Limited data are available on the use of coronary computed tomographic angiography (CCTA) in patients who have received percutaneous coronary intervention (PCI). To evaluate patterns of cardiac testing including CCTA after PCI, we created a retrospective observational dataset linking National Cardiovascular Data Registry CathPCI Registry baseline data with longitudinal inpatient and outpatient Medicare claims data for patients who received coronary stenting from November 1, 2005 through December 31, 2007. In 192,009 patients with PCI (median age 74 years), the first test after coronary stenting was CCTA for 553 (0.3%), stress testing for 89,900 (46.8%), and coronary angiography for 22,308 (11.6%); 79,248 (41.3%) had no further testing. Patients referred to CCTA first generally had similar or lower baseline risk than those referred for stress testing or catheterization first. Compared to patients with stress testing first after PCI, patients who underwent CCTA first had higher unadjusted rates of subsequent noninvasive testing (10% vs 3%), catheterization (26% vs 15%), and revascularization (13% vs 8%) within 90 days of initial testing after PCI (p <0.0001 for all comparisons). In conclusion, despite similar or lesser-risk profiles, patients initially evaluated with CCTA after PCI had more downstream testing and revascularization than patients initially evaluated with stress testing. It is unclear whether these differences derive from patient selection, performance of CCTA compared to other testing strategies, or the association of early adoption of CCTA with distinct patterns of care.
We analyzed the use of diagnostic methods for coronary artery disease (CAD) after coronary stent implantation in Medicare fee-for-service beneficiaries using a combined dataset comprised of inpatient and outpatient claims from the Centers for Medicare & Medicaid Services and data from the National Cardiovascular Data Registry Catheter PCI (CathPCI) Registry. Our aim was to provide insight into emerging patterns of testing with computed coronary tomographic angiography (CCTA) compared to alternative testing options in patients after percutaneous coronary intervention (PCI) procedures from 2005 through 2007 and the association of initial test choice with downstream testing and procedures including subsequent catheterization and revascularization.
Methods
The Duke University Medical Center institutional review board granted a waiver of informed consent and authorization for this study, and all analyses were conducted by the Duke Clinical Research Institute.
PCI cases were drawn from the CathPCI Registry—a large national registry of patients who have received diagnostic cardiac catheterization or PCI. Initially we identified patients ≥65 years of age who received PCI with stenting and who were admitted and discharged from January 2004 through December 2008. The first PCI procedure with stent for each admission was considered the index event and was the initial unit of analysis. Initially there were 672,617 eligible index events from the CathPCI Registry. Index PCI events were linked to Medicare inpatient claims data from 2004 through 2008 using an established method. We successfully linked 67% of all eligible index events to an admission in the Centers for Medicare & Medicaid Services data. The resulting match allowed identification of subsequent resource use in Centers for Medicare & Medicaid Services inpatient, outpatient, and physician claims files.
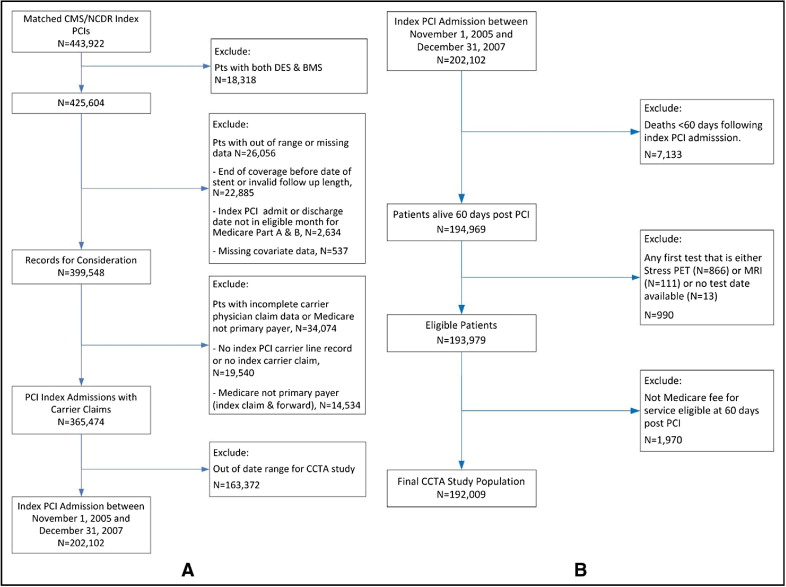
Some exclusion criteria were applied to define the final study population including limiting the cohort for the present study to those with PCI from November 1, 2005 through December 31, 2007 to account for changes in coding for CCTA and to allow for ≥1 year of potential follow-up as detailed in Figure 1 . We defined a 60-day black-out period after PCI for each patient during which tests or procedures were not considered in the final study analysis because these tests and procedures may have been performed for cardiac rehabilitation, staging of procedures, or functional capacity assessments. Patients were excluded if they died or did not retain Part A and Part B Medicare coverage during this black-out period.
Numbers and dates of noninvasive cardiac stress tests and procedures after index PCI were identified by Current Procedural Technology and Healthcare Common Procedure Coding System codes (electrocardiographic stress, 93015 to 93018; nuclear, 78460, 78461, 78464, 78465, 78472, 78473, 78481, 78483; positron emission tomography, 78491, 78492; stress echocardiography, 93350; CCTA, 0146T to 0149T). We stratified patients based on the type of the first diagnostic test they received after their coronary stenting (after a 60-day black-out period). Numbers and dates of repeat catheterizations and coronary revascularizations (PCI or coronary artery bypass grafting) after PCI were identified using Current Procedural Technology, International Classification of Diseases, Ninth Revision, Clinical Modification , and Healthcare Common Procedure Coding System codes (catheterization, 93508, 93539, 93540, 93545; PCI, 92980 to 92982, 92984, 92995, 92996, G0290, G0291, 36.01, 36.02, 36.05, 36.06, 36.07, 00.66; coronary artery bypass grafting, 33510 to 33514, 33516 to 33519, 33521 to 33523, 33533 to 33536, 36.1x, 36.2, S2205 to S2209).
Demographic, clinical, and hospital baseline characteristics for patients at time of index PCI were analyzed overall and by type of initial test (if any) performed after coronary stenting at any time during the study period using descriptive statistics (number of observations, mean ± SD, median, 25th and 75th percentiles, minimum, and maximum) for numerical (or continuous) variables and with frequency and percentage for categorical variables. All statistical tests were 2-sided with a significance level of 0.05. The p values were based on Pearson chi-square tests for categorical variables or Kruskal–Wallis tests for continuous or ordinal variables.
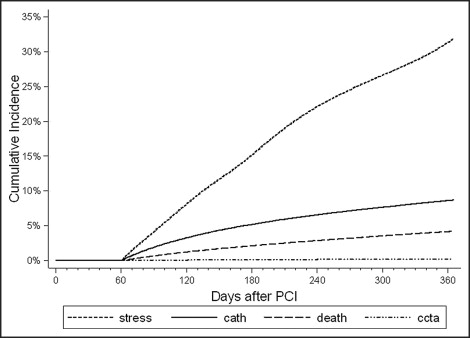
Using cumulative incidence functions that accounted for administrative censoring and included death as a competing risk, we computed and plotted time to first test (e.g., CCTA, stress test, or catheterization) occurring ≥60 days and up to 1 year after the index revascularization episode. Cumulative incidence across groups was compared using the method of Gray.
One-year cumulative incidence rates were used to evaluate quarterly time trends for first noninvasive cardiac test or invasive coronary angiography after coronary stenting. We used an unadjusted Poisson regression model to determine the significance of quarterly trends.
To evaluate patterns of “layered” testing after PCI, we calculated rates of invasive and noninvasive testing and procedures conditional on the initial test after PCI (e.g., CCTA first, stress test first, catheterization first, or no subsequent test). We identified subsequent procedures (e.g., CCTA next, stress test next, any catheterization, any revascularization, or no subsequent procedure) occurring within a 90-day “episode-of-care” window after the initial cardiac test after PCI and calculated rates of additional noninvasive testing, diagnostic catheterization, and coronary revascularization after initial testing after PCI. “Catheterization yield” rates were defined as the number of patients undergoing coronary revascularization within 90 days of the initial test after PCI divided by the number of patients undergoing catheterization procedures within the same period.
Time trends of invasive and noninvasive testing and procedures within 90 days after CCTA as the first test after PCI were evaluated by date of CCTA in 1/2-year increments to assess whether downstream care patterns after CCTA varied with time. Analysis was limited to patients with 90 days of follow-up after CCTA. Patients with CCTA from January 1, 2006 through June 30, 2006 were excluded because of very small numbers. An unadjusted negative binomial regression model was used to determine the significance of time trends.
All statistical analyses were conducted using SAS 9.2 or higher (SAS Institute, Cary, North Carolina) and STATA 11 (STATA Corp., College Station, Texas).
Results
The study population consisted of 192,009 fee-for-service Medicare beneficiaries undergoing stent implantation from November 1, 2005 through December 31, 2007, with follow-up from January 1, 2006 through December 31, 2008 ( Figure 1 ). Median duration of follow-up was 705 days (interquartile range 516 to 917). Overall, during the entire study period, 553 patients (0.3%) had CCTA as their first test ≥60 days after coronary stenting. In contrast, 89,900 patients (46.8%) had a stress test (stress nuclear, stress echocardiography, or exercise treadmill test) as their first test, 22,308 patients (11.6%) underwent coronary angiography as their first test, and 79,248 patients (41.3%) had no cardiac testing after index PCI ( Table 1 ).
| Characteristic | Overall | CCTA First | Stress Test First | Catheterization First | No Testing |
|---|---|---|---|---|---|
| (n = 192,009) | (n = 553) | (n = 89,900) | (n = 22,308) | (n = 79,248) | |
| Baseline demographics and co-morbid conditions | |||||
| Age (years) | 74 (69–80) | 73 (69–78) | 73 (69.78) | 74 (69.79) | 76 (70–80) |
| ≥75 years | 49% | 42% | 44% | 47% | 55% |
| Women | 43% | 42% | 42% | 45% | 43% |
| White race | 89% | 91% | 89% | 89% | 89% |
| Body mass index | 28 (25–31) | 28 (25–31) | 28 (25–32) | 28 (25–32) | 27 (24–31) |
| ≥30 kg/m 2 | 33% | 32% | 34% | 35% | 32% |
| Previous myocardial infarction (>7 days) | 24% | 23% | 22% | 30% | 25% |
| Previous heart failure | 13% | 10% | 10% | 16% | 16% |
| Hypertension | 81% | 77% | 81% | 84% | 81% |
| Diabetes mellitus | 32% | 28% | 31% | 37% | 33% |
| Renal failure (glomerular filtration rate <30 ml/min or dialysis) | 4% | 2% | 3% | 5% | 5% |
| Cerebrovascular disease | 16% | 16% | 14% | 18% | 17% |
| Peripheral vascular disease | 15% | 15% | 13% | 18% | 16% |
| Chronic lung disease | 18% | 20% | 16% | 21% | 20% |
| Dyslipidemia ⁎ | 74% | 78% | 76% | 77% | 72% |
| Current smoker | 12% | 11% | 11% | 13% | 14% |
| Previous percutaneous coronary intervention | 27% | 34% | 26% | 36% | 24% |
| Previous coronary bypass | 22% | 25% | 21% | 31% | 21% |
| Cardiac status | |||||
| Presenting symptoms | |||||
| No angina pectoris | 14% | 10% | 15% | 11% | 14% |
| Atypical chest pain | 8% | 8% | 8% | 7% | 7% |
| Stable angina pectoris | 16% | 21% | 18% | 16% | 14% |
| Unstable angina pectoris | 34% | 44% | 34% | 41% | 32% |
| Non–ST-segment elevation myocardial infarction | 17% | 11% | 14% | 16% | 20% |
| ST-segment elevation myocardial infarction | 11% | 6% | 10% | 9% | 13% |
| Heart failure | 12% | 11% | 9% | 13% | 15% |
| Procedural characteristics | |||||
| Drug-eluting stent used | 74% | 78% | 77% | 73% | 70% |
| Stent diameter (mm) | 3.0 (2.5–3.5) | 3.0 (2.75–3.5) | 3.0 (2.5–3.5) | 3.0 (2.5–3.5) | 3.0 (2.5–3.5) |
| Mean stent diameter (mm) | 2.98 | 3.04 | 2.97 | 2.99 | 2.98 |
| Stent diameter <3 mm | 40% | 34% | 41% | 40% | 40% |
| Time to first test (days) | 245 (140–396) | 251 (142–412) | 255 (150–400) | 204 (112–366) | |
| Duration of follow-up † (days) | 705 (516–917) | 734 (555–930) | 775 (587–960) | 726 (539–933) | 622 (449–835) |
| Hospital features | |||||
| Centers for Medicare & Medicaid Services–certified beds | 421 (300–569) | 424 (275–585) | 411 (294–570) | 424 (300–568) | 424 (303–571) |
| Urban location | 60% | 65% | 59% | 61% | 60% |
| Region | |||||
| Northeast | 11% | 4% | 12% | 9% | 11% |
| Midwest | 35% | 30% | 34% | 36% | 36% |
| South | 39% | 58% | 39% | 42% | 39% |
| West | 14% | 9% | 15% | 12% | 14% |
| Hospital profit type | |||||
| Community/private | 89% | 90% | 90% | 89% | 88% |
| Academic | 51% | 42% | 50% | 52% | 53% |
| Annual percutaneous coronary intervention volume | 877 (560–1482) | 843 (550,1526) | 875 (558–1517) | 921 (601–1562) | 872 (553–1444) |
⁎ Dyslipidemia diagnosed and/or treated by a physician, defined according to the National Cardiovascular Data Catheter Percutaneous Coronary Intervention Registry data collection-form criteria: (1) total cholesterol >200 mg/dl, or (2) low-density lipoprotein ≥130 mg/dl, or (3) high-density lipoprotein <30 mg/dl, or (4) admission cholesterol >200 mg/dl, or (5) triglycerides >150 mg/dl, or (6) treatment was initiated because low-density lipoprotein was >100 mg/dl (2.59 mmol/L) in patients with known coronary artery disease.
The 553 CCTAs completed as first tests after PCI were performed at 199 sites, with tests per site ranging from 1 to 33 (median 1, interquartile range 1 to 3); 106 sites performed only 1 study (106 total studies, 19%), 85 sites performed 2 to 9 studies (292 total studies, 53%), and 8 sites performed ≥10 studies (155 total studies, 28%).
Patients with CCTA as their first test after coronary stenting differed at baseline from the overall study population (p <0.0001 for all comparisons; Table 1 ). In general, patients referred for CCTA first after coronary stenting had lower rates of most risk factors and co-morbidities compared to patients referred to cardiac catheterization first and compared to patients who did not receive further cardiovascular testing during the study period.
Compared to only those patients referred for stress testing first, patients referred to CCTA had clinically similar rates (within 2%) of most baseline characteristics, cardiac risk factors, and co-morbidities evaluated. Patients with CCTA had modestly lower rates of hypertension and diabetes but higher rates of chronic lung disease. At time of index PCI, patients with CCTA had higher rates of previous revascularization but were less likely to have presented with myocardial infarction (or no angina). Patients who received CCTA first had received on average slightly larger stents (mean diameter 3.04 vs 2.97 mm, interquartile range 2.75 to 3.5 vs 2.5 to 3.5) during index PCI and were less likely to have received stents <3.0 mm in diameter.
Over the study interval, rate of using CCTA as the first test within 1 year after coronary stenting was 0.19% (proportion of patients with CCTA first at any time during follow-up [median 734 days] was 0.3%; Figure 2 ). This rate increased over time, from 0.13% for patients with PCI in the fourth quarter of 2005 to 0.23% in the fourth quarter of 2007. Over the same period, stress testing first decreased from 34.7% to 30.7%, coronary angiography first increased from 8.6% to 9.0%, and the rate of no subsequent cardiac testing increased from 56.6% to 60.0% ( Table 2 ).
| Total Population (n = 192,009) | 2005 Q4 | 2006 | 2007 | Rate Ratio/Q | p Value ⁎ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||||
| Coronary computed tomographic angiography (n = 365) | 0.13% | 0.13% | 0.17% | 0.19% | 0.19% | 0.22% | 0.17% | 0.24% | 0.23% | 1.043 | 0.03 |
| Stress test (n = 61,411) | 34.7% | 32.8% | 33.6% | 32.2% | 32.2% | 30.5% | 31.6% | 31.1% | 30.7% | 0.993 | 0.03 |
| Catheterization (n = 16,721) | 8.6% | 8.5% | 8.7% | 8.2% | 8.6% | 8.8% | 9.0% | 8.9% | 9.0% | 1.007 | 0.002 |
| None (n = 113,512) | 56.6% | 58.5% | 57.5% | 59.4% | 59.0% | 60.6% | 59.2% | 59.8% | 60.0% | 1.003 | 0.17 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


