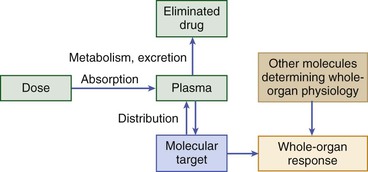
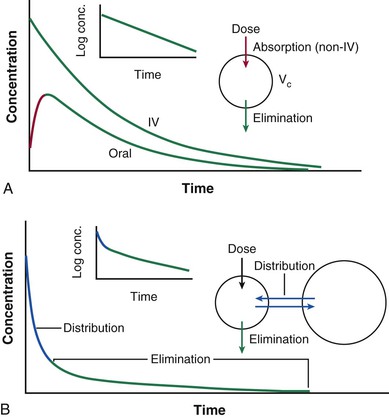
Dan M. Roden Drug treatment makes up a large fraction of total health care costs. In 2008, the total cost of healthcare in the United States was approximately $2.5 trillion, and more than 10% was spent on prescription drugs.1 Cardiovascular disease makes up the largest subcategory in this spending: The American Heart Association estimated that the 2008 cost of care for cardiovascular disease was $298 billion, and total prescription drug costs for cardiovascular care were $33 billion.2 Patients vary in their responses to drug treatment, and multiple mechanisms can be invoked, such as poor compliance, variable impact of diverse disease mechanisms on drug actions, drug interactions, and an increasingly recognized role of genomic variation. Indeed, adverse drug reactions across all therapeutic categories are estimated to be the fourth to the sixth most common cause of death in the United States, costing $19 to $27 billion annually, and accounting directly for 3% to 6% of all hospital admissions.3 This chapter outlines principles of drug action, the major mechanisms underlying variability in drug effects, and current and future approaches to enable the safest and most effective therapy for an individual patient. The fundamental assumption underlying administration of any drug is that the real or expected benefit exceeds the anticipated risk. The benefits of drug therapy are initially defined in small clinical trials, perhaps involving several thousand patients, before a drug’s marketing and approval. Ultimately, the efficacy and safety profiles of any drug are determined after the compound has been marketed and used widely in hundreds of thousands of patients. When a drug is administered for the acute correction of a life-threatening condition, the benefits are often self-evident; insulin for diabetic ketoacidosis, nitroprusside for hypertensive encephalopathy, and lidocaine for ventricular tachycardia are examples. Extrapolation of such immediately obvious benefits to other clinical situations may not be warranted, however. The efficacy of lidocaine to terminate ventricular tachycardia led to its widespread use as a prophylactic agent in cases of acute myocardial infarction, until it was recognized that in this setting, the drug does not alter mortality rates. The outcome of the Cardiac Arrhythmia Suppression Trial (CAST) highlights the difficulties in extrapolating from an incomplete understanding of physiology to chronic drug therapy. CAST tested the hypothesis that suppression of ventricular ectopic activity, a recognized risk factor for sudden death after myocardial infarction, would reduce mortality; this notion was highly ingrained in cardiovascular practice in the 1970s and 1980s. In CAST, sodium channel–blocking antiarrhythmics did suppress ventricular ectopic beats but also unexpectedly increased mortality threefold. Similarly, with the development of a first-generation cholesterol ester transport protein (CETP) inhibitor, the goal of elevation of high-density lipoprotein (HDL) levels was achieved, but with an accompanying increase in mortality. Thus, the use of arrhythmia suppression or of HDL elevation as a surrogate marker did not produce the desired drug action, reduction in mortality, probably because the underlying pathophysiology or full range of drug actions were incompletely understood. Similarly, drugs with positive inotropic activity augment cardiac output in patients with heart failure but also are associated with an increase in mortality, probably as a consequence of drug-induced arrhythmias. Nevertheless, clinical trials with these agents suggest symptom relief. Thus, the prescriber and the patient may elect therapy with positive inotropic drugs to realize this benefit while recognizing the risk. This complex decision making is at the heart of the broad concept of personalized medicine that incorporates into the care of an individual patient not only genomic (or other) markers of variable drug responses but also factors such as patients’ understanding of their disease and their willingness to tolerate minor or serious risks of treatment. The risks of drug therapy may be a direct extension of the pharmacologic actions for which the drug is actually being prescribed. Excessive hypotension in a patient taking an antihypertensive agent and bleeding in a patient taking a platelet IIb/IIIa receptor antagonist are examples. In other cases, adverse effects develop as a consequence of pharmacologic actions that were not appreciated during a drug’s initial development and use in patients. Rhabdomyolysis occurring with HMG-CoA reductase inhibitors (statins), angioedema developing during ACE inhibitor therapy, and torsades de pointes arising during treatment with noncardiovascular drugs such as thioridazine or pentamidine are examples. Of importance, these rarer but serious effects generally become evident only after a drug has been marketed and extensively used. Even rare adverse effects can alter the overall perception of risk versus benefit and can prompt removal of the drug from the market, particularly if alternate therapies thought to be safer are available. For example, withdrawal of the first insulin sensitizer, troglitazone, after recognition of hepatotoxicity was further spurred by the availability of other new drugs in this class. The recognition of multiple cyclooxygenase (COX) isoforms led to the development of specific COX-2 inhibitors to retain aspirin’s analgesic effects but reduce gastrointestinal side effects. However, one of these, rofecoxib, was withdrawn because of an apparent increase in cardiovascular mortality. The events surrounding the withdrawal of rofecoxib have important implications for drug development and utilization. First, specificity achieved by targeting a single molecular entity may not necessarily reduce adverse effects; one possibility is that by inhibiting COX-2, the drug removes a vascular protective effect of prostacyclin. Second, drug side effects may include not only readily identifiable events such as rhabdomyolysis or torsades de pointes but also an increase that may be difficult to detect in events such as myocardial infarction that are common in the general population. Two major processes determine how the interaction between a drug and its target molecule(s) can generate variable drug actions in a patient (Fig. 9-1). The first, pharmacokinetics, describes drug delivery to and removal from the target molecule and includes the processes of absorption, distribution, metabolism, and excretion—collectively termed drug disposition. The second process, pharmacodynamics, describes how the interaction between a drug and its molecular target(s) generates downstream molecular, cellular, whole-organ, and whole-body effects. The framework shown in Figure 9-1 identifies a series of genes that mediate clinical drug actions, and in which variants may thus contribute to variable drug actions. These genes encode drug-metabolizing enzymes, drug transport molecules, drug targets, and molecules modulating the biology in which the drug-target interaction occurs. The latter include molecular perturbations that cause the disease being targeted. Pharmacogenetics describes the concept that individual variants in the genes controlling these processes contribute to variable drug actions, whereas pharmacogenomics describes the way in which variability across multiple genes, up to whole genomes, explains differences in drug response among individuals and populations. Presented next is an overview of broad principles of pharmacokinetics, pharmacodynamics, and pharmacogenomics, followed by more detailed discussions of the specific genes, their function, and important variants influencing cardiovascular drug responses. Drugs can exert variable effects, even in the absence of pharmacokinetic variability. As indicated in Figure 9-1, this can arise as a function of variability in the molecular targets with which drugs interact to achieve their beneficial and adverse effects, as well as variability in the broader biologic context within which the drug-target interaction takes place. Variability in the number or function of a drug’s target molecules can arise because of genetic factors (see later) or because disease alters the number of target molecules or their state (e.g., changes in the extent of phosphorylation). Simple examples of variability in the biologic context are high dietary salt, which can inhibit the antihypertensive action of beta blockers, and hypokalemia, which increases the risk for drug-induced QT prolongation. In addition, disease itself can modulate drug response. For example, the effect of lytic therapy in a patient with no clot is manifestly different from that in a patient with acute coronary thrombosis, or the vasodilating effects of nitrates, beneficial in patients with coronary disease with angina, can be catastrophic in patients with aortic stenosis. These examples highlight the requirement for precision in diagnosis to avoid situations in which risk outweighs potential benefit. One hope is that emerging genomic or other molecular approaches can add to this precision. The targets with which drugs interact to produce beneficial effects may or may not be the same as those with which drugs interact to produce adverse effects. Drug targets may be in the circulation, at the cell surface, or within cells. Many newer drugs have been developed to interact with a specific drug target; examples of such targets are 3-hydroxy-3-methyl-glutaryl–coenzyme A (HMG-CoA) reductase, angiotensin-converting enzyme (ACE), G protein–coupled receptors (e.g., alpha, beta, angiotensin II, histamine), and platelet IIb/IIIa receptors. Such targets generally are identified in the course of basic mechanistic studies; a very appealing newer approach is to use modern genetic techniques to identify DNA variants associated with desired phenotypes, such as absence of myocardial infarction, as a clue to identify new drug targets.4 On the other hand, many drugs widely used in cardiovascular therapeutics were developed when the technology to identify specific molecular targets simply was not available; digoxin, amiodarone, and aspirin are examples. Some, like amiodarone, have many drug targets. In other cases, however, even older drugs turn out to have rather specific molecular targets. The actions of digitalis glycosides are mediated primarily by the inhibition of Na+,K+-ATPase. Aspirin permanently acetylates a specific serine residue on the COX enzyme, an effect that is thought to mediate its analgesic effects and its gastrointestinal toxicity. With repeated doses, drug levels accumulate to a steady state, the condition under which the rate of drug administration is equal to the rate of drug elimination in any given period. Drug accumulation to steady state is near-complete in four to five elimination half-lives (see Fig. 9-3). For many drugs, the target molecule is in or readily accessible from plasma, so this time course also describes the development of pharmacologic effects. However, in other cases, whereas steady-state plasma concentrations are achieved in four to five elimination half-lives, steady-state drug effects take longer to achieve and several explanations are possible. First, an active metabolite may need to be generated to achieve drug effects. Second, time may be required for translation of the drug effect at the molecular site to a physiologic endpoint; inhibition of synthesis of vitamin K–dependent clotting factors by warfarin ultimately leads to a desired elevation of the international normalized ratio (INR), but the development of this desired effect occurs only as levels of clotting factors fall. Third, penetration of a drug into intracellular or other tissue sites of action may be required before development of drug effect. One mechanism underlying such penetration is the variable function of specific drug uptake and efflux transport proteins that control intracellular drug concentrations.
Drug Therapeutics and Personalized Medicine
Importance of Correct Drug Use
The Key Decision in Drug Therapy: Risk Versus Benefit
Mechanisms Underlying Variability in Drug Action
Pharmacodynamic Principles
Time Course of Drug Effects

Drug Therapeutics and Personalized Medicine
9