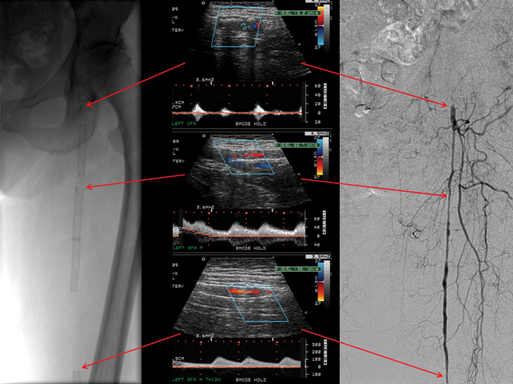
Color flow greatly aids duplex examination of lower extremity arteries, particularly the iliac and tibial arteries. It facilitates establishing vessel location, helps identify points of turbulence associated with stenoses, and can determine the length of arterial occlusions while identifying reconstitution of occluded vessels (Figure 1). Measurements of diameter from the color-flow image are less accurate than spectral analysis in quantifying stenoses. As a result, spectral analysis is required to accurately quantify stenoses. It is important to remember that color is a display of average, not peak, velocity shifts and that it changes with changes in the angle of insonation. Clinical application of duplex mapping to the lower extremity arteries, therefore, begins with color flow to identify the arteries and ensure a reliable Doppler angle. Depending on the color settings, it CAN help localize areas suspicious for stenoses, but only elevated peak systolic velocities are a reliable indication of a significant stenosis. Points within a vessel that do not fill on color flow and do not have an associated Doppler signal indicate occlusion. Duplex criteria for grading isolated stenoses in the iliac, femoral, and popliteal arteries were first proposed by Jäger and colleagues (Table 1). These early criteria depended heavily on analysis of spectral broadening for detecting stenoses of less than 50% reduction in diameter. Because spectral broadening is difficult to quantify in clinical studies and can be increased by increasing sample volume size and/or the gain control of the duplex scanner, spectral broadening for clinical purposes is not particularly useful in quantifying lower extremity arterial stenoses less than 50%. However, the criteria for 50% to 99% stenosis have proved quite accurate in prospective blinded clinical studies (Table 2). TABLE 1 Original Spectral Criteria for Duplex-Identified Stenoses in Lower Extremity Arteries From Jäger KA, Phillips DJ, Martin RL, et al: Noninvasive mapping of lower limb arterial lesions, Ultrasound Med Biol 11:515–521, 1985. TABLE 2 Values for Duplex Scanning in Detecting 50% or Greater Stenoses in Lower Extremity Arteries Proximal to the Tibial Vessels
Duplex Imaging of Infrainguinal Occlusive Disease
Equipment and Technique
Velocity Waveforms and Criteria Defining Stenoses
Percentage of Stenosis
Criteria
0
Normal waveforms and velocities
1–19
Normal waveforms and velocities
Spectral broadening primarily on the down slope of the systolic portion of the velocity curve
20–49
Normal triphasic waveform with marked spectral broadening
There is at least a 30% increase in peak systolic velocity
50–99
Loss of end systolic reverse flow
100% or more increase in peak systolic velocity
Occluded
No detectable Doppler signal in an adequately visualized vessel
ILIAC
COMMON FEMORAL
DEEP FEMORAL
SUPERFICIAL FEMORAL
POPLITEAL
Author
No. of Patients
Sens
Spec
PPV
NPV
Sens
Spec
PPV
NPV
Sens
Spec
PPV
NPV
Sens
Spec
PPV
NPV
Sens
Spec
PPV
NPV
Kohler et al.
32
89
90
75
96
67
98
80
96
67
81
53
88
84
93
90
88
75
97
86
93
Moneta et al.
150
89
99
94
97
76
99
93
96
83
97
83
97
87
98
97
89
67
99
93
94
Cossman et al.
61
81
98
94
92
70
97
78
96
71
95
56
97
87
85
86
72
84
97
93
93
Aly et al.∗
90
89
99
92
99
NA
NA
NA
NA
100
99
95
100
95†
99†
94†
99†
95†
99†
94†
99† ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Duplex Imaging of Infrainguinal Occlusive Disease
