Duplex guidance should be performed by an experienced vascular technologist with an extensive proficiency in preoperative duplex arteriography. Guidance for balloon angioplasty procedures requires the technologist to be gowned and gloved and the duplex scanner’s keyboard to be covered by a sterile film. We routinely use an HDI 5000 scanner with SonoCT feature (Philips Medical Systems, Bothell, WA). A variety of duplex probes inserted in a sterile plastic sleeve with coupling gel are used to insonate the arteries according to anatomic location and depth. Generally, the arteries in the thigh and calf (1–4 cm deep) are visualized with a linear 7–4 MHz scanhead. More superficial (<1 cm deep) arterial structures at the ankle and foot can be insonated by a compact linear 15–7 MHz hockey stick probe. Addition of a curved 5–2 MHz transducer is necessary for assessing deeper arterial segments, including distal superficial femoral artery (SFA) and above-the-knee popliteal artery.
One of the distinct advantages of the proposed technique is the possibility to perform the majority of the procedures through an ipsilateral puncture. This has several benefits: prevention of potential complications of contralateral groin puncture, use of shorter endovascular devices that are easier to manipulate, and avoidance of potential difficulties and complications of aortoiliac disease and variable anatomy. Direct duplex visualization allows puncturing the softest and the thinnest portion of arterial wall and helps avoid dissections, posterior wall puncture, bleeding, and other potential problems associated with blind arterial punctures.
Ipsilateral CFA duplex-guided access is possible in the majority of cases. In our experience with 402 femoral–popliteal angioplasties, 370 (92%) cases were performed by way of the ipsilateral CFA, with contralateral cannulation necessary in the remaining 32 cases (8%). Contralateral CFA access required fluoroscopy (alone in six cases and with 10–20 mL of contrast in the remaining 26 cases) for the ipsilateral common iliac artery cannulation. General contraindications for antegrade ultrasound-guided CFA puncture are a high bifurcation and/or deep location (≥3 cm from the skin).
After a successful ipsilateral CFA cannulation, a guidewire is directed into the proximal SFA, threaded across the diseased segment(s), and parked at the tibioperoneal trunk or one of the tibial arteries under duplex guidance. In cases of a contralateral CFA access, fluoroscopy is used to cross the aortic bifurcation. After the guidewire is identified by duplex in the ipsilateral proximal CFA, the procedure should be continued with duplex guidance.
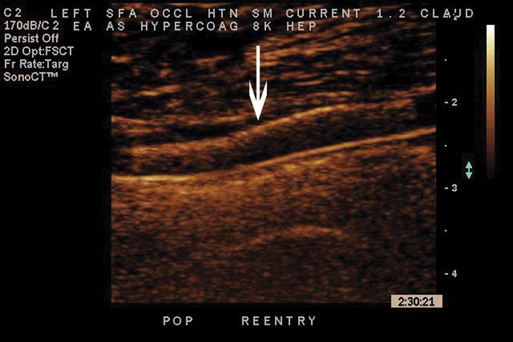
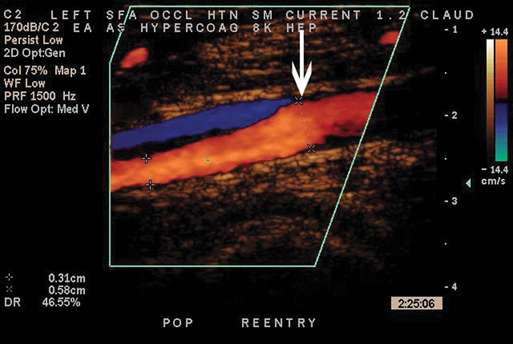
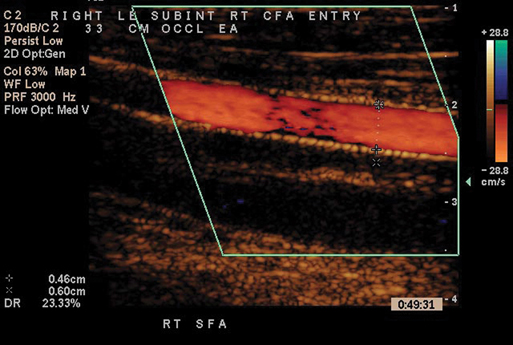
In cases of femoral and popliteal occlusions, a directional catheter supporting the guidewire is pointed against the wall 3 to 5 mm proximal to the occlusion to initiate subintimal dissection. Wire loop formation is confirmed by duplex imaging. Advancement of the wire through the occlusion is followed to the patent arterial segment, which is identified by the presence of color filling the lumen. Reentry attempts should be initiated within the first 1 to 2 cm after flow reconstitution to minimize the length of angioplasty. The arterial segment with the least amount of calcification and thinnest intima–media layer should be preferably chosen for reentry. If the guidewire fails enter the true lumen after several attempts, the directional catheter should be advanced and pointed toward the lumen for additional wire support. Reentry efforts are usually continued cautiously to prevent extension of the dissection plane to the popliteal artery below the knee. We always try to spare the outflow artery for a possible femoropopliteal bypass in case of subintimal angioplasty failure. After the guidewire enters the true arterial lumen, its position is confirmed with color flow imaging in both longitudinal and transverse planes.
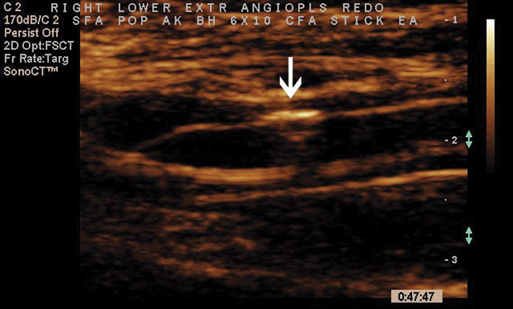
The diseased segment is then balloon dilated under duplex guidance (Figure 1). Balloon diameter and length are chosen based on direct arterial measurements obtained by the duplex examination. Duplex image magnification (up to 5 times) and minimal error of the measurements (0.1 mm) provide precise measurements of the arterial diameter and of lumen and wall thickness, which eliminates over- or undersizing of balloon and stents.
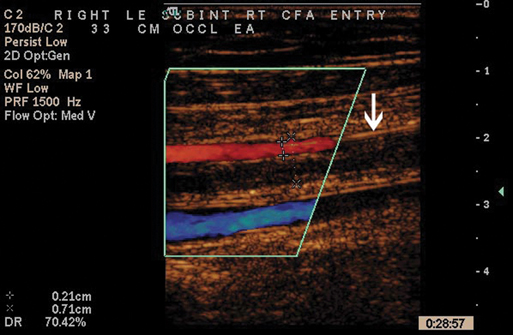
A thorough duplex examination of the entire treated segment should be performed immediately after removing the balloon angioplasty catheters to identify possible areas of residual disease, thrombi, plaque dissection, or recoil. Residual disease and plaque recoils are identified as luminal defects partially obstructing the flow (Figure 2). Partial or occlusive arterial thrombi have an anechoic intraluminal appearance. Dissections can be diagnosed by the bidirectional flow pattern or flow separation with clearly different velocities as shown by color Doppler (Figure 3). All suspected abnormalities are carefully evaluated by direct diameter reduction measurement on color and/or power images as well as spectral analyses including peak systolic velocity (PSV) ratios. Luminal defects of more than 30% diameter reduction with PSV ratio of 2 or more across the stenosis can be treated by placing self-expanding stents under duplex guidance (Figures 4 and 5). Finally, the infrapopliteal arteries are insonated to reassure absence of embolization or thrombosis.
Only gold members can continue reading.
Log In or
Register to continue
Related
![]()