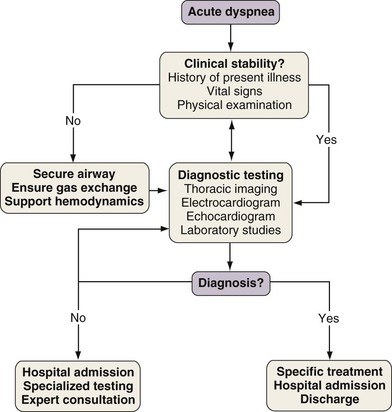
With any clinical encounter, the focus of the initial assessment is on whether or not the patient is stable (Figure 19-3). If this evaluation reveals evidence of hemodynamic insult or lability, hypotension may need to be treated promptly with intravenous fluids, vasopressors, and/or vasodilators. Airway patency and adequacy may be threatened by a depressed level of consciousness, aspiration, or trauma. Endotracheal intubation may become necessary in such instances and when gas exchange derangements cannot be rectified by supplemental oxygen or noninvasive positive-pressure ventilation. Once these basic support elements are addressed, diagnostic testing can safely proceed.
Differential Diagnosis
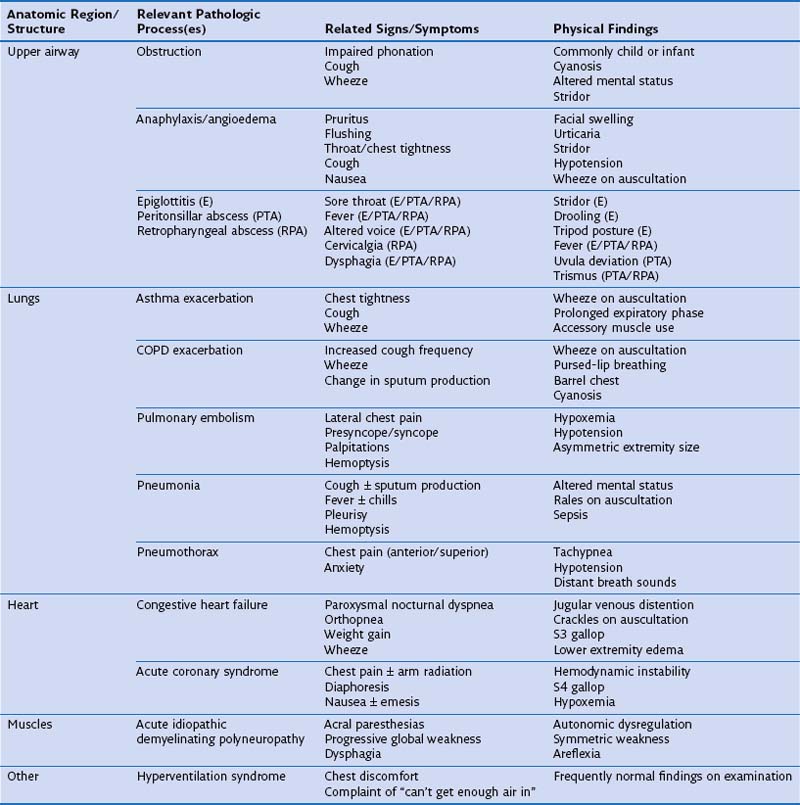
One approach to the differential diagnosis for acute dyspnea is to consider how processes in certain anatomic regions contribute to this symptom (Table 19-1). Obstruction is the most common mechanism for dyspnea arising from upper airway problems. Stridor, a variably high-pitched, harsh inspiratory noise caused by turbulent airflow, often can be heard in the context of an aspirated foreign body and edema of the epiglottis and laryngeal soft tissues. Prompt evaluation and management of upper airway blockage are critical, because the airway is endangered. Exacerbations of asthma and COPD typically are manifested as bronchospasm, wheeze, and cough. Sputum production is common to exacerbations of COPD associated with acute bronchitis and pneumonia, but its physical characteristics alone are not useful in predicting a causative pathogen. Pleuritic chest pain is sharp, incisive, breath-taking discomfort caused by irritation of the parietal pleural nerve supply along the thoracic cavity. This type of pain can accompany pulmonary embolism, pneumonia with or without pleural effusion, and pneumothorax.