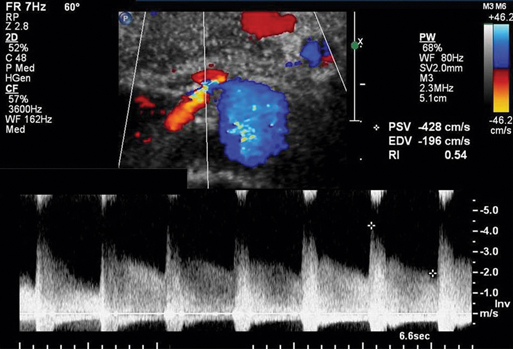
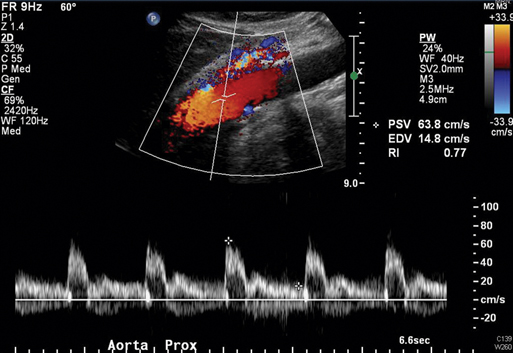
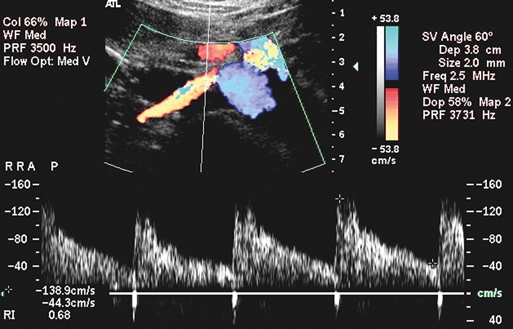
The abdominal aorta is evaluated initially to determine if there is aneurysmal or occlusive disease, and the aortic peak systolic velocity (PSV) is measured at the level of the superior mesenteric artery (Figure 1). The origins of the main renal arteries are most commonly identified from a midline approach, with the aorta in transverse view, located just distal to the superior mesenteric artery, and near the level of the left renal vein as it crosses anterior to the aorta. An attempt should also be made to locate and evaluate accessory renal arteries. Classification of renal arterial occlusive disease by duplex scanning is based on velocity waveforms from the renal artery and adjacent abdominal aorta. The triphasic flow pattern seen in the aortoiliac and lower extremity arteries is a result of the relatively high vascular resistance of the normal peripheral circulation. In contrast, the normal kidney offers a low vascular resistance, and the renal artery velocity waveform is monophasic with forward flow throughout the cardiac cycle (Figure 2). This low-resistance waveform is also characteristic of the normal internal carotid artery and celiac axis. Renal artery narrowing results in a focally increased renal artery PSV. Normal renal arteries typically show PSV values of less than 180 cm/sec. Because the PSV associated with a significant renal artery stenosis increases relative to aortic PSV, the ratio of peak systolic velocities in the renal artery and aorta can be used as an index of severity of a renal artery stenosis. This is referred to as the renal-to-aortic ratio (RAR). An RAR of 3.5 or greater is commonly used to identify a 60% or greater renal artery stenosis (Figure 3). However, like the ankle-to-brachial pressure index, this diagnostic ratio compares the arterial site of interest to a normal reference site.
Duplex Scanning in the Evaluation of Renal Arterial Occlusive Disease
Scanning Technique
Interpretation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine