INDICATIONS/CONTRAINDICATIONS
Lung transplantation is the established surgical treatment modality for end-stage parenchymal and vascular nonmalignant lung diseases. The International Society for Heart and Lung Transplantation (ISHLT) maintains the largest registry worldwide, which covers more than 3,000 transplants annually. The most common indication for lung transplantation has been chronic obstructive pulmonary disease (COPD) for a long time and still represents 34% of the overall worldwide transplant activity. With the introduction of new allocation algorithms such as the Lung Allocation Score (LAS) the percentage of patients transplanted for idiopathic pulmonary fibrosis (IPF) has risen. Cystic fibrosis is the third main indication for lung transplantation. The number of patients with pulmonary arterial hypertension undergoing transplantation has decreased and the preferred type of transplantation is nowadays bilateral lung transplantation. Bronchiectasis, sarcoidosis, retransplantation, connective tissue disease, lymphangioleiomyomatosis, and congenital heart disease are less common indications for lung transplantation.
The percentage of bilateral procedures is constantly increasing and has reached more than 70% of all lung transplant procedures worldwide. In our own center the percentage of bilateral procedures represent more than 90% of the overall lung transplant volume.
The background for this strategy can be found in the persistent survival benefit of bilateral lung recipients compared to single lung recipients. Although a selection bias might play a role in obtaining these superior results, the survival benefit is reproducible in the ISHLT database among patients with different diagnoses and different age groups (Fig. 3.1).
Advanced operative techniques of bilateral transplantation with special importance for pediatric recipients include lobar transplantation or split lung transplantation, which however, should be performed in specialized centers only. In addition, living-related lung donation can be another technical option for bilateral transplantation in selected patients.
There are few absolute contraindications, however, a number of relative contraindications, which vary center wise according to different individual experiences and differences in the availability of donor organs. Absolute contraindications are: Significant systemic diseases, severe extrapulmonary organ dysfunctions, recent malignancies, HIV infection, hepatitis B or C, pan-resistant MRSA or Burkholderia cepacia, active nicotine, and alcohol or drug abuse.
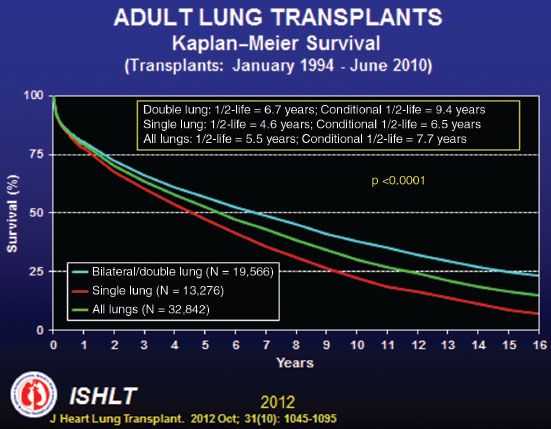
Figure 3.1 ISHLT Registry Slide showing Kaplan–Meier survival for single versus double lung transplantation.
The large number of relative contraindications must be individually judged from case to case: Osteoporosis, muscular or skeletal diseases, extreme cachexy or obesity, long-time corticosteroid therapy, infection with mycobacteria, coronary disease or left ventricular dysfunction, significant peripheral vascular disease, renal insufficiency, severe chest wall deformity, and psychosocial instability.
Pretransplant mechanical ventilation or extracorporeal support was initially considered a contraindication to lung transplantation. However, nowadays new allocation policies and the availability of innovative bridging options allow a safe bridge to lung transplantation in selected patients. The current trend is to keep patients as ambulatory as possible on the device.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
The optimal time for listing for lung transplantation is at a stage when survival expectancy with lung transplantation exceeds the survival expectancy without transplantation and the patient is still in a condition to survive the expected waiting period. This implies that the timing of referral and listing for lung transplantation are not only based on recipient factors, but also have to take the organ availability and the allocation system into account. Allocation algorithms vary substantially in different countries. While algorithms based on waiting time only uniformly led to high waiting list mortality and have been abandoned by most countries, nowadays allocation algorithms using the LAS— which takes the expected waiting list mortality and the anticipated 1-year post-transplant survival into account—or center-based allocation are the most common systems in use.
 SURGERY
SURGERY
Positioning
The patient is positioned supine for bilateral lung transplantation with abducted arms and the chest is elevated by inflatable cushions (Fig. 3.2). The entire chest with either one or both groins is scrubbed in the sterile field. This provides access for the thoracic incision as well as for femoral cannulation if required. In this position no additional femoral arterial line to aid in blood pressure monitoring is usually required.

Figure 3.2 Standard position of the recipient for bilateral lung transplantation.
Approach
Standard approach to the chest for bilateral lung transplantation is usually the so-called clamshell incision, which combines a bilateral thoracotomy with a transverse sternotomy and ligation of the internal thoracic vessels (Fig. 3.3) and can also be gained by two separate thoracotomies (Fig. 3.4). Some centers also use a median sternotomy, which however, limits access to the posterior hilum.
In patients with separate bilateral thoracotomies the standard approach on the right side is the fourth intercostal space, which provides excellent access to all hilar structures and gives the opportunity for central cannulation for cardiopulmonary bypass (CPB) or extracorporeal membrane oxygenation (ECMO) whenever necessary. The serratus anterior muscle is divided, while the latissimus dorsi can be left untouched. It is important to open the intercostal muscles from just posterior of the internal thoracic artery to the posterior end of the rib to allow full spreading of the intercostal space without causing rib fractures. On the left side it can be beneficial to choose the fifth intercostal space to facilitate exposure of the left atrium.
The clamshell incision provides the best exposure to both hili and the heart, especially when central cannulation for extracorporeal support is required. The decision whether to use separate incisions or a clamshell incision is based on the individual anatomic situation, especially the size of the recipient chest cavity, the extent of adhesions and whether intraoperative extracorporeal support will be required.
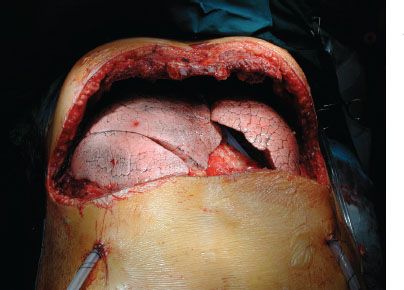
Figure 3.3 Approaches for bilateral transplantation—anterolateral thoracotomy.
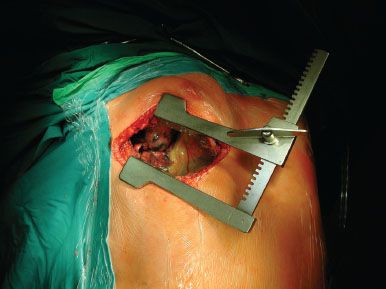
Figure 3.4 Approaches for bilateral transplantation—clamshell incision.
Technique
Intubation is routinely performed with a left-sided double-lumen tube to allow unilateral ventilation. The choice, which lung is transplanted first depends on donor and recipient issues. The preoperative recipient V/Q scan is an important tool in this decision process. Usually the functionally worse side is transplanted first if the procedure is planned without the use of extracorporeal support. In case of a quality difference between the donor lungs, for example, due to traumatic alterations or other minor impairments, the better lung will be transplanted first. The implantation is performed in a sequential technique.
Recipient pneumonectomy is performed in standard fashion with stapling of the pulmonary artery and pulmonary veins. The bronchus is prepared centrally and opened with a scalpel. Two polydioxanone 4-0 stay sutures are placed at the angles between the cartilaginous and the membranous portion. Thereafter the lung is removed from the chest cavity and the pericardium is opened between the superior pulmonary vein and the phrenic nerve and circumferentially dissected to fully mobilize the left atrium. Thereafter, the pulmonary artery is prepared intrapericardially as central as possible to provide sufficient length for the anastomosis (Fig. 3.5). Once the intrapericardial dissection is completed the posterior mediastinum can be closed with a running PDS 4-0 suture to prevent bleeding from lymph nodes in this area, which is difficult to control after the lung has been implanted. Meticulous hemostasis has to be performed before beginning with the implantation.
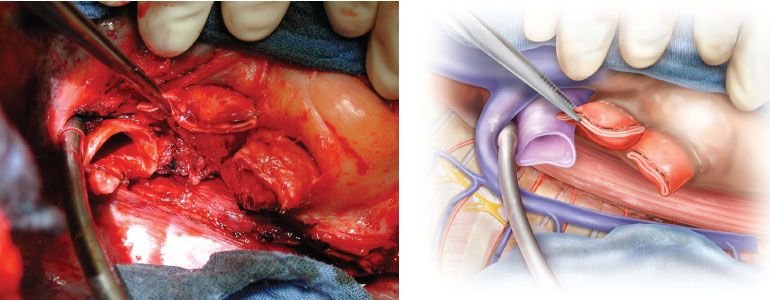
Figure 3.5 Right hilum after intrapericardial preparation of the vessels.
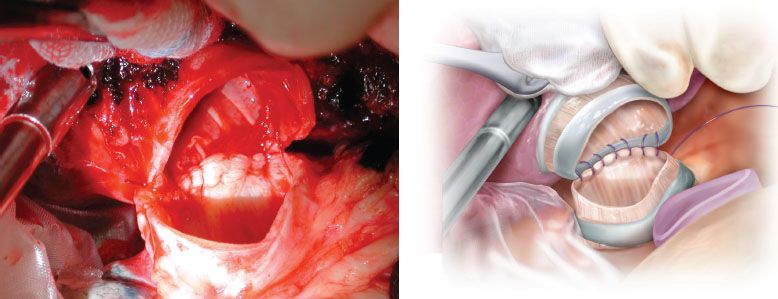
Figure 3.6 Bronchial anastomosis using the single running suture technique.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


